Optos 200Tx and Heidelberg Spectralis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Deep Venous Thrombosis with Suspected Pulmonary Embolism
Thoracic Imaging Peter A. Loud, MD Deep Venous Thrombosis Douglas S. Katz, MD Dennis A. Bruce, MD with Suspected Pulmonary Donald L. Klippenstein, MD Zachary D. Grossman, MD Embolism: Detection with Combined CT Venography Index terms: Computed tomography (CT), 1 angiography, 9*.129142, and Pulmonary Angiography 9*.12915, 9*.12916 Embolism, pulmonary, 60.72 Pulmonary angiography, 944.12914, 944.12915, 944.12916 PURPOSE: To determine the frequency and location of deep venous thrombosis at Veins, thrombosis, 9*.751, 9*.12914 computed tomographic (CT) venography after CT pulmonary angiography in a large series of patients clinically suspected of having pulmonary embolism and to Radiology 2001; 219:498–502 compare the accuracy of CT venography with lower-extremity venous sonography. Abbreviation: MATERIALS AND METHODS: Venous phase images were acquired from the DVT ϭ deep venous thrombosis diaphragm to the upper calves after completion of CT pulmonary angiography in 650 patients (373 women, 277 men; age range, 18–99 years; mean age, 63 years) 1 From the Department of Radiology, to determine the presence and location of deep venous thrombosis. Results of CT Roswell Park Cancer Institute, Elm and Carlton Sts, Buffalo, NY 14263 (P.A.L., venography were compared with those of bilateral lower-extremity venous sonog- D.L.K., Z.D.G.), and the Department raphy in 308 patients. of Radiology, Winthrop University Hospital, Mineola, NY (D.S.K., D.A.B.). RESULTS: A total of 116 patients had pulmonary embolism and/or deep venous From the 1999 RSNA scientific assem- thrombosis, including 27 patients with pulmonary embolism alone, 31 patients with bly. -

Fluorescein Angiography Findings in Both Eyes of a Unilateral Retinoblastoma Case During Intra-Arterial Chemotherapy with Melphalan
Int J Ophthalmol, Vol. 12, No. 12, Dec.18, 2019 www.ijo.cn Tel: 8629-82245172 8629-82210956 Email: [email protected] ·Letter to the Editor· Fluorescein angiography findings in both eyes of a unilateral retinoblastoma case during intra-arterial chemotherapy with melphalan Cem Ozgonul1, Neeraj Chaudhary2, Raymond Hutchinson3, Steven M. Archer1, Hakan Demirci1 1Department of Ophthalmology and Visual Sciences, W.K. was inserted into the left femoral artery, advanced into the Kellogg Eye Center, MI 48105, USA internal carotid and up to the origin of the ophthalmic artery. 2Department of Radiology, University of Michigan, MI 48109, Once the catheter tip position was confirmed at the origin USA of the ophthalmic artery by fluoroscopy, 5 mg melphalan 3Department of Pediatric Hematology/Oncology, University of was infused in a pulsatile fashion over 30min. There was Michigan, MI 48109, USA no anatomical variant of orbital vascular structure. During Correspondence to: Hakan Demirci. Department of the 2nd IAC, following the infusion of melphalan, sodium Ophthalmology and Visual Science, W.K. Kellogg Eye Center, fluorescein dye at a dose of 7.7 mg/kg was injected through the 1000 Wall St, Ann Arbor, MI 48105, USA. hdemirci@med. same microcatheter. Real-time FA was recorded by using the umich.edu RetCam III (Clarity Medical Systems, Pleasanton, California). Received: 2018-11-01 Accepted: 2019-04-09 FA was repeated 4wk later during the 3rd IAC in the same manner, before infusion of the chemotherapy. In both sessions, DOI:10.18240/ijo.2019.12.24 there was no catheterization or injection of contrast material into the untreated carotid and ophthalmic artery. -

Risk Factors for Adverse Reactions of Fundus Fluorescein Angiography
