The Ciliary Ganglion Story – Prelude to Synapse the Oculomotor Nerve Carries Preganglionic Parasympathetic Fibers Into the Orbit
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
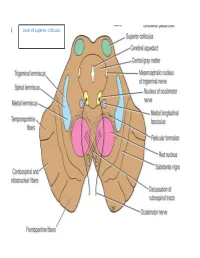
Level of Superior Colliculus ° Edinger- Westphal Nucleus ° Pretectal Nucleus: Close to the Lateral Part of the Superior Colliculus
Level of superior colliculus ° Edinger- Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. Red nucleus • Rounded mass of gray matter • Situated bt cerebral aqueduct and substantia nigra • Reddish blue(vascularity & iron containing pigment) • Afferents from: cerebral cortex,cerebellum,substa ntia nigra, thalamic nuclei, spinal cord • Efferent to: spinal cord, reticular formation. thalamus and substantia nigra • involved in motor coordination. Crus cerebri • Corticospinal & corticonuclear fibers (middle) • Frontopontine fibers (medial) • Temporopontine fibers (lateral) these descending tracts connect the cerebral cortex with spinal cord, cranial nerves nuclei, pons & cerebellum Level at superior colliculus ° Superior colliculus ° Occulomotor nucleus (posterior to MLF) ° Occulomotor n emerges through red nucleus ° Edinger-Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. ° MLF ° Medial , trigeminal, spinal leminiscus ( no lateral leminiscus) ° Red nucleus ° Substantia nigra ° Crus cerebri ° RF Substantia nigra ° Large motor nucleus ° is a brain structure located in the midbrain ° plays an important role in reward, addiction, and movement. ° Substantia nigra is Latin for "black substance" due to high levels of melanin ° has connections with basal ganglia ,cerebral cortex ° Concerned with muscle tone ° Parkinson's disease is caused by the death of neurons in the substantia nigra Oculomotor Nerve (III) • Main oculomotor nucleus • Accessory parasympathetic nucleus -

Cranial Nerves 9Th & 10Th
Cranial Nerves 9th & 10th Neuroanatomy block-Anatomy-Lecture 8 Editing file Objectives At the end of the lecture, students should be able to: ● Define the deep origin of both Glossopharyngeal and Vagus Nerves. ● Locate the exit of each nerve from the brain stem. ● Describe the course and distribution of each nerve . ● List the branches of both nerves. Color guide ● Only in boys slides in Green ● Only in girls slides in Purple ● important in Red ● Notes in Grey Glossopharyngeal (IX) 9th Cranial Nerve ● it's mixed nerve, a Sensory nerve with preganglionic parasympathetic and few motor fibers ● It has no real nucleus to itself. Instead it shares nuclei with VII (facial) and X (vagus). Superficial attachment Course ● It arises from the ventral aspect of the 1. It Passes forwards between medulla by a linear series of small Internal jugular vein and rootlets, in groove between olive and External carotid artery. inferior cerebellar peduncle. ● It leaves the cranial cavity by passing 2. Lies Deep to Styloid process. through the jugular foramen in company with the Vagus , and the Accessory 3. Passes between external and nerves and the Internal jugular vein. internal carotid arteries at the posterior border of Stylopharyngeus then lateral to it. 4. It reaches the pharynx by passing between middle and inferior constrictors, deep to Hyoglossus, where it breaks into terminal branches. 3 Glossopharyngeal (IX) 9th Cranial Nerve Ganglia & Communications ● Small with no branches. Superior Ganglion ● It is connected to the Superior Cervical sympathetic ganglion. ● Large and carries general sensations from pharynx, soft palate and tonsil. Inferior ● ganglion It is connected to Auricular Branch of Vagus. -

Nerves of the Orbit Optic Nerve the Optic Nerve Enters the Orbit from the Middle Cranial Fossa by Passing Through the Optic Canal
human anatomy 2016 lecture fourteen Dr meethak ali ahmed neurosurgeon Nerves of the Orbit Optic Nerve The optic nerve enters the orbit from the middle cranial fossa by passing through the optic canal . It is accompanied by the ophthalmic artery, which lies on its lower lateral side. The nerve is surrounded by sheath of pia mater, arachnoid mater, and dura mater. It runs forward and laterally within the cone of the recti muscles and pierces the sclera at a point medial to the posterior pole of the eyeball. Here, the meninges fuse with the sclera so that the subarachnoid space with its contained cerebrospinal fluid extends forward from the middle cranial fossa, around the optic nerve, and through the optic canal, as far as the eyeball. A rise in pressure of the cerebrospinal fluid within the cranial cavity therefore is transmitted to theback of the eyeball. Lacrimal Nerve The lacrimal nerve arises from the ophthalmic division of the trigeminal nerve. It enters the orbit through the upper part of the superior orbital fissure and passes forward along the upper border of the lateral rectus muscle . It is joined by a branch of the zygomaticotemporal nerve, whi(parasympathetic secretomotor fibers). The lacrimal nerve ends by supplying the skin of the lateral part of the upper lid. Frontal Nerve The frontal nerve arises from the ophthalmic division of the trigeminal nerve. It enters the orbit through the upper part of the superior orbital fissure and passes forward on the upper surface of the levator palpebrae superioris beneath the roof of the orbit . -

