De Quervain's Release Standard of Care PT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Multiple Pulley Rupture Following Corticosteroid Injection for Trigger Digit: Case Report
SCIENTIFIC ARTICLE Multiple Pulley Rupture Following Corticosteroid Injection for Trigger Digit: Case Report Cassie Gyuricza, MD, Eva Umoh, BA, Scott W. Wolfe, MD We report a case of pulley rupture following repeated local corticosteroid injections for trigger digit. The treatment involved exploration, tenolysis, and reconstruction using the palmaris longus tendon. (J Hand Surg 2009;34A:1444–1448. © 2009 Published by Elsevier Inc. on behalf of the American Society for Surgery of the Hand.) Key words Corticosteroid, pulley rupture, trigger digit. RIGGER DIGIT, OR stenosing tenosynovitis,isa local corticosteroid injection through a lateral approach condition characterized by painful locking or at the proximal phalanx10 (0.5 mL local anesthetic and Tsnapping of a digit caused by mechanical im- 0.5 mL triamcinolone acetonide 40 mg/mL [Kenalog- pingement of the flexor tendon passing through a hy- 40, Bristol-Meyers Squibb Co, Princeton, NJ]). Her pertrophic A1 pulley. Initial conservative management symptoms of pain temporarily improved, but 4 months of trigger digits with various corticosteroid preparations later, the patient returned with recurrent pain and a is well described.1–4 Side effects, including subcutane- second local corticosteroid injection was administered, ous fat atrophy, pain, depigmentation of the skin, and again using the lateral approach. During the ensuing 8 transient elevation of urine and blood glucose levels in months, the patient had persistent pain and tenderness patients with diabetes, are generally mild and self- over the A2 pulley. The patient also developed pain at limiting.5,6 We are aware of 2 previously reported cases the A1 pulley, and a third injection (0.5 mL local of delayed flexor tendon rupture following corticoste- anesthetic and 0.5 mL triamcinolone acetonide 40 mg/ 7,8 roid injections for trigger digit thought to be the result mL) was given into the palmar surface overlying the A1 of intratendinous injection. -

Acute Hand Infections
CURRENT CONCEPTS Acute Hand Infections Meredith Osterman, MD, Reid Draeger, MD, Peter Stern, MD CME INFORMATION AND DISCLOSURES The Review Section of JHS will contain at least 3 clinically relevant articles selected by the Provider Information can be found at http://www.assh.org/Pages/ContactUs.aspx. editor to be offered for CME in each issue. For CME credit, the participant must read the Technical Requirements for the Online Examination can be found at http://jhandsurg. articles in print or online and correctly answer all related questions through an online org/cme/home. examination. The questions on the test are designed to make the reader think and will occasionally require the reader to go back and scrutinize the article for details. Privacy Policy can be found at http://www.assh.org/pages/ASSHPrivacyPolicy.aspx. The JHS CME Activity fee of $30.00 includes the exam questions/answers only and does not ASSH Disclosure Policy: As a provider accredited by the ACCME, the ASSH must ensure fi include access to the JHS articles referenced. balance, independence, objectivity, and scienti c rigor in all its activities. Disclosures for this Article Statement of Need: This CME activity was developed by the JHS review section editors Editors and review article authors as a convenient education tool to help increase or affirm fl reader’s knowledge. The overall goal of the activity is for participants to evaluate the Ghazi M. Rayan, MD, has no relevant con icts of interest to disclose. appropriateness of clinical data and apply it to their practice and the provision of patient Authors care. -
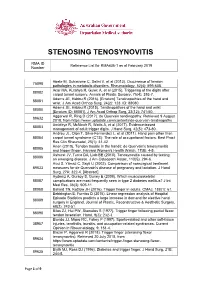
Reference List Concerning De Quervain Tenosynovitis
STENOSING TENOSYNOVITIS RMA ID Reference List for RMA436-1 as at February 2019 Number Abate M, Schiavone C, Salini V, et al (2013). Occurrence of tendon 75098 pathologies in metabolic disorders. Rheumatology, 52(4): 599-608. Acar MA, Kutahya H, Gulec A, et al (2015). Triggering of the digits after 88082 carpal tunnel surgery. Annals of Plastic Surgery, 75(4): 393-7. Adams JE, Habbu R (2016). [Erratum] Tendinopathies of the hand and 88081 wrist. J Am Acad Orthop Surg, 24(2): 123. ID: 88080. Adams JE, Habbu R (2015). Tendinopathies of the hand and wrist 88080 [Erratum ID: 88081]. J Am Acad Orthop Surg, 23(12): 741-50. Aggarwal R, Ring D (2017). de Quervain tendinopathy. Retrieved 9 August 89632 2018, from https://www.uptodate.com/contents/de-quervain-tendinopathy Amirfeyz R, McNinch R, Watts A, et al (2017). Evidence-based 88083 management of adult trigger digits. J Hand Surg, 42(5): 473-80. Andreu JL, Oton T, Silva-Fernandez L, et al (2011). Hand pain other than 88084 carpal tunnel syndrome (CTS): The role of occupational factors. Best Pract Res Clin Rheumatol, 25(1): 31-42. Anon (2010). Tendon trouble in the hands: de Quervain's tenosynovitis 88085 and trigger finger. Harvard Women's Health Watch, 17(8): 4-5. Ashurst JV, Turco DA, Lieb BE (2010). Tenosynovitis caused by texting: 88086 an emerging disease. J Am Osteopath Assoc, 110(5): 294-6. Avci S, Yilmaz C, Sayli U (2002). Comparison of nonsurgical treatment 89633 measures for de Quervain's disease of pregnancy and lactation. J Hand Surg, 27A: 322-4. -