Original Article Risk factors for adverse reactions of fundus fluorescein angiography Yi Yang1, Jingzhuang Mai2, Jun Wang1 1Department of Ophthalmology, 2Epidemiology Division, Department of Cardiac Surgery, Guangdong Cardiovascular Institute, Guangdong General Hospital, Guangzhou 510080, China Contributions: (I) Conception and design: All authors; (II) Administrative support: All authors; (III) Provision of study materials or patients: Y Yang; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: Y Yang, JZ Mai; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Yi Yang. Department of Ophthalmology, Guangdong General Hospital, #106, Zhongshan Second Road, Guangzhou 510080, China. Email: [email protected]. Background: To explore the difference between the outcomes of correlations between a series of variables and adverse reactions (ARs) to fluorescein from univariate and multivariate analysis and to evaluate the nausea effects in different age groups. Methods: A retrospective study of patients undergoing consecutive fluorescein angiography between March 2010 and February 2012 was conducted. No patients were excluded on the ground of age, presence of atopy, allergy history, previous procedures without severe allergic ARs, asymptomatic hypertension and kidney failure with serum creatinine levels lower than 250 μmol/L or with renal dialysis. Results: A total of 829 patients were enrolled and 22.2% of them had ARs. The majority of reactions were nausea (12.1%) which occurred less when age became old (P<0.0001). When the correlations between a series of variables and ARs were assessed separately, age (P<0.0001), prior reactions (P<0.0001) and motion sickness (P=0.0062) were highly and cardio/cerebrovascular disease (P=0.0015), diabetes (P=0.0001) and renal disease (P=0.0219) were lowly related to ARs. -
Spring Programme 2011
Faculty of Radiologists Royal College of Surgeons in Ireland Combined Spring Meeting 8th & 9 th April 2011 Venue: Castlemartyr Hotel, Co. Cork. Programme Faculty of Radiologists, Royal College of Surgeons in Ireland CPD Credits Awarded: 5 Royal College of Radiologists credits are applied for. Friday 8 th April 2011 3.30-4.30pm Registration 4.30-5.30pm Stroke in 2011, Moderator: Dr. Ian Kelly, Waterford Regional Hospital 4.30-5.00pm Acute Stoke Imaging. Dr Noel Fanning, Cork University Hospital, Cork 5.00-5.30pm Stroke: A clinical perspective. Dr. George Pope, John Radcliffe Hospitals, Oxford 5.30-6.30pm Moderator: Dr. Adrian Brady, Dean, Faculty of Radiologists Belfast to Bosnia and Autopsy to Virtopsy Dr. Jack Crane, State Pathologist, NI 8pm Dinner Saturday 9 th April 2011 8.30-9.00am Registration 9.00-10.00am Liver hour. Moderator: Dr John Feeney, AMNCH, Dublin 9.00-9.30am Liver imaging pre metastatectomy. Dr. Peter MacEneaney, Mercy University Hospital, Cork 9.30-10.00am Parenchymal and focal liver biopsy - when and how. Dr Stephen J Skehan St Vincent's University Hospital, Dublin 10.00-11.00am Paediatric Hour. Moderator: Dr. Stephanie Ryan, The Children’s University Hospital Temple Street, Dublin 10.00-10.30am Paediatric Abdominal Emergencies. Dr Eoghan Laffan, The Children’s, University Hospital Temple Street, Dublin 10.30-11.00am Non Accidental Injury. Dr Conor Bogue, Cork University Hospital, Cork 11.00-11.30am Tea/Coffee Break and Poster Exhibition 11.30-12.30pm MSK Hour. Moderator: Dr Orla Buckley, AMNCH, Dublin 11.30-12.00pm Image guided joint interventions. -
National Correct Coding Initiative's (Ncci) General
NATIONAL CORRECT CODING INITIATIVE’S (NCCI) GENERAL CORRESPONDENCE LANGUAGE AND SECTION-SPECIFIC EXAMPLES (FOR NCCI PROCEDURE TO PROCEDURE (PTP) EDITS AND MEDICALLY UNLIKELY EDITS (MUE)) EFFECTIVE: April 1, 2017* *INCLUDES 2017 HCPCS/CPT CODES Current Procedural Terminology (CPT) codes, descriptions and other data only are copyright 2016 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association. Applicable FARS\DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for the data contained or not contained herein. TABLE OF CONTENTS Section Page Introduction 5 General Correspondence Language for NCCI PTP Edits and Medically Unlikely Edits (MUEs) Standard preparation/monitoring services for anesthesia 8 HCPCS/CPT procedure code definition 8 CPT Manual or CMS manual coding instruction 8 Mutually exclusive procedures 9 Sequential procedure 9 CPT “Separate procedure” definition 9 More extensive procedure 9 Gender-specific procedures 10 Standards of medical/surgical practice 10 Anesthesia service included in surgical procedure 10 Laboratory panel 10 Deleted/modified edits for NCCI 11 Misuse of column two code with column one code 11 Medically Unlikely Edits (MUE) (Units of Service) 11 Deleted/modified edits -
