Radiographic Evaluation of the Wrist: a Vanishing Art Rebecca A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ulna Length and Mid-Upper
Ulna length is an estimation of height. It is not an accurate measure of height Ulna length should be used only when: o It is not possible to measure height or to obtain height by recall OR o Recalled height does not match patients appearance ① To measure ulna length – Complete Women Men this once, on admission Ulna Under 65 years Ulna Under 65 Ensure the patients left arm is bare length 65 & over length 65 years years from palm to elbow (cm) years (cm) & over Ask the patient Approximate Approximate to cross their height (metres) height (metres) left arm across 32.0 1.84 1.84 32.0 1.94 1.87 their chest 31.5 1.83 1.83 31.5 1.93 1.86 (as in this 31.0 1.81 1.81 31.0 1.91 1.84 picture) 30.5 1.80 1.79 30.5 1.89 1.82 30.0 1.79 1.78 30.0 1.87 1.81 Measure between the point of the 29.5 1.77 1.76 29.5 1.85 1.79 elbow (olecranon process) and the 29.0 1.76 1.75 29.0 1.84 1.78 midpoint of the prominent bone of 28.5 1.75 1.73 28.5 1.82 1.76 the wrist (styloid process) 28.0 1.73 1.71 28.0 1.80 1.75 Record ulna length on MUST chart 27.5 1.72 1.70 27.5 1.78 1.73 27.0 1.70 1.68 27.0 1.76 1.71 ② To find estimated height from ulna 26.5 1.69 1.66 26.5 1.75 1.70 length – Complete this once, on 26.0 1.68 1.65 26.0 1.73 1.68 admission 25.5 1.66 1.63 25.5 1.71 1.67 Follow a. -
Total Volar Extrusion of the Lunate and Scaphoid Proximal Pole with Concurrent Scapholunate Dissociation
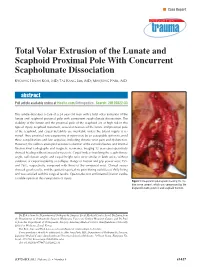
n Case Report Total Volar Extrusion of the Lunate and Scaphoid Proximal Pole With Concurrent Scapholunate Dissociation KYOUNG HWAN KOH, MD; TAE KANG LIM, MD; MIN JONG PARK, MD abstract Full article available online at Healio.com/Orthopedics. Search: 20120822-33 This article describes a case of a 24-year-old man with a total volar extrusion of the lunate and scaphoid proximal pole with concurrent scapholunate dissociation. The viability of the lunate and the proximal pole of the scaphoid are at high risk in this type of injury. Scaphoid nonunion, avascular necrosis of the lunate and proximal pole of the scaphoid, and carpal instability are inevitable unless the blood supply is re- stored. Thus, proximal row carpectomy at injury may be an acceptable option to avoid these complications and late sequelae, including chronic wrist pain and dysfunction. However, the authors attempted accurate reduction of the extruded bones and internal fixation.Final radiographs and magnetic resonance imaging 12 years postoperatively showed healing without avascular necrosis. Carpal indices involving the scapholunate angle, radiolunate angle, and carpal height ratio were similar in both wrists without evidence of carpal instability or collapse. Range of motion and grip power were 75% and 76%, respectively, compared with those of the uninjured wrist. Clinical scores showed good results, and the patient reported no pain during activities of daily living and was satisfied with his surgical results. Open reduction and internal fixation can be a viable option in this rare pattern of injury. Figure: Intraoperative photograph showing the me- dian nerve (arrow), which was compressed by the displaced lunate (asterisk) and scaphoid fracture. -