De Quervain's Syndrome
De Quervain's syndrome What is it? Treatment options are: Through a transverse or longitudinal De Quervain's syndrome is a painful condition 1. Avoiding activities that cause pain, if incision, and protecting the nerve that affects tendons where they run through a possible branches just under the skin, the surgeon tunnel on the thumb side of the wrist. widens the tendon tunnel by slitting its roof. The tunnel roof forms again as the 2. Using a wrist/thumb splint, which can split heals, but it is wider and the What is the cause? often be obtained from a sports shop or a physiotherapist. It needs to immobilize tendons have sufficient room to move the thumb as well as the wrist. without pain. It appears without obvious cause in many cases. Pain relief is usually rapid. The scar may Mothers of small babies seem particularly prone 3. Steroid injection relieves the pain in be sore and unsightly for several weeks. to it, but whether this is due to hormonal Because the nerve branches were gently changes after pregnancy or due to lifting the about 70% of cases. The risks of injection are small, but it very occasionally causes moved to see the tunnel, transient baby repeatedly is not known. There is little temporary numbness can occur on the evidence that it is caused by work activities, but some thinning or colour change in the skin at the site of injection. back of the hand or thumb. Other risks the pain can certainly be aggravated by hand are the risks of any surgery such as use at work, at home, in the garden or at sport. -

Radiohamate Impingement After Proximal Row Carpectomy ‘Radiohamate Impingement PRC’
Acta Orthop. Belg., 2020, 86 e-supplement 1, 19-21 CASE REPORT Radiohamate impingement after proximal row carpectomy ‘Radiohamate impingement PRC’ Pieter Caekebeke, Luc De Smet From the Department of Orthopaedics UZ Leuven, Pellenberg, Belgium Radiocarpal impingement after PRC is a well-known from 0% to 18% (5). Radiocarpal and pisiform complication due to impingement of the radial styloid impingement have been described after PRC. The against the radial carpal bones. A less common first is probably due to the proximalization of the impingement syndrome is that of the pisiforme. distal row with impingement of the trapezium/ We describe a radiohamate impingement and its trapezoid against the radial styloid process. The diagnosis and treatment. Based on a case we saw treatment is a radial styloid process resection for at our practice. Diagnosis is bases on standard radiographs and SPECT-CT. The treatment is the first and a pisiformectomy for the latter (3,5). No initially conservative. Surgery is necessary when other impingement syndromes have been described. conservative treatment fails and consists of resectie We present a case of radiohamate impingement of the proximal pole of the hamate. syndrome after proximal row carpectomy. Keywords: Radiohamate ; impingement ; proximal row CASE REPORT carpectomy. A 53-year-old mechanic contacted us 1 year after a work-accident with localized radiocarpal INTRODUCTION pain and swelling. Radiographs showed a stage Proximal row carpectomy (PRC) is a well- two SLAC wrist. (Fig. 1) A PRC with synovectomy established motion-preserving salvage procedure was performed. The following 3 years were for degenerative disorders of the proximal carpal uneventful with no to minimal pain complaints. -