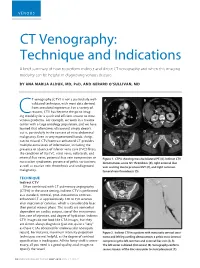
CT Venography: Technique and Indications
VENOUS CT Venography: Technique and Indications A brief summary of how to perform indirect and direct CT venography and when this imaging modality can be helpful in diagnosing venous disease. BY ANA MARIJA ALDUK, MD, PHD, AND GERARD O’SULLIVAN, MD T venography (CTV) is not a particularly well- A B validated technique, with most data derived from anecdotal experience. For a variety of reasons, CTV has become the go-to imag- Cing modality for a quick and efficient answer to most venous problems. For example, we work in a trauma center with a large oncology population, and we have learned that oftentimes ultrasound simply doesn’t cut it, particularly in the context of intra-abdominal C D malignancy. Even in very experienced hands, things can be missed. CTV/contrast-enhanced CT provides multiple extra levels of information, including the presence or absence of inferior vena cava (IVC) filters; the condition of the IVC, renal veins, collaterals, and internal iliac veins; potential iliac vein compression or Figure 1. CTPA showing massive bilateral PE (A). Indirect CTV nutcracker syndromes; presence of pelvic varicosities; demonstrates acute IVC thrombosis (B), right external iliac as well as ovarian vein thrombosis and undiagnosed vein scarring due to previous DVT (C), and right common malignancy. femoral vein thrombosis (D). TECHNIQUE A C Indirect CTV Often combined with CT pulmonary angiography (CTPA) in the acute setting, indirect CTV is performed as a standard, nonoral, post–intravenous contrast- enhanced CT at approximately 120 to 150 seconds after injection of contrast, which is considerably later than portal venous phase. -

2Nd Quarter 2001 Medicare Part a Bulletin
In This Issue... From the Intermediary Medical Director Medical Review Progressive Corrective Action ......................................................................... 3 General Information Medical Review Process Revision to Medical Record Requests ................................................ 5 General Coverage New CLIA Waived Tests ............................................................................................................. 8 Outpatient Hospital Services Correction to the Outpatient Services Fee Schedule ................................................................. 9 Skilled Nursing Facility Services Fee Schedule and Consolidated Billing for Skilled Nursing Facility (SNF) Services ............. 12 Fraud and Abuse Justice Recovers Record $1.5 Billion in Fraud Payments - Highest Ever for One Year Period ........................................................................................... 20 Bulletin Medical Policies Use of the American Medical Association’s (AMA’s) Current Procedural Terminology (CPT) Codes on Contractors’ Web Sites ................................................................................. 21 Outpatient Prospective Payment System January 2001 Update: Coding Information for Hospital Outpatient Prospective Payment System (OPPS) ......................................................................................................................... 93 he Medicare A Bulletin Providers Will Be Asked to Register Tshould be shared with all to Receive Medicare Bulletins and health care -

Bilateral Exudative Retinal Detachment in a Patient with Cerebral Venous Sinus Thrombosis: a Case Report
Bilateral exudative retinal detachment in a patient with cerebral venous sinus thrombosis: a case report Liang Li The second Xiangya Hospital, Central South University Ling Gao ( [email protected] ) Second Xiangya Hospital https://orcid.org/0000-0002-9850-2038 Case report Keywords: exudative retinal detachment, cerebral venous sinus thrombosis, elschnig spot, retinal capillary ischemia Posted Date: June 6th, 2019 DOI: https://doi.org/10.21203/rs.2.9789/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/8 Abstract Background: Cerebral venous sinus thrombosis (CVST) is a rare cerebrovascular disease, it’s ocular symptoms often characterized by a subacute bilateral visual loss, or diplopia and paralysis of eye movements. Fundus examination usually presents as