Carpal Tunnel Syndrome
Information O from Your Family Doctor Carpal Tunnel Syndrome What is carpal tunnel syndrome? hands a lot. You may notice that over time your Carpal tunnel syndrome (KAR-pal TUN-el grip gets weaker and you tend to drop heavy SIN-drome) is a common, painful disorder objects. of the wrist and hand. It happens when the median nerve, which runs through the wrist, How is it diagnosed? gets squeezed under a band of tissue called a Talk to your doctor if you are having these ligament. This causes pain and other symptoms symptoms. He or she will ask questions about along the nerve (see drawing). the ways you use your hands and about specific What causes it? Anything that increases Shading indicates area pressure on the median where symptoms are felt nerve can cause carpal tunnel syndrome. Sometimes pregnancy and health conditions like arthritis and diabetes can increase the pressure. People who use their hands and wrists repeatedly in the same way (for example, Transverse typists, carpenters, and carpal cashiers) are more likely to get ligament carpal tunnel syndrome. What are the symptoms? Carpal tunnel syndrome Thenar may cause pain, numbness, muscles Wrist or tingling in your wrist and bone hand, mostly in the middle finger, index finger, and Tendon thumb. The symptoms are Median usually worse at night and nerve when you use your wrists and ILLUSTRATION BY KATHRYN BORN continued O Page 1 of 2 Information O from Your Family Doctor Carpal Tunnel Syndrome (continued) symptoms in each part of your hand and wrist. He or she may also test how your nerves and Notes: muscles respond to electrical stimulation. -

New Fixation Approach for Transverse Metacarpal Neck Fracture: a Biomechanical Study
Chiu et al. Journal of Orthopaedic Surgery and Research (2018) 13:183 https://doi.org/10.1186/s13018-018-0890-2 RESEARCHARTICLE Open Access New fixation approach for transverse metacarpal neck fracture: a biomechanical study Yung-Cheng Chiu1,2, Ming-Tzu Tsai3, Cheng-En Hsu4,5, Horng-Chaung Hsu1,2, Heng-Li Huang6,7 and Jui-Ting Hsu6,7* Abstract Background: Fifth metacarpal neck fracture, also known as boxer’s fracture, is the most common metacarpal fracture. Percutaneous Kirschner-wire (K-wire) pinning has been shown to produce favorable clinical results. However, the fixation power of K-wires is a major concern. Plate fixation is also a surgical option, but it has the disadvantages of tendon adhesion, requirement of secondary surgery for removal of the implant, and postoperative joint stiffness. A fixation method that causes little soft tissue damage and provides high biomechanical stability is required for patients with fifth metacarpal neck fracture for whom surgical intervention is indicated. The present study proposed fixation using K-wires and a cerclage wire to treat fifth metacarpal neck fracture. The fixation power of this new method was compared with that of K-wires alone and plates. Methods: We used a saw blade to create transverse metacarpal neck fractures in 16 artificial metacarpal bone specimens, which were then treated with four types of fixation as follows: (1) locking plate with five locking bicortical screws (LP group), (2) regular plate with five bicortical screws (RP group), (3) two K-wires (K group), and (4) two K-wires and a figure-of-eight cerclage wire (KW group). -