(UED). a Health Care Provider Shall Determine the Nature of an Upper Extremity Disorder Before Initiating Treatment
1 REVISOR 5221.6300 5221.6300 UPPER EXTREMITY DISORDERS. Subpart 1. Diagnostic procedures for treatment of upper extremity disorders (UED). A health care provider shall determine the nature of an upper extremity disorder before initiating treatment. A. An appropriate history and physical examination must be performed and documented. Based on the history and physical examination the health care provider must at each visit assign the patient to the appropriate clinical category according to subitems (1) to (6). The diagnosis must be documented in the medical record. Patients may have multiple disorders requiring assignment to more than one clinical category. This part does not apply to upper extremity conditions due to a visceral, vascular, infectious, immunological, metabolic, endocrine, systemic neurologic, or neoplastic disease process, fractures, lacerations, amputations, or sprains or strains with complete tissue disruption. (1) Epicondylitis. This clinical category includes medial epicondylitis and lateral epicondylitis, ICD-9-CM codes 726.31 and 726.32. (2) Tendonitis of the forearm, wrist, and hand. This clinical category encompasses any inflammation, pain, tenderness, or dysfunction or irritation of a tendon, tendon sheath, tendon insertion, or musculotendinous junction in the upper extremity at or distal to the elbow due to mechanical injury or irritation, including, but not limited to, the diagnoses of tendonitis, tenosynovitis, tendovaginitis, peritendinitis, extensor tendinitis, de Quervain's syndrome, intersection syndrome, flexor tendinitis, and trigger digit, including, but not limited to, ICD-9-CM codes 726.4, 726.8, 726.9, 726.90, 727, 727.0, 727.00, 727.03, 727.04, 727.05, 727.09, 727.2, 727.3, 727.4 to 727.49, 727.8 to 727.82, 727.89, and 727.9. -

Top Hand, and Wrist Problems
12/10/2016 TOP HAND, AND WRIST Disclosures PROBLEMS: HOW TO • None SPOT THEM IN CLINIC Nicolas H. Lee, MS MD [email protected] UCSF Dept of Orthopaedic Surgery Assistant Clinical Professor Hand, Upper Extremity and Microvascular Surgery Dec. 10 th , 2016 Outline Outline • Carpal Tunnel Syndrome •Carpal Tunnel Syndrome • Trigger Finger • • Basal Joint arthritis Trigger Finger • Basal Joint arthritis • De Quervain tenosynovitis • De Quervain tenosynovitis • Mallet Finger • Mallet Finger • Ganglion cyst • Ganglion cyst 1 12/10/2016 Carpal Tunnel Syndrome • Compression of median nerve in carpal tunnel • Irritation of the nerve presents as numbness/pain 10 structures 9 flexor tendons Median nerve https://www.pinterest.com/pin/429812358163325007/ Anatomy (motor) Etiology 1. Idiopathic – most common 2. Anatomic – rare • Thenar Muscle (OAF) 3. Systemic – DM, hypothyroidism • Opponens Pollicis (deep) 4. **** Occupational Exposure • Abductor Pollicis Brevis (superficial) **** “A direct relationship between repetitive work • Flexor Pollicis Brevis activity (eg, keyboarding) and CTS has never been (superficial 1/2) objectively demonstrated.” 1 http://teachmeanatomy.info/upper-limb/muscles/hand/ 2 12/10/2016 Rare anatomic causes Carpal Tunnel Syndrome ● HPI – systemic risk factors Tenosynovitis CMC arthritis ◦ More common in: Ganglion Fracture 1) Diabetics 2) Hypothyroidism 3) Pregnancy (20-45%) Persistent Median artery Acromegaly Abnormal muscle Tumor Carpal Tunnel Syndrome ● CC: ◦ “I wake up at night and my hands are asleep” ◦ “I have to shake them to get the blood flowing again” ◦ “I have to run them under warm water and then I can go back to sleep” ◦ “Fingers go numb when I drive” ◦ “My hand goes numb when I use my cell phone” ◦ “I am always dropping things” Carpal Tunnel Syndrome Cranford, C.S. -

