Applied Anatomy of the Superficial Branch of the Radial Nerve
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Radiohamate Impingement After Proximal Row Carpectomy ‘Radiohamate Impingement PRC’
Acta Orthop. Belg., 2020, 86 e-supplement 1, 19-21 CASE REPORT Radiohamate impingement after proximal row carpectomy ‘Radiohamate impingement PRC’ Pieter Caekebeke, Luc De Smet From the Department of Orthopaedics UZ Leuven, Pellenberg, Belgium Radiocarpal impingement after PRC is a well-known from 0% to 18% (5). Radiocarpal and pisiform complication due to impingement of the radial styloid impingement have been described after PRC. The against the radial carpal bones. A less common first is probably due to the proximalization of the impingement syndrome is that of the pisiforme. distal row with impingement of the trapezium/ We describe a radiohamate impingement and its trapezoid against the radial styloid process. The diagnosis and treatment. Based on a case we saw treatment is a radial styloid process resection for at our practice. Diagnosis is bases on standard radiographs and SPECT-CT. The treatment is the first and a pisiformectomy for the latter (3,5). No initially conservative. Surgery is necessary when other impingement syndromes have been described. conservative treatment fails and consists of resectie We present a case of radiohamate impingement of the proximal pole of the hamate. syndrome after proximal row carpectomy. Keywords: Radiohamate ; impingement ; proximal row CASE REPORT carpectomy. A 53-year-old mechanic contacted us 1 year after a work-accident with localized radiocarpal INTRODUCTION pain and swelling. Radiographs showed a stage Proximal row carpectomy (PRC) is a well- two SLAC wrist. (Fig. 1) A PRC with synovectomy established motion-preserving salvage procedure was performed. The following 3 years were for degenerative disorders of the proximal carpal uneventful with no to minimal pain complaints. -
Shoulder Shoulder
SHOULDER SHOULDER ⦿ Connects arm to thorax ⦿ 3 joints ◼ Glenohumeral joint ◼ Acromioclavicular joint ◼ Sternoclavicular joint ⦿ https://www.youtube.com/watch?v=rRIz6oO A0Vs ⦿ Functional Areas ◼ scapulothoracic ◼ scapulohumeral SHOULDER MOVEMENTS ⦿ Global Shoulder ⦿ Arm (Shoulder Movement Joint) ◼ Elevation ◼ Flexion ◼ Depression ◼ Extension ◼ Abduction ◼ Abduction ◼ Adduction ◼ Adduction ◼ Medial Rotation ◼ Medial Rotation ◼ Lateral Rotation ◼ Lateral Rotation SHOULDER MOVEMENTS ⦿ Movement of shoulder can affect spine and rib cage ◼ Flexion of arm Extension of spine ◼ Extension of arm Flexion of spine ◼ Adduction of arm Ipsilateral sidebending of spine ◼ Abduction of arm Contralateral sidebending of spine ◼ Medial rotation of arm Rotation of spine ◼ Lateral rotation of arm Rotation of spine SHOULDER GIRDLE ⦿ Scapulae ⦿ Clavicles ⦿ Sternum ⦿ Provides mobile base for movement of arms CLAVICLE ⦿ Collarbone ⦿ Elongated S shaped bone ⦿ Articulates with Sternum through Manubrium ⦿ Articulates with Scapula through Acromion STERNOCLAVICULAR JOINT STERNOCLAVICULAR JOINT ⦿ Saddle Joint ◼ Between Manubrium and Clavicle ⦿ Movement ◼ Flexion - move forward ◼ Extension - move backward ◼ Elevation - move upward ◼ Depression - move downward ◼ Rotation ⦿ Usually movement happens with scapula Scapula Scapula ● Flat triangular bone ● 3 borders ○ Superior, Medial, Lateral ● 3 angles ○ Superior, Inferior, Lateral ● Processes and Spine ○ Acromion Process, Coracoid Process, Spine of Scapula ● Fossa ○ Supraspinous, Infraspinous, Subscapularis, Glenoid SCAPULA -

De Quervain's Release Standard of Care PT
BRIGHAM & WOMEN’S HOSPITAL Department of Rehabilitation Services Physical Therapy Standard of Care: de Quervain’s Syndrome: Surgical Management Physical Therapy management of the patient who had a release of the first extensor compartment. Case Type/Diagnosis: (diagnosis specific, impairment/dysfunction specific) 11 Since the first description of “washerwoman’s sprain” tenosynovitis of the first dorsal compartment has become a commonly recognized inflammatory disorder. The most radial of the extensor compartments on the dorsum of the wrist is occupied by the tendons of the extensor pollicis brevis and abductor pollicis longus. The tendons are enveloped in an osseofibrous