bilateral papilledema and other ocular signs are rare. We report a case of bilateral multiple retinal detachments and nally diagnosed as CVST. Case presentation: A 49-year old woman with progressive headache and bilateral vision deterioration visited our clinic. Ophthaomological examinations including medical history, best-corrected visual acuity, intraocular pressure, slit-lamp biomicroscopy, fundus ophthalmoscopy, uorescein angiography and Optical coherence tomography and head Magnetic Resonance Venogram (MRV) was also performed. Blood tests for ruling out systemic diseases were also performed. Fundus exam revealed bilateral multiple retinal detachment with sub-retinal uid and blurred disc margin. Fluorescein angiography (FA) revealed early hypouorescence in the background stage, multiple pinpoint leakages at the level of retinal pigment epithelium (RPE), and late pooling to outline the boundary of retinal detachment, with some of the leakage shaped as multiple circles in the late stage of FA. -

Introduction
RIMS, IMPHAL ANNUAL REPORT 2014-15 INTRODUCTION 1. DESCRIPTION : The Regional Institute of Medical Sciences (RIMS), Imphal was established in the year 1972. It is an institution of regional importance catering to the needs of the North Eastern Region in the field of imparting undergraduate and post graduate medical education.The Institution brings together educational facilities for the training of personnel in all important branches of medical specialities including Dental and Nursing education in one place. The Institute is affiliated to the Manipur University, Canchipur, Imphal. 2. MANAGEMENT : The Institute was transferred to the Ministry of Health & Family Welfare, Government of India from North Eastern Council, Shillong (under Ministry of DoNER, Government of India) w.e.f. 1st April, 2007. Under the existing administrative set-up, the highest decision making body is the Board of Governors headed by the Union Minister of Health & Family Welfare as the President and the Director of the Institute as the Secretary. The Executive Council is responsible for the management of the Institute. The Secretary, Ministry of Health & Family Welfare, Government of India is the Chairman of the Executive Council while the head of the Institute remains as Secretary. Thus, the institute is managed at two levels, namely the Board of Governors and the Executive Council. A. Board of Governors : 1. Hon’ble Union Minister, - President Health & Family Welfare, Government of India. 2. Hon’ble Chief Minister, Manipur. - Vice-President 3. A Representative of the Planning Commission, - Member Government of India. 4. Health Ministers of the Beneficiary States - Member 5. Secretary, Ministry of Health & Family Welfare, - Member Government of India. -

(MRA) and Magnetic Resonance Venography (MRV) Medical Policy
Magnetic Resonance Angiography (MRA) and Magnetic Resonance Venography (MRV) Medical Policy The content of this document is used by plans that do not utilize NIA review. Service: Magnetic Resonance Angiography (MRA) and Magnetic Resonance Venography (MRV) PUM 250-0027-1712 Medical Policy Committee Approval 12/11/2020 Effective Date 01/01/2021 Prior Authorization Needed Yes Description: Magnetic Resonance Angiography (MRA) and Magnetic Resonance Venography (MRV) use Magnetic resonance imaging (MRI) technology to produce detailed 2-dimensional or 3- dimensional images of the vascular system and may be tailored to assess arteries or veins. It is often used for vascular conditions where other types of imaging are considered inferior or contraindicated, and to decrease risk of cumulative radiation exposure and often instead of invasive procedures. Indications of Coverage: A. MRA/MRV is considered medically necessary for the anatomical regions listed below when the specific indications or symptoms described are documented: 1. Head/Brain: a. Suspected intracranial aneurysm (ICA) or arteriovenous malformation (AVM). Any of the following: 1. Acute severe headache, severe exertional headache, or sudden onset of explosive headache, in individuals with signs / symptoms highly suggestive of a leaking/ruptured internal carotid artery or arteriovenous malformation. 2. Known subarachnoid hemorrhage or diagnosis of spontaneous intracerebral hemorrhage with concern for underlying vascular abnormality. 3. Suspected arteriovenous malformation (AVM) or dural AV fistula in an individual with prior indeterminate imaging study 4. Thunderclap headache with question of underlying vascular abnormality AND prior negative workup to include EITHER i. negative brain MRI, OR ii. Negative brain CT and negative lumbar puncture Page 1 of 15 5. -

