Basketball and Volleyball
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

VOLLEYBALL Table of Contents (Click on an Item to Jump Directly to That Section) Page IMPORTANT DATES and DEADLINES
VOLLEYBALL Table of Contents (click on an item to jump directly to that section) Page IMPORTANT DATES AND DEADLINES ....................................................................................................... 3 STATE MEET SITES AND DATES .................................................................................................................. 3 STATE TOURNAMENT BRACKET ................................................................................................................ 4 RULE REVISIONS .............................................................................................................................................. 5 SOUTH DAKOTA CHANGES ........................................................................................................................... 5 SOUTH DAKOTA MODIFICATIONS ............................................................................................................. 6 GENERAL INFORMATION Classification and Alignments ....................................................................................................................... 6 On-Line Schedules and Rosters ...................................................................................................................... 6 Match Limitation ............................................................................................................................................. 6 Length of Sets & Matches/Match Format ................................................................................................... -
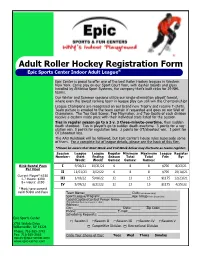
Inline Hockey Registration Form
Adult Roller Hockey Registration Form Epic Sports Center Indoor Adult League® Epic Center is proud to offer one of the best Roller Hockey leagues in Western New York. Come play on our Sport Court floor, with dasher boards and glass installed by Athletica Sport Systems, the company that’s built rinks for 29 NHL teams. Our Winter and Summer sessions utilize our single-elimination playoff format, where even the lowest ranking team in league play can still win the Championship! League Champions are recognized on our brand new Trophy and receive T-shirts. Team picture is emailed to the team captain if requested and goes on our Wall of Champions. The Top Goal Scorer, Top Playmaker, and Top Goalie of each division receive a custom made prize with their individual stats listed for the session. Ties in regular season go to a 3 v. 3 three-minute-overtime, then sudden death shootout. Ties in playoffs go to sudden death overtime. 3 points for a reg- ulation win. 0 points for regulation loss. 2 points for OT/shootout win. 1 point for OT/shootout loss. The AAU Rulebook will be followed, but Epic Center’s house rules supersede some of them. For a complete list of league details, please see the back of this flier. *Please be aware that Start Week and End Week below may fluctuate as teams register. Session League League Regular Minimum Maximum League Register Number: Start Ending Season Total Total Fee: By: Week: Week: Games: Games: Games: Rink Rental Fees I 9/06/21 10/31/21 6 8 8 $700 8/23/21 Per Hour II 11/01/21 1/02/22 6 8 8 $700 10/18/21 Current Player*:$150 -

A Study on Common Injuries in the Game of Volleyball IJPESH 2019; 6(1): 148-150 © 2019 IJPESH Dr
International Journal of Physical Education, Sports and Health 2019; 6(1): 148-150 P-ISSN: 2394-1685 E-ISSN: 2394-1693 Impact Factor (ISRA): 5.38 A study on common injuries in the game of volleyball IJPESH 2019; 6(1): 148-150 © 2019 IJPESH www.kheljournal.com Dr. Keshava Murthy T Received: 19-11-2018 Accepted: 21-12-2018 Abstract Top most position acquired in the field of competitive game as per the spectators concern that is soccer. Dr. Keshava Murthy T. Deputy Director of Physical Second position grasp in the game of volleyball at International level has one of the highest participation Education, Mangalore rates in worldwide, including both indoor and beach volleyball. It is one of the unique team sports that University, Mangalagangothri, has evolved into two distinct Olympic events–indoor and beach. Although injury patterns differ between Karnataka, India indoor and beach volleyball, there are similar injuries commonly seen between the two sports. Overall, overuse injuries are more common than acute injuries, because of the amount of repetition, improper technique, and type of playing surface. Overuse conditions of the knee, shoulder and lower back are not unusual in volleyball. Volleyball players repeatedly use their shoulders for spiking and blocking, overuse of injuries of the shoulder are common. Sprains and strains, most often around ankle, also occur. Finger injuries (phalanges), such as dislocations and tendon tears, frequently occur during setting and blocking in the game of volleyball. The researcher has the experience of more than 30 years in the game of volleyball, as a player, as a coach for the Mangalore University. -