canal lined by synovium, which, when subjected to excessive or repetitive mechanical stresses, responds in a characteristic fashion distinguished by pain, swelling, and limitation of motion of the thumb. In 1895,Fritz de Quervain, a Swiss surgeon, 1 was first credited with the recognition of this disease and so it bore his name. More accurately, Tillaux 2 and Gray 3 referred to this disorder before de Quervain. Anatomy: Twenty-four extrinsic tendons cross the wrist and provide power and dexterity in the hand. Each tendon passes through a series of tight fibrous -osseous canals designed to optimize the balance between motion and force production by maintaining the tendon in close approximation to the joint or joints it controls. There are six separate compartments under the dorsal carpal ligament each lined with a separate synovial sheath membrane. The first one is over the radial styloid and it contains the abductor pollicis longus and the extensor pollicis brevis tendons. These tendons pass through an unyielding osteoligamentous tunnel formed by a shallow groove in the radial styloid process and a tough overlying roof composed by the transverse fibers of the dorsal ligament. -

Unilateral Os Radiostyloideum Presenting with Degenerative
Scholars Journal of Applied Medical Sciences (SJAMS) ISSN 2320-6691 (Online) Sch. J. App. Med. Sci., 2014; 2(6A):1997-1999 ISSN 2347-954X (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Case Report Unilateral Os Radiostyloideum Presenting with Degenerative Changes and Wrist Pain in an Elderly Male: A Case Report Puneet Gupta1*, Manik Mahajan2, Rajesh Sharma1, Poonam sharma3 1Department of Radio-diagnosis and Imaging, ASCOMS Hospital, Sidhra, Jammu (J&K), India 2Department of Radio-diagnosis and imaging, PGIMS, Rohtak 3Department of pathology, GMC, Jammu (J&K), India *Corresponding author Puneet gupta Email: Abstract: Accessory carpal bones are rare findings and are mostly discovered as an incidental finding when radiographs are obtained for some other purpose. Herein we report a case of Os radiostyloideum in a 56-year-old male patient, who presented with chronic left wrist pain. Keywords: Carpal, Wrist, Ossicles. INTRODUCTION of scaphoid, showing normal trabecular pattern (Fig. Accessory bones, or ossicles, are considered to be 1A). A prospective diagnosis of Os Radiostyloideum normal anatomic variants. Accessory ossicles are was made. Patient was advised a non- contrast CT scan secondary ossification centres that are distinct from the of the left wrist for further evaluation. CT scan revealed associated underlying bone. Although generally thought the presence of a well defined, small, rounded bone to be congenital in origin, occasionally a posttraumatic with distinct trabecular pattern and peripheral cortex or degenerative etiology may be considered if supported distal and lateral to the radial head without any by patient history or correlative findings [1]. -
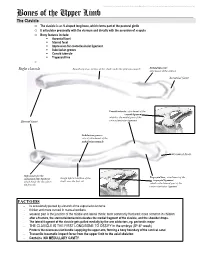
Bones of the Upper Limb
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. Bones of the Upper Limb The Clavicle o The clavicle is an S-shaped long bone, which forms part of the pectoral girdle o It articulates proximally with the sternum and distally with the acromion of scapula o Bony features include: . Acromial facet . Sternal facet . Impression for costoclavicular ligament . Subclavian groove . Conoid tubercle . Trapezoid line o Right clavicle Smooth superior surface of the shaft, under the platysma muscle Deltoid tubercle: attachment of the deltoid Acromial facet Conoid tubercle, attachment of the conoid ligament which is the medial part of the Sternal facet coracoclavicular ligament Subclavian groove: site of attachment of the subclavius muscle Acromial facet Impression for the Trapezoid line, attachment of the costoclavicular ligament Rough inferior surface of the trapezoid ligament which binds the clavicle to shaft, over the first rib which is the lateral part of the the first rib coracoclavicular ligament FACTOIDS - Its occasionally pierced by a branch of the supraclavicular nerve - thicker and more curved in manual workers - weakest part is the junction of the middle and lateral thirds: most commonly fractured; more common in children - after a fracture, the sternocleidomastoid elevates the medial fragment of the clavicle, and the shoulder drops. - The lateral fragment of the clavicle gets pulled medially by the arm adductors, eg. pectoralis major - THE CLAVICLE IS THE FIRST LONG BONE TO OSSIFY in the embryo (5th-6th week) - Protects the neurovascular bundle supplying the upper arm, forming a bony boundary of the cervical canal - Transmits traumatic impact force from the upper limb to the axial skeleton - Contains NO MEDULLARY CAVITY - This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. -