6.3.3 Distal Radius and Wrist
6 Specific fractures 6.3 Forearm and hand 6.3.3 Distal radius and wrist 1 Assessment 657 1.1 Biomechanics 657 1.2 Pathomechanics and classification 657 1.3 Imaging 658 1.4 Associated lesions 659 1.5 Decision making 659 2 Surgical anatomy 660 2.1 Anatomy 660 2.2 Radiographic anatomy 660 2.3 Preoperative planning 661 2.4 Surgical approaches 662 2.4.1 Dorsal approach 2.4.2 Palmar approach 3 Management and surgical treatment 665 3.1 Type A—extraarticular fractures 665 3.2 Type B—partial articular fractures 667 3.3 Type C—complete articular fractures 668 3.4 Ulnar column lesions 672 3.4.1 Ulnar styloid fractures 3.4.2 Ulnar head, neck, and distal shaft fractures 3.5 Postoperative care 674 3.6 Complications 676 3.7 Results 676 4 Bibliography 677 5 Acknowledgment 677 656 PFxM2_Section_6_I.indb 656 9/19/11 2:45:49 PM Authors Daniel A Rikli, Doug A Campbell 6.3.3 Distal radius and wrist of this stable pivot. The TFCC allows independent flexion/ 1 Assessment extension, radial/ulnar deviation, and pronation/supination of the wrist. It therefore plays a crucial role in the stability of 1.1 Biomechanics the carpus and forearm. Significant forces are transmitted across the ulnar column, especially while making a tight fist. The three-column concept (Fig 6.3.3-1) [1] is a helpful bio- mechanical model for understanding the pathomechanics of 1.2 Pathomechanics and classification wrist fractures. The radial column includes the radial styloid and scaphoid fossa, the intermediate column consists of the Virtually all types of distal radial fractures, with the exception lunate fossa and sigmoid notch (distal radioulnar joint, DRUJ), of dorsal rim avulsion fractures, can be produced by hyper- and the ulnar column comprises the distal ulna (DRUJ) with extension forces [2]. -
Pearls and Pitfalls of Forearm Nailing
Current Concept Review Pearls and Pitfalls of Forearm Nailing Sreeharsha V. Nandyala, MD; Benjamin J. Shore, MD, MPH, FRCSC; Grant D. Hogue, MD Boston Children’s Hospital, Boston, MA Abstract: Pediatric forearm fractures are one of the most common injuries that pediatric orthopaedic surgeons manage. Unstable fractures that have failed closed reduction and casting require surgical intervention in order to correct length, alignment, and rotation to optimize forearm range of motion and function. Flexible intramedullary nailing (FIN) is a powerful technique that has garnered widespread popularity and adaptation for this purpose. Surgeons must become familiar with the technical pearls and pitfalls associated with this technique in an effort to prevent complications. Key Concepts: • Flexible intramedullary nailing is a useful technique that is widely utilized for most unstable both-bone forearm fractures except in the setting of highly comminuted fracture patterns or in refractures with abundant intrame- dullary callus formation. • Proper contouring of the rod prior to insertion and bending of the tip will help decrease the risk of malunion and facilitate rod passage across the fracture site. • The surgeon must be aware of the numerous pitfalls that are associated with flexible intramedullary nailing and the methods to mitigate each complication. Introduction Flexible intramedullary nailing (FIN) offers several key As enthusiasm grows for FIN as a treatment for pediatric advantages for the management of those pediatric fore- forearm fractures, surgeons must also clearly understand arm fractures that are not amenable to closed treatment. the technical nuances, controversies, and strategies to These advantages include cosmetic incisions for nail in- mitigate complications associated with this technique. -

Table 9-10 Ligaments of the Wrist and Their Function
Function and Movement of the Hand 283 Table 9-10 Ligaments of the Wrist and Their Function Extrinsic Ligaments Function Palmar radiocarpal Volarly stabilizes radius to carpal bones; limits excessive wrist extension Dorsal radiocarpal Dorsally stabilizes radius to carpal bones; limits excessive wrist flexion Ulnar collateral Provides lateral stability of ulnar side of wrist between ulna and carpals Radial collateral Provides lateral stability of radial side of wrist between radius and carpals Ulnocarpal complex and articular Stabilizes and helps glide the ulnar side of wrist; stabilizes distal disk (or triangular fibrocartilage radioulnar joint complex) Intrinsic Ligaments Palmar midcarpal Forms and stabilizes the proximal and distal rows of carpal bones Dorsal midcarpal Forms and stabilizes the proximal and distal rows of carpal bones Interosseous Intervenes between each carpal bone contained within its proximal or distal row Accessory Ligament Transverse carpal Stabilizes carpal arch and contents of the carpal tunnel Adapted from Hertling, D., & Kessler, R. (2006). Management of common musculoskeletal disorders: Physical therapy principles and methods. Philadelphia, PA: Lippincott, Williams & Wilkins.; Oatis, C. A. (2004). Kinesiology: The mechanics and pathomechanics of human movement. Philadelphia, PA: Lippincott, Williams & Wilkins.; Weiss, S., & Falkenstein, N. (2005). Hand rehabilitation: A quick reference guide and review. St. Louis, MO: Mosby Elsevier. The radial and ulnar collateral ligaments provide lateral and medial support, respectively, to the wrist joint. The ulnocarpal complex is more likely to be referred to as the triangular fibro- cartilage complex (TFCC) and includes the articular disk of the wrist. The TFCC is the major stabilizer of the distal radioulnar joint (DRUJ) and can tear after direct compressive force such as a fall on an outstretched hand. -