Fluorescein and Indocyanine Green Angiography Guidelines ______
Fluorescein and Indocyanine Green Angiography Guidelines _______________________________________________________________________________ Approved by: Board Last reviews: 21 January 2012, 3 June 2015 Approval date: 2007 Next review: 3 June 2018 The Royal Australian and New Zealand College of Ophthalmologists ACN 000 644 404 94-98 Chalmers Street, Surry Hills NSW 2010 Phone: +61 2 9690 1001 Fax: +61 2 9690 1321 www.ranzco.edu Introduction and purpose These Guidelines have been issued by RANZCO for the guidance of ophthalmologists. They should not be used by any other persons or provided to patients as a replacement for medical advice. 1. Fluorescein angiography (FA) is an extremely useful and minimally invasive diagnostic investigation that is frequently performed in ophthalmologists’ private practices and ophthalmology departments. Indocyanine Green (ICG) angiography is a similar but less frequently performed investigation. Despite the generally low risks of the procedure, deaths have occurred during and following FA in both Australia and overseas. General 2. Guidelines in eye care are neither minimal nor aspirational but represent quality eye care commensurate with knowledge as at the date of issue. These Guidelines are based on the best available scientific data and on the collective judgement and evaluation of available evidence by retinal specialists in consultation with medico legal and medical (immunology) colleagues. 3. The Guidelines are for the pattern-of-practice rather than the care of a particular individual. While they may meet the needs of most patients, they cannot possibly meet the needs of all patients. 4. Adherence to these Guidelines will not ensure a successful outcome in every situation and the Guidelines should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably directed at obtaining the best results. -

Initial Observations Comparing MDCT and 3.0T MRI Findings with Autopsy Findings
Utility of Postmortem Autopsy via Whole- Body Imaging: Initial Observations Comparing MDCT and 3.0T MRI Findings with Autopsy Findings Jang Gyu Cha, MD1 Dong Hun Kim, MD1 Objective: We prospectively compared whole-body multidetector computed Dae Ho Kim, MD2 tomography (MDCT) and 3.0T magnetic resonance (MR) images with autopsy Sang Hyun Paik, MD1 findings. Jai Soung Park, MD1 Materials and Methods: Five cadavers were subjected to whole-body, 16- Seong Jin Park, MD1 channel MDCT and 3.0T MR imaging within two hours before an autopsy. A radi- Hae Kyung Lee, MD1 ologist classified the MDCT and 3.0T MRI findings into major and minor findings, Hyun Sook Hong, MD1 which were compared with autopsy findings. 3 Duek Lin Choi, MD Results: Most of the imaging findings, pertaining to head and neck, heart and 4 Kyung Moo Yang, MD vascular, chest, abdomen, spine, and musculoskeletal lesions, corresponded to 4 Nak Eun Chung, MD autopsy findings. The causes of death that were determined on the bases of 4 Bong Woo Lee, MD MDCT and 3.0T MRI findings were consistent with the autopsy findings in four of 4 Joong Seok Seo, MD five cases. CT was useful in diagnosing fatal hemorrhage and pneumothorax, as well as determining the shapes and characteristics of the fractures and the direc- Index terms: tion of external force. MRI was effective in evaluating and tracing the route of a Computed tomography (CT) metallic object, soft tissue lesions, chronicity of hemorrhage, and bone bruises. Magnetic resonance (MR) Whole-body imaging Conclusion: A postmortem MDCT combined with MRI is a potentially powerful Forensic autopsy tool, providing noninvasive and objective measurements for forensic investiga- DOI:10.3348/kjr.2010.11.4.395 tions.