Stress Fracture of the Radial Styloid Process in a Judo Player: a Case Report
―Case Reports― Stress Fracture of the Radial Styloid Process in a Judo Player: A Case Report Hiroshi Hashiguchi1, Satoshi Iwashita1,AtsushiOhkubo1, Takuya Sawaizumi2 and Shinro Takai2 1Department of Orthopaedic Surgery, Nippon Medical School Chiba Hokusoh Hospital 2Department of Orthopaedic Surgery, Nippon Medical School Stress fractures of the upper limbs are uncommon, and are most often reported as individual cases or small series. In particularly, stress fractures around the wrist are even less common. A stress fracture of the radial styloid process in a judo player was surgically treated, and a favorable treatment outcome was obtained. A 16-year-old adolescent boy experienced pain in the right wrist, with no apparent trig- ger, while playing judo. Stress fracture of the radial styloid process was diagnosed with plain radio- graphs and was treated conservatively with cast immobilization. Although bone union was achieved, the fracture recurred after he resumed paying judo. Thus, surgical treatment was performed. The proce- dure was resection of the distal bone fragment. He resumed practicing 2 months postoperatively and returned to judo matches after 1 more month. As of 1 year after distal bone fragment resection, he was able to participate in judo without pain, limited range of motion, or instability of the wrist. (J Nippon Med Sch 2015; 82: 109―112) Key words: stress fracture, radial styloid process, sports injury Introduction curred with dorsiflexion of the wrist. Tenderness was In athletes, stress fractures are thought to be caused by noted on the radial styloid process. Grip strength was repetitive stress applied to a structure, as in running and 29.8 kg on the right and 36.4 kg on the left. -

SOME COMPLICATIONS of COLLES' FRACTURE and THEIR TREATMENT by W
Postgrad Med J: first published as 10.1136/pgmj.27.314.627 on 1 December 1951. Downloaded from 627 SOME COMPLICATIONS OF COLLES' FRACTURE AND THEIR TREATMENT By W. H. STEPHENSON, F.R.C.S. From the Department of Surgery, Postgraduate Medical School of London, Hammersmith Hospital Though Colles' fracture is a common injury its other positions has been tried, such as the Cotton complications and their treatment are seldom Loder (full palmar-flexion of the wrist and ulnar dealt with in surgical papers. In this paper it is deviation with extreme pronation of the forearm), proposed to discuss the following complications: but no position is completely successful in pre- I. Redisplacement. venting redisplacement. Protected by copyright. 2. Mal-union. Gross comminution may be seen in all age 3. Laxity of the inferior radio-ulnar joint. groups but is more commonly observed in the 4. Joint stiffness and adhesions. elderly. Comminution means instability, and even 5. Traumatic arthritis of the wrist joint. with the best support redisplacement is therefore 6. Pain over the ulnar aspect of the wrist. always a possibility. 7. Late rupture of the extensor pollicis longus Compression of bone on the dorsal aspect of the tendon. fracture is the direct result of the causative force. 8. Sudeck's atrophy (post-traumatic osteo- In some instances it is so well marked that after dystrophy). good reduction has been obtained a distinct gap 9. Injuries of the median nerve. may be seen dorsally between the fracture surfaces io. Prolonged absence from work. in the lateral radiograph. I. Redisplacement Treatment This is the commonest complication of im- Minor degrees of malalignment may be accepted portance. -

Anatomy Lab: the Skeletal System Part I: Vertebrae and Thoracic Cage