2020-21 Sports Calendar
BOARD APPROVED - 2.1.2021 - DATES / EVENTS SUBJECT TO CHANGE February 2021 March 2021 February 2021 Su Mo Tu We Th Fr Sa Su Mo Tu We Th Fr Sa 123456 123456 7 8 910111213 7 8 9 10 11 12 13 14 15 16 17 18 19 20 14 15 16 17 18 19 20 21 22 23 24 25 26 27 21 22 23 24 25 26 27 28 28 29 30 31 SUNDAY MONDAY TUESDAY WEDNESDAY THURSDAY FRIDAY SATURDAY Jan 31 Feb 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 Football Practice Cross Country Cross Country Competitions Volleyball Practice Begin Volleyball Competitions Begin 28 Mar 1 2 3 4 5 6 1 4/12/2021 10:54 AM BOARD APPROVED - 2.1.2021 - DATES / EVENTS SUBJECT TO CHANGE March 2021 April 2021 March 2021 Su Mo Tu We Th Fr Sa Su Mo Tu We Th Fr Sa 123456 123 7 8 910111213 45678910 14 15 16 17 18 19 20 11 12 13 14 15 16 17 21 22 23 24 25 26 27 18 19 20 21 22 23 24 28 29 30 31 25 26 27 28 29 30 SUNDAY MONDAY TUESDAY WEDNESDAY THURSDAY FRIDAY SATURDAY Feb 28 Mar 1 2 3 4 5 6 Cross Country Volleyball Games Soccer Practice Soccer Games Football Practice Football Games 7 8 9 10 11 12 13 Cross Country Football Games Soccer Games Volleyball Games 14 15 16 17 18 19 20 Football Games Soccer Games Volleyball Games Cross Country Cross Country District Meets 21 22 23 24 25 26 27 12:00am Cross Country Entries Football Games Due Soccer Games Spirit Practice Volleyball Games Basketball Practice Basketball Games Cross Country Championships 28 29 30 31 Apr 1 2 3 Basketball Games Final Football Week Soccer Games Volleyball Championships Wrestling Practice Spirit Practice 2 4/12/2021 10:54 AM BOARD -

Northwestern State Intramurals COVID VOLLEYBALL/BASKETBALL GUIDELINES 1
Northwestern State Intramurals COVID VOLLEYBALL/BASKETBALL GUIDELINES 1. All sign ups must be done on IMleagues prior to the event. All rosters must be filled out in their entirety to verify student eligibility. You must show your student ID to play but will not turn in your student ID to staff. 2. Intramural Staff & Participants’ temperature will be checked upon entry into the gym. Only one door will be used for entry. 3. Only players and coaches on rosters will be allowed in the gym during scheduled game/match times. NO fans or extra guests will be allowed in the gym during game/match times. All players and coaches should exit facility immediately at the conclusion of play. 4. Games/matches will be scheduled with an extra 15 minutes apart to allow facility to clear. 5. Only one basketball game and one volleyball game will be scheduled at a time. 6. Student IDs will not be collected during the games/matches but must be shown upon entry of the gym. 7. Pinnies and jerseys will not be distributed by Intramural Staff. Teams must provide their own jerseys with numbers to play. 8. No group huddles between teams will be permitted on the court. NO handshakes at the end of the game. NO high fives during the game. 9. No early warmup is allowed in the facility while scheduled games are playing. Teams will be afforded a 10-minute warmup once they are allowed in the gym. This may be modified and reduced to accommodate the schedule. FACE COVERING PROTOCOLS ALL players and coaches MUST always wear a protective face covering when entering the gym. -

17 SEP 14 N,L1 :32 SENATE
SEVENTEENTH CONGRESS OF THE ) REPUBLIC OF THE PHILIPPINES ) Second Regular Session ) ■17 SEP 14 n,l1 :32 SENATE P.S. Res. No.'r,')^ KlCl.'1. , Introduced by SENATOR SONNY ANGARA RESOLUTION EXPRESSING THE SUPPORT OF THE SENATE OF THE PHILIPPINES TO THE SAMAHANG BASKETBOL NG PILIPINAS (SBP) IN THEIR EFFORTS TO SPEARHEAD THE PHILIPPINES’ BID TO HOST THE 2023 FIBA WORLD CUP WHEREAS, since its inception in 1932, theFederation Internationale de Basketball (International Basketball Federation) or FIBA has been the world’s governing body for basketball and is recognized as the sole competent authority in basketball by the International Olympic Committee (IOC); WHEREAS, FIBA organizes and oversees international competitions which include the Olympic Basketball Tournament, the 3x3 Basketball, and the organization’s flagship event - the FIBA Basketball World Cup; WHEREAS, through these tournaments and events, FIBA brings together 213 National Basketball Federations from all over the world, including the Philippines which has been a memberof the organization since 1936; WHEREAS, based on the FIBA World Ranking, the Philippines ranks 43rd out of the 132 countries. The country also ranks 6,h out of the 32 Asian countries participating in FIBA tournaments, ahead of countries such as India, Malaysia, Thailand, Jordan, Lebanon, Indonesia, Singapore, United Arab Emirates, and the Kingdom of Saudi Arabia to name a few;1 WHEREAS, with the upcoming 2023 FIBA World Cup, the FIBA governing body will allow the provision of multiple countries hosting the group -