Isolated Trapezoid Fractures a Case Report with Compilation of the Literature
Bulletin of the NYU Hospital for Joint Diseases 2008;66(1):57-60 57 Isolated Trapezoid Fractures A Case Report with Compilation of the Literature Konrad I. Gruson, M.D., Kevin M. Kaplan, M.D., and Nader Paksima, D.O., M.P.H. Abstract as an axial load5,6 or bending stress7 transmitted indirectly Isolated fractures of the trapezoid bone have been rarely to the trapezoid through the second metacarpal. We present reported in the literature, the mechanism of injury being a case of an acute, isolated trapezoid fracture that resulted an axial or bending load transmitted through the second from direct trauma to the distal carpus and that was treated metacarpal. We report a case of an isolated, nondisplaced nonoperatively. Additionally, strategies for diagnosis and trapezoid fracture that was sustained by direct trauma treatment, as well as a synthesis of the published results and subsequently treated successfully in a short-arm cast. for both isolated and concomitant trapezoid fractures, are Diagnostic and treatment strategies for isolated fractures presented. of the trapezoid bone are reviewed as well as the results of operative and nonoperative treatment. Case Report A 25-year-old right-hand dominant male presented to the ractures of the carpus most commonly involve the emergency room (ER) complaining of isolated right-wrist scaphoid,1 with typical physical examination findings pain and swelling of 1 day’s duration. The patient stated Fof “snuffbox” tenderness. This presentation is fre- that a heavy metal door at work had closed onto the back quently the result of the patient falling onto an outstretched of his wrist causing an immediate onset of swelling and hand. -

Upper Extremity Injuries in Pediatric Athletes
Review Article Page 1 of 10 Upper extremity injuries in pediatric athletes Kristen M. Sochol, Daniel A. Charen, Jaehon Kim Department of Orthopedics at Mount Sinai Hospital, New York, NY, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: All authors; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Kristen M. Sochol, MD. Department of Orthopedics at Mount Sinai Hospital, 5E 98th St, New York, NY 10029, USA. Email: [email protected]. Abstract: Upper extremity injuries in the pediatric patient are common, but are often more difficult to diagnose compared to their adult counterparts due to the gradual progression of cartilage ossification. Common pediatric upper extremity injuries include fractures and soft tissue trauma. Less prevalent injuries include sport specific overuse injuries. Fractures in the pediatric population are best described using the Salter-Harris classification, which has management and prognostic implications. Most pediatric upper extremity injuries can be managed with an initial trial of immobilization and early range of motion, followed by surgical intervention if necessary. Children have a robust healing response to bony and soft tissue injuries, and have good outcomes with appropriate management. Keywords: Pediatric athletes; upper extremity; Salter-Harris; overuse; injury Received: 14 February 2018; Accepted: 08 May 2018; Published: 15 May 2018. doi: 10.21037/aoj.2018.05.04 View this article at: http://dx.doi.org/10.21037/aoj.2018.05.04 Introduction joints are constrained by a network of ligaments that are primarily named after their attachment sites. -

Carpals and Tarsals of Mule Deer, Black Bear and Human: an Osteology Guide for the Archaeologist
Western Washington University Western CEDAR WWU Graduate School Collection WWU Graduate and Undergraduate Scholarship 2009 Carpals and tarsals of mule deer, black bear and human: an osteology guide for the archaeologist Tamela S. Smart Western Washington University Follow this and additional works at: https://cedar.wwu.edu/wwuet Part of the Anthropology Commons Recommended Citation Smart, Tamela S., "Carpals and tarsals of mule deer, black bear and human: an osteology guide for the archaeologist" (2009). WWU Graduate School Collection. 19. https://cedar.wwu.edu/wwuet/19 This Masters Thesis is brought to you for free and open access by the WWU Graduate and Undergraduate Scholarship at Western CEDAR. It has been accepted for inclusion in WWU Graduate School Collection by an authorized administrator of Western CEDAR. For more information, please contact [email protected]. MASTER'S THESIS In presenting this thesis in partial fulfillment of the requirements for a master's degree at Western Washington University, I grant to Western Washington University the non-exclusive royalty-free right to archive, reproduce, distribute, and display the thesis in any and all forms, including electronic format, via any digital library mechanisms maintained by WWu. I represent and warrant this is my original work, and does not infringe or violate any rights of others. I warrant that I have obtained written permissions from the owner of any third party copyrighted material included in these files. I acknowledge that I retain ownership rights to the copyright of this work, including but not limited to the right to use all or part of this work in future works, such as articles or books. -