ANA Lab: Bone 1 Anatomy Lab: The skeletal system Part I: Vertebrae and Thoracic cage Spine (Vertebrae) Body Vertebral arch Vertebral canal Pedicle Lamina Spinous process Transverse process Sup. articular facets Inf. articular facets Sup. vertebral notch Inf. vertebral notch Intervertebral foramen Cervical vertebrae: 7 Typical (C3-C6) Transverse foramen C1, Atlas C2, Axis: dens C7 Thoracic vertebrae: 12 Typical (T2-T10) T1 T11, 12 Lumbar vertebrae: 5 Typical (L1-4) Sacrum: 5 Ala Anterior sacral foramina Posterior sacral foramina Sacral canal ANA Lab: Bone 2 Sacral hiatus promontory median sacral crest intermediate crest lateral crest Coccyx Horns Transverse process Thoracic cages Ribs: 12 pairs Typical ribs (R3-R10): Head, 2 facets intermediate crest neck tubercle angle costal cartilage costal groove R1 R2 R11,12 Sternum Manubrium of sternum Clavicular notch for sternoclavicular joint body xiphoid process ANA Lab: Bone 3 Part II: Skull and Facial skeleton Skull Cranial skeleton, Calvaria (neurocranium) Facial skeleton (viscerocranium) Overview: identify the margin of each bone Cranial skeleton 1. Lateral view Frontal Temporal Parietal Occipital 2. Cranial base midline: Ethmoid, Sphenoid, Occipital bilateral: Temporal Viscerocranium 1. Anterior view Ethmoid, Vomer, Mandible Maxilla, Zygoma, Nasal, Lacrimal, Inferior nasal chonae, Palatine 2. Inferior view Palatine, Maxilla, Zygoma Sutures: external view vs. internal view Coronal suture Sagittal suture Lambdoid suture External appearance of skull Posterior view external occipital protuberance -

Distal Radius Surgical Technique
DISTAL RADIUS SURGICAL TECHNIQUE 3-DIMENSIONAL FRACTURE MANAGEMENT SYSTEM 1 TABLE OF CONTENTS Radial Technique Room Configuration and Patient Prep ..................................3 1 Reduction and Provisional Fixation .......................................3 2 Target Wire and Template .....................................................4 Cage Size ......................................................................4 Access Marking .............................................................4 3 Access — Incision ..................................................................5 Access — 2.5 mm Side Cut Drill ...................................5 4 Access — Guide Pin and 5.0 mm Drill ..................................6 5 Cavity Preparation .................................................................6 6 Cage Delivery and Locking ..................................................7 Cage Locking ................................................................7 7 Proximal Plate Application ....................................................8 8 Distal Fragment Fixation — Guide Wires ..............................8 Radial Side Suggestion .................................................9 Distal Fragment Fixation — 2.0 mm Drill ......................9 Ulnar Side Suggestion ...................................................9 Ulnar Side Volar Fragment Suggestion .........................9 9 Secure Fragments ...............................................................10 10 Confirm Anatomic Reconstruction and Remove K-Wires ....10 Post -

Radiographic Evaluation of the Wrist: a Vanishing Art Rebecca A
Radiographic Evaluation of the Wrist: A Vanishing Art Rebecca A. Loredo, MD,* David G. Sorge, MD, Lt. Colonel,† and Glenn Garcia, MD‡ he intricate anatomy and compartmentalization of struc- interpretation of standard or MR arthrograms and for identi- Ttures in the wrist are somewhat daunting. As in other joints, fying various patterns of arthritic involvement.2 The com- the radiographic appearance of disease processes affecting the partments are as follows: wrist is very much dependent on the articular and periarticular soft tissue and osseous anatomy. Therefore, abbreviated discus- 1. Radiocarpal compartment sions of the pertinent anatomy are included within the introduc- 2. Midcarpal compartment tion with more specific anatomic discussions within the text as a 3. Pisiform-triquetral compartment prelude to certain conditions affecting the wrist. 