Musculoskeletal Ultrasound in the Evaluation of Polymyalgia Rheumatica
Review Med Ultrason 2015, Vol. 17, no. 3, 361-366 DOI: 10.11152/mu.2013.2066.173.aig Musculoskeletal ultrasound in the evaluation of Polymyalgia Rheumatica Iolanda Maria Rutigliano, Chiara Scirocco, Fulvia Ceccarelli, Annacarla Finucci, Annamaria Iagnocco Rheumatology Unit, Sapienza Università di Roma, Rome, Italy Abstract Polymyalgia rheumatica (PMR) is a relatively frequent disease affecting individuals older than 50 years and is character- ized by inflammatory involvement of the shoulder and hip girdles and the neck. Clinical manifestations are represented by pain and morning stiffness in this regions. An extensive and comprehensive assessment of the inflammatory status is crucial in PMR patients, including imaging evaluation. This narrative review reports the current available data in the literature about the role of musculoskeletal ultrasound in PMR. Keywords: polymyalgia rheumatica, ultrasound, bursitis, tenosynovitis Introduction PMR is characterized by pain and morning stiffness, longer than 45 min, involving the neck and the shoulder Polymyalgia rheumatica (PMR) is an inflammatory and hip girdles. Stiffness and pain are usually bilateral, rheumatic condition that typically affects individuals old- worsen in the morning and improve with activity. Fa- er than 50 years, with incidence increasing with age. An tigue, malaise, anorexia, weight loss and fever are also Italian epidemiologic study reported an annual incidence common and are considered “constitutional symptoms”. rate of PMR over the period 1980–1988 of 12.7/100,000 An association between PMR and giant-cell arteritis [1-2]. The etiology of PMR remains unknown, although (GCA) has been described and PMR has been identified currently the role of both genetic and environmental fac- in 40-60% of patients affected by GCA; on the contra- tors, such as infections, has been hypothesized. -
![De Quervain's Tenosynovitis: [11] Lee KH, Kang CN, Lee BG, a Case-Control Study with Prospe Tively Jung WS, Kim DY, Lee CH](https://docslib.b-cdn.net/cover/6782/de-quervains-tenosynovitis-11-lee-kh-kang-cn-lee-bg-a-case-control-study-with-prospe-tively-jung-ws-kim-dy-lee-ch-886782.webp)
De Quervain's Tenosynovitis: [11] Lee KH, Kang CN, Lee BG, a Case-Control Study with Prospe Tively Jung WS, Kim DY, Lee CH
Chapter De Quervain’s Tenosynovitis: Effective Diagnosis and Evidence-Based Treatment Jenson Mak Abstract De Quervain’s tenosynovitis (DQT) is a repetitive stress condition located at the first dorsal compartment of the wrist at the radial styloid. The extensor pollicis brevis (EPB) and abductor pollicis longus (APL) tendons and each tendon sheath are inflamed and this may result in thickening of the first dorsal extensor sheath. Workers who perform repetitive activities of the wrist and hand and those who rou- tinely use their thumbs in grasping and pinching motions in a repetitive manner are most susceptible to DQT. Conservative treatments include activity modification, modalities, orthotics, and manual therapy. This chapter identifies, in an evidence base manner through the literature, the most effective diagnostic measures for DQT. It also examines the evidence base on (or lack thereof) the treatment or treat- ment combinations to reduce pain and improve functional outcomes for patients with DQT. Keywords: De Quervain’s tenosynovitis, diagnosis, treatment, workplace, evidence-based 1. Introduction In 1893, Paul Jules Tillaux described a painful crepitus sign (Aïe crépitant de Tillaux)—tenosynovitis of the adductor and the short extensor of the thumb. In 1894, Fritz de Quervain, a Swiss surgeon, first described tenosynovitis on December 18, 1894, in Mrs. D., a 35-year-old woman who had severe pain in the extensor muscle region of the thumb, excluding tuberculosis. “It is a condition affecting the tendon sheaths of the abductor pollicis longus, and the extensor pollicis brevis. It has definite symptoms and signs. The condition may affect other extensor tendons at the wrist” [1]. -

Treatment of the Painful Biceps Tendon—Tenotomy Or Tenodesis?
ARTICLE IN PRESS Current Orthopaedics (2006) 20, 370–375 Available at www.sciencedirect.com journal homepage: www.elsevier.com/locate/cuor UPPER LIMB Treatment of the painful biceps tendon—Tenotomy or tenodesis? F. LamÃ, D. Mok Shoulder Unit, Department of Orthopaedics, Epsom General Hospital, Dorking Road, Epsom, Surrey KT18 7EG, UK KEYWORDS Summary Biceps; The function of the long head of biceps tendon in the shoulder remains controversial. Tenodesis; Pathology of the biceps tendon such as tenosynovitis, subluxation and pre-rupture are Tenotomy; intimately associated with rotator cuff disease. Treatment therefore varies widely among Shoulder surgery surgeons and range from non-operative management to biceps tenotomy or tenodesis. The purpose of this article is to provide an up to date review on the indications and results of biceps tenotomy and tenodesis. & 2006 Elsevier Ltd. All rights reserved. Anatomy Therefore, rupture of the biceps tendon most commonly occurs proximally near the glenoid labrum and distally in the The anatomical origin of the long head of biceps tendon is bicipital groove. variable. It arises most commonly from the glenoid labrum (45%), less commonly from the supraglenoid tubercle (30%) Function and in the remaining it arises from both the glenoid labrum and the supraglenoid tubercle (25%). The tendon travels The biceps muscle-tendon unit is one of many structures in obliquely within the glenohumeral joint to exit beneath the the human body to cross two joints. In the elbow, it serves transverse humeral ligament along the intertubercular primarily as a forearm supinator. Its secondary role is as an sulcus or bicipital groove. In the glenohumeral joint the elbow flexor. -