Neuroanatomy Crash Course
Neuroanatomy Crash Course Jens Vikse ∙ Bendik Myhre ∙ Danielle Mellis Nilsson ∙ Karoline Hanevik Illustrated by: Peder Olai Skjeflo Holman Second edition October 2015 The autonomic nervous system ● Division of the autonomic nervous system …………....……………………………..………….…………... 2 ● Effects of parasympathetic and sympathetic stimulation…………………………...……...……………….. 2 ● Parasympathetic ganglia ……………………………………………………………...…………....………….. 4 Cranial nerves ● Cranial nerve reflexes ………………………………………………………………….…………..…………... 7 ● Olfactory nerve (CN I) ………………………………………………………………….…………..…………... 7 ● Optic nerve (CN II) ……………………………………………………………………..…………...………….. 7 ● Pupillary light reflex …………………………………………………………………….…………...………….. 7 ● Visual field defects ……………………………………………...................................…………..………….. 8 ● Eye dynamics …………………………………………………………………………...…………...………….. 8 ● Oculomotor nerve (CN III) ……………………………………………………………...…………..………….. 9 ● Trochlear nerve (CN IV) ………………………………………………………………..…………..………….. 9 ● Trigeminal nerve (CN V) ……………………………………………………................…………..………….. 9 ● Abducens nerve (CN VI) ………………………………………………………………..…………..………….. 9 ● Facial nerve (CN VII) …………………………………………………………………...…………..………….. 10 ● Vestibulocochlear nerve (CN VIII) …………………………………………………….…………...…………. 10 ● Glossopharyngeal nerve (CN IX) …………………………………………….……….…………...………….. 10 ● Vagus nerve (CN X) …………………………………………………………..………..…………...………….. 10 ● Accessory nerve (CN XI) ……………………………………………………...………..…………..………….. 11 ● Hypoglossal nerve (CN XII) …………………………………………………..………..…………...…………. -

The Sympathetic and the Parasympathetic Nervous System
The sympathetic and the parasympathetic nervous system Zsuzsanna Tóth, PhD Institute of Anatomy, Histology and Embryology Semmelweis University The role of the autonomic nervous system Claude Bernard • „milieu intérieur” concept; every organism lives in its internal environment that is constant and independent form the external environment Walter Bradford Cannon homeostasis; • an extension of the “milieu interieur” concept • consistence in an open system requires mechanisms that act to maintain that consistency • steady-state conditions require that any tendency toward change automatically meets with factors that resist that change • regulating systems that determine the homeostatic state : o autonomic nervous system ( sympathetic, parasympathetic, enteral) o endocrine system General structure of the autonomic nervous system craniosacral thoracolumbar Anatomy Neurotransmittersof the gut autonomic nervous system. symp. gangl pregangl. fiber pregangl. postgangl. fiber fiber (PoR) PoR enteral ganglion PoR PoR smooth muscle smooth muscle Kuratani S Development 2009;136:1585-1589 Sympathetic activation: Fight or flight reaction • energy mobilization • preparation for escape, or fight vasoconstriction • generalized Parasympathetic activation: adrenal • energy saving and restoring • „rest and digest” system • more localized vasoconstriction Paravertebral ganglia and the sympathetic chains pars cervicalis superius ganglion medium cervicale stellatum pars vertebrae • from the base of the skull to the caudal end thoracalis thoracalis of the sacrum • paravertebral ganglia (ganglia trunci sympathici) • rami interganglionares pars vertebrae • the two chains fuses at the ganglion impar abdominalis lumbalis sacrum pars pelvina foramen sacralia anteriora ganglion impar Anatomy of the cervical part of the sympathetic trunk superior cervical ganglion • behind the seath of the carotid, fusiform ggl. cervicale superius • IML T1-3 vegetative motoneurons- preganglionic fibers truncus symp. -