REVIEW ARTICLE Osteoarthritis of the Wrist
REVIEW ARTICLE Osteoarthritis of the Wrist Krista E. Weiss, Craig M. Rodner, MD From Harvard College, Cambridge, MA and Department of Orthopaedic Surgery, University of Connecticut Health Center, Farmington, CT. Osteoarthritis of the wrist is one of the most common conditions encountered by hand surgeons. It may result from a nonunited or malunited fracture of the scaphoid or distal radius; disruption of the intercarpal, radiocarpal, radioulnar, or ulnocarpal ligaments; avascular necrosis of the carpus; or a developmental abnormality. Whatever the cause, subsequent abnormal joint loading produces a spectrum of symptoms, from mild swelling to considerable pain and limitations of motion as the involved joints degenerate. A meticulous clinical and radiographic evaluation is required so that the pain-generating articulation(s) can be identi- fied and eliminated. This article reviews common causes of wrist osteoarthritis and their surgical treatment alternatives. (J Hand Surg 2007;32A:725–746. Copyright © 2007 by the American Society for Surgery of the Hand.) Key words: Wrist, osteoarthritis, arthrodesis, carpectomy, SLAC. here are several different causes, both idio- of events is analogous to SLAC wrist and has pathic and traumatic, of wrist osteoarthritis. been termed scaphoid nonunion advanced collapse Untreated cases of idiopathic carpal avascular (SNAC). Wrist osteoarthritis can also occur second- T 1 2 necrosis, as in Kienböck’s or Preiser’s disease, may ary to an intra-articular fracture of the distal radius or result in radiocarpal arthritis. Congenital wrist abnor- ulna or from an extra-articular fracture resulting in malities, such as Madelung’s deformity,3,4 can lead malunion and abnormal joint loading. -

Radiohamate Impingement After Proximal Row Carpectomy ‘Radiohamate Impingement PRC’
Acta Orthop. Belg., 2020, 86 e-supplement 1, 19-21 CASE REPORT Radiohamate impingement after proximal row carpectomy ‘Radiohamate impingement PRC’ Pieter Caekebeke, Luc De Smet From the Department of Orthopaedics UZ Leuven, Pellenberg, Belgium Radiocarpal impingement after PRC is a well-known from 0% to 18% (5). Radiocarpal and pisiform complication due to impingement of the radial styloid impingement have been described after PRC. The against the radial carpal bones. A less common first is probably due to the proximalization of the impingement syndrome is that of the pisiforme. distal row with impingement of the trapezium/ We describe a radiohamate impingement and its trapezoid against the radial styloid process. The diagnosis and treatment. Based on a case we saw treatment is a radial styloid process resection for at our practice. Diagnosis is bases on standard radiographs and SPECT-CT. The treatment is the first and a pisiformectomy for the latter (3,5). No initially conservative. Surgery is necessary when other impingement syndromes have been described. conservative treatment fails and consists of resectie We present a case of radiohamate impingement of the proximal pole of the hamate. syndrome after proximal row carpectomy. Keywords: Radiohamate ; impingement ; proximal row CASE REPORT carpectomy. A 53-year-old mechanic contacted us 1 year after a work-accident with localized radiocarpal INTRODUCTION pain and swelling. Radiographs showed a stage Proximal row carpectomy (PRC) is a well- two SLAC wrist. (Fig. 1) A PRC with synovectomy established motion-preserving salvage procedure was performed. The following 3 years were for degenerative disorders of the proximal carpal uneventful with no to minimal pain complaints.