Research Article Prevalence and Awareness Evaluation of De
Available online www.ijpras.com International Journal of Pharmaceutical Research & Allied Sciences, 2020, 9(4):151-157 ISSN : 2277-3657 Research Article CODEN(USA) : IJPRPM Prevalence and Awareness Evaluation of De Quervain’s Tenosynovitis among Students in the Kingdom of Saudi Arabia Bashar Reada1, Nawaf Alshaebi2*, Khalid Almaghrabi2, Abdullah Alshuaibi2, Arwa Abulnaja3, Khames Alzahrani4 1 Department of Medicine, MBBS, FSCSC, College of Medicine, King Abdulaziz University Hospital, Jeddah, KSA. 2 Department of Medicine, Undergraduate, College of Medicine, King Abdulaziz University, Jeddah, KSA. 3 Department of Medicine, Medical Intern, College of Medicine, King Abdulaziz University, Jeddah, KSA. 4 Department of Medicine, BDS, Ministry of Health, Jeddah, Saudi Arabia. *Email: nawafalshaebi @ hotmail.com ABSTRACT Introduction: De Quervain's tenosynovitis is characterized by inflammation and thickening of the tendons of the extensor pollicis brevis and abductor pollicis longus muscles and the synovial sheath, leading to a common cause of wrist pain that typically occurs in adults. This condition has been given several other names such as texting tenosynovitis, BlackBerry thumb, washerwoman's sprain, gamer’s thumb, teen texting tendonitis, WhatsAppitis, and radial styloid tenosynovitis, all of which involve repeated thumb pinching and wrist movement. Objectives: The purpose of this study was to determine the prevalence of de Quervain’s tenosynovitis among students using smartphones in Saudi Arabia. Many studies have been conducted on this disease in other countries, but not many have been performed in Saudi Arabia. Our aim was to obtain more information about the disease prevalence among students in Saudi Arabia. Our secondary objective was to determine the correlation of the condition with different demographics and risk factors in our study population, such as age, sex, and time spent texting. -

Your Guide to Trigger Finger Surgery Brian J
Your Guide to Trigger Finger Surgery Brian J. Bear, MD OrthoIllinois Hand, Wrist, and Elbow Center of Excellence Care Team and Contact Numbers: Brian J. Bear, MD Main Phone line . 815-398-9491 OrthoIllinois Kailey - Lead Nurse . .815-398-9491 324 Roxbury Road Ronda - Surgery Scheduler . 815-484-6969 Rockford, IL Sadie - Office Scheduler . .815-484-6996 TABLE OF CONTENTS Learn about Dr. Bear . 2 What is Trigger Finger/Trigger Thumb?. 3 Surgical Treatment v Description of Trigger Finger Release . 3 The Surgical Experience v Information to Keep in Mind Prior to Surgery . 4 v Pre-Admission Guide for Surgery . 5 v Pre-operative Phase . 6 v Intra-operative Phase . 7 v Post-operative Phase . 8 After Surgery v While You Recover at Home . 9 Commonly Asked Questions . 10-11 What Can I Do After Surgery? . 13 1 Learn More About Dr. Bear I would like to take this opportunity to tell you more about myself and my experience in health care. Originally from Winnetka, Illinois, I attended Northwestern University graduating in 1987, cum laude, president of Mortar Board Senior Honor Society and a member of Phi Betta Kappa. I continued my studies at Northwestern University School of Medicine, receiving my medical degree in 1991 as a member of Alpha Omega Alpha honor society. Following my graduation, I pursued advanced orthopedic training at Cornell Hospital for Special Surgery, which is ranked as the top orthopedic hospital in the United States. In addition, I completed a specialized training fellowship program in elbow and hand surgery at the Mayo Clinic. My practice is focused on shoulder, elbow, hand, microvascular, traumatic, and reconstructive surgery.