Simple Ways to Dissect Ciliary Ganglion for Orbital Anatomical Education
OkajimasDetection Folia Anat. of ciliary Jpn., ganglion94(3): 119–124, for orbit November, anatomy 2017119 Simple ways to dissect ciliary ganglion for orbital anatomical education By Ming ZHOU, Ryoji SUZUKI, Hideo AKASHI, Akimitsu ISHIZAWA, Yoshinori KANATSU, Kodai FUNAKOSHI, Hiroshi ABE Department of Anatomy, Akita University Graduate School of Medicine, Akita, 010-8543 Japan –Received for Publication, September 21, 2017– Key Words: ciliary ganglion, orbit, human anatomy, anatomical education Summary: In the case of anatomical dissection as part of medical education, it is difficult for medical students to find the ciliary ganglion (CG) since it is small and located deeply in the orbit between the optic nerve and the lateral rectus muscle and embedded in the orbital fat. Here, we would like to introduce simple ways to find the CG by 1): tracing the sensory and parasympathetic roots to find the CG from the superior direction above the orbit, 2): transecting and retracting the lateral rectus muscle to visualize the CG from the lateral direction of the orbit, and 3): taking out whole orbital structures first and dissecting to observe the CG. The advantages and disadvantages of these methods are discussed from the standpoint of decreased laboratory time and students as beginners at orbital anatomy. Introduction dissection course for the first time and with limited time. In addition, there are few clear pictures in anatomical The ciliary ganglion (CG) is one of the four para- textbooks showing the morphology of the CG. There are sympathetic ganglia in the head and neck region located some scientific articles concerning how to visualize the behind the eyeball between the optic nerve and the lateral CG, but they are mostly based on the clinical approaches rectus muscle in the apex of the orbit (Siessere et al., rather than based on the anatomical procedure for medical 2008). -

Anatomical Study of the Zygomaticotemporal Branch Inside the Orbit
Open Access Original Article DOI: 10.7759/cureus.1727 Anatomical Study of the Zygomaticotemporal Branch Inside the Orbit Joe Iwanaga 1 , Charlotte Wilson 1 , Koichi Watanabe 2 , Rod J. Oskouian 3 , R. Shane Tubbs 4 1. Seattle Science Foundation 2. Department of Anatomy, Kurume University School of Medicine 3. Neurosurgery, Complex Spine, Swedish Neuroscience Institute 4. Neurosurgery, Seattle Science Foundation Corresponding author: Charlotte Wilson, [email protected] Abstract The location of the opening of the zygomaticotemporal branch (ZTb) of the zygomatic nerve inside the orbit (ZTFIN) has significant surgical implications. This study was conducted to locate the ZTFIN and investigate the variations of the ZTb inside the orbit. A total of 20 sides from 10 fresh frozen cadaveric Caucasian heads were used in this study. The vertical distance between the inferior margin of the orbit and ZTFIN (V-ZTFIN), the horizontal distance between the lateral margin of the orbit and ZTFIN (H-ZTFIN), and the diameter of the ZTFIN (D-ZTFIN) were measured. The patterns of the ZTb inside the orbit were classified into five different groups: both ZTb and LN innervating the lacrimal gland independently (Group A), both ZTb and LN innervating the lacrimal gland with a communicating branch (Group B), ZTb joining the LN without a branch to the lacrimal gland (Group C), the ZTb going outside the orbit through ZTFIN without a branch to the lacrimal gland nor LN (Group D), and absence of the ZTb (Group E). The D-ZTFIN V-ZTFIN H-ZTFIN ranged from 0.2 to 1.1 mm, 6.6 to 21.5 mm, 2.0 to 11.3 mm, respectively. -

Extracranial Course of Cranial Nerves
Extracranial course of cranial nerves Oculomotor, Trochlear, Abducent, Trigeminal, Facial and Accessory nerves Dr. Heba Kalbouneh Associate Professor of Anatomy and Histology Dr. Heba Kalbouneh Brainstem Mid brain Pons Medulla Pons Inferior view Facial nerve Anatomically, the course of the facial nerve can be divided into two parts: Motor: Innervates the muscles of facial Intracranial – the course of the nerve through expression, the posterior belly of the the cranial cavity, and the cranium itself. digastric, the stylohyoid and the stapedius Extracranial – the course of the nerve outside muscles. the cranium, through the face and neck. General Sensory: A small area around the concha of the auricle, EAM Special Sensory: Provides special taste sensation to the anterior 2/3 of the tongue. Parasympathetic: Supplies many of the glands of the head and neck, including: 1- Submandibular and sublingual salivary glands (via the submandibular ganglion/ chorda tympani) 2- Nasal, palatine and pharyngeal mucous glands (via the pterygopalatine ganglion/ greater petrosal) 3- Lacrimal glands (via the pterygopalatine ganglion/ greater petrosal) Dr. Heba Kalbouneh Intracranial course The nerve arises in the pons. It begins as two roots; a large motor root, and a small sensory root The two roots travel through the internal acoustic meatus. Pons Here, they are in very close proximity to the inner ear. 7th (motor) 8th Note: The part of the facial nerve that runs between the motor root of facial and vestibulocochlear nerve is sometimes Kalbouneh known as the nervus intermedius It contains the sensory and parasympathetic Heba fibers of the facial nerve Dr. Dr. Still within the temporal bone, the roots leave the internal acoustic meatus, and enter into the facial canal. -