ADULT SPORTS FAQ's 1. What Are the Age Requirements for Participation in Adult Sports Programs?
ADULT SPORTS FAQ’s 1. What are the age requirements for participation in Adult Sports programs? Volleyball participants must be at least 16 years of age during the season in order to be eligible. Basketball, Dodgeball, Flag-Football, and Softball participants must be at least 18 years of age during the season in order to be eligible. The age difference in adult sports programs is due to the potential level of physical contact during league play. 2. Are uniforms required in team sports participation? Team uniforms are not required for our volleyball or softball leagues. Basketball, Dodgeball, and Flag-Football teams, however, must wear same color shirts with permanent numbers placed on the back. All teams provide their own equipment. Game balls are provided only in the softball program. 3. Why are the fees so high for the adult leagues? League fees are used to pay for scorekeepers, staffing, facility maintenance and equipment. Awards are also given to the top two teams in each division. Compared to other communities, our fees are still considerably affordable. YOUTH SPORTS FAQ’s 1. What are the age requirements for participation in Youth Sports programs? Children learn at various stages and must learn all the skills necessary before advancing to a higher level. It is recommended that participants sign up according to the grade or age limit assigned to a particular program. The Instructor may then recommend a participant to be moved to a more advanced level if the participant is physically and cognitively ready. 2. My child will meet the proper age limit in a couple of months. -

A/B Grade Level: 9-10-11-12 773800 This Semester-Long Course Includes In
HEALTH AND PHYSICAL EDUCATION DEPARTMENT TEAM SPORTS: A/B Grade Level: 9-10-11-12 773800 This semester-long course includes instruction in two or three activity units per quarter. Each unit offers opportunities for student growth in health enhancing fitness activities, movement skills and concepts of personal and social responsibility. Students will apply the knowledge of components and principles in health- and skill-related fitness when creating a personal fitness plan. Units of study in team sports may include hockey, flag football, ultimate Frisbee, team handball, soccer, basketball, softball, volleyball, Tchoukball or other team sports chosen by the instructor. Unlimited repeats for subject credit VOLLEYBALL: A/B Grade Level: 9-10-11-12 775131/775132 This course is designed for volleyball players of all ability levels to develop necessary volleyball skills to participate for life. Zero previous volleyball experience is required. Throughout the semester students will participate in volleyball related fitness activities in addition to the gameplay and skill development. The first quarter of the course will emphasize skill development, with a moderate amount of time for game play. The second quarter of the course will emphasize game play, strategies, and tactics with a moderate amount of time for skill development. The course requires excellent sportsmanship as we want all classmates to feel encouraged to participate no matter their skill level and enjoy their class time. Unlimited repeats for subject credit NET/RACKET SPORTS: A/B Grade Level: 9-10-11-12 773700 This course is designed for students of all ability levels to develop necessary racket sport skills to participate for life. -

Wilson Ball Cleaning Recommendations
What chemicals can clean our game balls without altering performance? Our primary recommendation is to follow CDC, state and local guidelines for health and safety. The following widely accepted definitions are relevant to composite leather, PU leather, and leather game ball care (CDC reference): There are several different methods for sanitizing and disinfecting composite leather, PU leather, and leather game product. Each customer should utilize the method that fits their health and safety protocols and the playing environment and timing needs. Simple Game Ball Cleaning Method To clean the ball, players may wish to use dish soap and water. While this practice may be likened to hand washing, note that all soap residue must be rinsed away and that drying time on each ball product may vary. An example cleaning regimen with soap and water includes: 1. Add 1 tablespoon of mild dish soap into a 1-gallon container. 2. Fill bucket with warm water, until a soapy mixture is formed. 3. Wet a first towel with the solution, wring out excess water, and gently wipe down entire product surface for at least 30 seconds. 4. Re-wet towel with plain warm water, wring out excess water, and wipe off excess soap from ball surface. 5. Rub a second, dry towel on the surface to wipe and dry off. 6. Let product air out overnight. Quick Turn Leather Game Ball Cleaning Method To clean the ball with faster turnaround times, we reference the following recommendations. The CDC released a list (referred to as ‘List N’) of effective disinfectants for disabling SARS-CoV-2 (i.e., the virus that causes Covid-19 disease) on hard, nonporous surfaces. -