4. Common carpometacarpal compartment 5. First carpometacarpal compartment 6. Intermetacarpal compartments Anatomy of the Wrist 7. Inferior (distal) radioulnar compartment Osseous Anatomy In daily clinical practice, the most important compart- The osseous structures of the wrist are the distal portions of the ments are the radiocarpal, midcarpal, and distal radioulnar radius and ulna, the proximal and distal rows of carpal bones, compartments. The radiocarpal compartment (Fig. 2) lies and the bases of the metacarpals (Fig. 1). The proximal row of between the proximal carpal row and the distal radius and carpal bones consists of the scaphoid, lunate, triquetrum, and the triangular fibrocartilage, which is fibrocartilaginous tis- the pisiform. The distal row of carpal bones contains the trape- sue that extends from the ulnar side of the distal aspect of the zium, trapezoid, capitate, and hamate bones. -
Bones of Upper Limb
BONES OF THE UPPER LIMB Dr. Jamila El-Medany OBJECTIVES At the end of the lecture, students should be able to: List the different bones of the UL. List the characteristic features of each bone. Differentiate between the bones of the right and left sides. List the articulations between the different bones. The Bones of UL are: Pectoral Girdle. Arm : Humerus. Forearm : Radius & Ulna. Wrist : Carpal bones Hand: Metacarpals & Phalanges Pectoral Girdle Formed of Two Bones: Clavicle (anteriorly) and Scapula (posteriorly). It is very light and allows the upper limb to have exceptionally free movement. Clavicle It is a doubly curved long bone lying horizontally across the root of the neck It is subcutaneous throughout its length. Functions: 1. It serves as a rigid support from which the scapula and free upper limb are suspended & keep them away from the trunk so that the arm has maximum freedom of movement. 2. Transmits forces from the upper limb to the axial skeleton. 3. Provides attachment for muscles. 4. It forms a boundary of the Cervicoaxillary canal for protection of the neurovascular bundle of the UL. Clavicle It is a long bone with no medullary cavity. It has the appearance of an elongated letter Capital (S) lying on one side. It has Two Ends: Medial (Sternal) : enlarged & triangular. Lateral (Acromial) : flattened. Body (shaft): Its medial 2/3 is convex forward. Its lateral 1/3 is concave forward. Surfaces: Superior : smooth as it lies just deep to the skin. Inferior : rough because strong ligaments bind it to the 1st rib. Articulations of Clavicle Medially with the manubrium at the Sternoclavicular joint . -

Bones of the Upper Limbs Anatomy Team 434
Bones of The Upper Limbs Anatomy Team 434 Color Index: If you have any complaint or ▪ Important Points suggestion please don’t hesitate to contact us on: ▪ Helping notes [email protected] ▪ Explanation OBJECTIVES ● List the different bones of the UL. ● List the characteristic features of each bone. ● Differentiate between the bones of the right and left sides. ● List the articulations between the different bones. New Terms Term Meaning Example Processes A V-shaped indentation (act as the key of the joint) Coracoid process in the scapula Notch An indentation, (incision) on an edge or surface Radial notch in the ulna A hollow place (The Notch is not complete but the fossa is complete and both of them act as Radial fossa in the humerus Fossa the lock of the joint) Tubercles A nodule or a small rounded projection on a bone Dorsal tubercle in the radius A large prominence on a bone usually serving for the attachment of muscles or ligaments (is a Tibial tuberosity in the tibia Tuberosity bigger projection than the Tubercle) Groove A channel, a long narrow depression sure Intertubercular groove in the humerus Between bones (the place where the two parallel bones attach together by the interosseous Sharp medial interosseous Interosseous border membrane) in the radius The long and narrow upper edge, angle, or crest of something the lateral supracondylar ridge in the femur Ridge Spine Thick projecting ridge of bone Spine of the Scapula Articulation Meeting of two bones to make the joints Any type of joint usually serves as point of attachment for muscles, ligaments, and might form joints Radial styloid process (wrist joint) Styloid process union of scaphoid bone fracture إعادة إلتحام العظام ببعظها عشان ترجع للحالة الطبيعية Union of the bone Bones Process is a bigger projection is a bigger projection .