Team Handball Study Guide
MIDDLE SCHOOL PE TEAM HANDBALL STUDY GUIDE Although popular throughout much of the world, team handball is just starting in the United States. The sport uses natural athletic skills such as running, jumping, throwing and catching to provide action for the game. Spectators describe team handball as soccer with your hands, but they also notice things that remind them of basketball, water polo and ice hockey. Team handball is one of the world’s fastest team games. Two sides of seven players, including the goalie, play it. The object is to score the most goals by throwing the ball into the opponent’s goal and attackers pass or dribble the ball with their hands until a shooting opportunity is created. When a team loses possession of the ball, that team goes on defense. HOW A GAME STARTS: A Throw-off is taken from half-court. Every player must be in his/her own half of the field and opponents must be 10 feet from the thrower until the ball is thrown. MOVING THE BALL: Passing the ball is the best way to move the ball. A player may also dribble the ball as is done in basketball. A player may take only 3 steps while holding the ball. He/she may then dribble the ball, stop dribbling, and take 3 more steps. Once a player stops moving, he/she has 3 seconds to throw the ball. He/she may dribble the ball once with one hand while running. A player may bounce or roll the ball to another player. A player may roll the ball with one hand along the ground. -

Basketball Rules
Basketball Rules 1. Each team consists of five players. Basketball is played by two teams. The purpose of each team is to throw the ball into it’s own basket and to prevent the other team from scoring. 2. A goal is made when a live ball enters the basket from above and passes through. A goal from the field counts 2 points for the team into whose basket the ball is thrown. A goal from a free throw attempt is credited to the thrower and counts 1 point for his or her team. A goal made from beyond the 3-point arc counts 3 points . 3. Jump Ball – This play takes place in the center of the court to start the game. The referee tosses the ball up between two opposing players. Players try to out-jump each other and tap the ball to a teammate. 4. Violation – Minor rule infraction such as: • Traveling – taking more than one step before passing or dribbling the ball. • Stepping out of bounds. • Throwing the ball out of bounds. • Double Dribble – dribbling, stopping the dribble, and starting the dribble again; dribbling the ball with both hands for more than one dribble. • 3 Seconds – offensive player with or without the ball may not be in the lane for more than 3 seconds. • Over and Back – once the ball has crossed over the center line, the offense may not go back over it. • Palming the Ball – permitting the ball to come to rest in one hand while dribbling. * On a violation the other team gains possession of the ball on the sideline or baseline. -
Youth Player Development Programmes
LITHUANIAN BASKETBALL FEDERATION 2nd Seminar for National Federations FIBA Europe, Munich, 2009 Youth Player Development Programmes LBF Secretary general Mindaugas Balciunas MAIN REASONS OF THE BASKETBALL SUCCESS IN LITHUANIA General popularity of the Well organized training process basketball sport (Well educated coaches, good infrastructure, good local (Historical victories, exceptional attention of the Government, competitional system) huge media cover, Nr 1 kind of sport in Lithuania) LITHUANIAN BASKETBALL SUCCESS Productive general management system Very good selection (All the segments involved in the management, small country (Most talanted kids coming to the basketball, wide net of is advantage in the development, system based on basketball schools, clubs and etc., many local competitions) autonomical associations) LITHUANIAN BASKETBALL FEDERATION GENERAL MANAGEMENT STRUCTURE All members of LBF: basketball clubs, General Conference schools,schools, associations,associations, townstowns federations etc. Composed of representatives of 4 Men’s, 2 Executive Board Women’s leagues, Coaches and Referees associations, Youth and Veterans leagues Elected by the General Conference for four LBF President year period Approved by the Executive Board under LBF Secretary General recommendation of the President LBF Administration Employed by the President and Secretary General LITHUANIAN BASKETBALL FEDERATION MANAGEMENT STRUCTURE LBF President Secretary general Office Commerci Youth NT Project’s Media Accounting administrato al director managers