The Mandibular Nerve - Vc Or VIII by Prof
The Mandibular Nerve - Vc or VIII by Prof. Dr. Imran Qureshi The Mandibular nerve is the third and largest division of the trigeminal nerve. It is a mixed nerve. Its sensory root emerges from the posterior region of the semilunar ganglion and is joined by the motor root of the trigeminal nerve. These two nerve bundles leave the cranial cavity through the foramen ovale and unite immediately to form the trunk of the mixed mandibular nerve that passes into the infratemporal fossa. Here, it runs anterior to the middle meningeal artery and is sandwiched between the superior head of the lateral pterygoid and tensor veli palatini muscles. After a short course during which a meningeal branch to the dura mater, and the nerve to part of the medial pterygoid muscle (and the tensor tympani and tensor veli palatini muscles) are given off, the mandibular trunk divides into a smaller anterior and a larger posterior division. The anterior division receives most of the fibres from the motor root and distributes them to the other muscles of mastication i.e. the lateral pterygoid, medial pterygoid, temporalis and masseter muscles. The nerve to masseter and two deep temporal nerves (anterior and posterior) pass laterally above the medial pterygoid. The nerve to the masseter continues outward through the mandibular notch, while the deep temporal nerves turn upward deep to temporalis for its supply. The sensory fibres that it receives are distributed as the buccal nerve. The 1 | P a g e buccal nerve passes between the medial and lateral pterygoids and passes downward and forward to emerge from under cover of the masseter with the buccal artery. -

Morphometry and Morphology of Foramen Petrosum in Indian Population
Basic Sciences of Medicine 2020, 9(1): 8-9 DOI: 10.5923/j.medicine.20200901.02 Morphometry and Morphology of Foramen Petrosum in Indian Population Rajani Singh1,*, Nand Kishore Gupta1, Raj Kumar2 1Department of Anatomy, Uttar Pradesh University of Medical Sciences Saifai 206130 Etawah UP India 2Department of Neurosugery Uttar Pradesh University of Medical Sciences Saifai 206130 Etawah UP India Abstract Greater wing of sphenoid contains three constant foramina, Foramen ovale, foramen rotundum and foramen spinosum. The presence of foramen Vesalius and foramen petrosum are inconsistent. Normally foramen ovale transmits mandibular nerve, accessory meningeal artery, lesser petrosal nerve and emissary vein. When foramen petrosum is present, lesser petrosal nerve passes through petrosal foramen instead of foramen ovale. Lesser petrosal nerve distribute postganglionic fibers from otic ganglion to parotid gland. In absence of knowledge of petrosal foramen transmitting lesser petrosal nerve, the clinician may damage the nerve during skull base surgery creating complications like hyperemia of face and profuse salivation from the parotid gland (following atropine administration), lacrimation (crocodile tears syndrome) and mucus nasal secretion. Considering clinical implications associated with petrosal foramen, the study was carried out. The aim of the study is to determine the prevalence of petrosal foramen in Indian Population and to bring out associated clinical significance. The study was conducted in the department of Anatomy UPUMS Saifai Etawah Indian. 30 half skulls were observed for the presence of petrosal foramina and morphometry was also done. Literature search was carried out, our findings were compared with previous work and associated clinical implications were bought out. Keywords Petrosal foramen, Lesser petrosal nerve, Foramen ovale patients. -

Oculoplastics/Orbit 2017-2019
Academy MOC Essentials® Practicing Ophthalmologists Curriculum 2017–2019 Oculoplastics and Orbit *** Oculoplastics/Orbit 2 © AAO 2017-2019 Practicing Ophthalmologists Curriculum Disclaimer and Limitation of Liability As a service to its members and American Board of Ophthalmology (ABO) diplomates, the American Academy of Ophthalmology has developed the Practicing Ophthalmologists Curriculum (POC) as a tool for members to prepare for the Maintenance of Certification (MOC) -related examinations. The Academy provides this material for educational purposes only. The POC should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably directed at obtaining the best results. The physician must make the ultimate judgment about the propriety of the care of a particular patient in light of all the circumstances presented by that patient. The Academy specifically disclaims any and all liability for injury or other damages of any kind, from negligence or otherwise, for any and all claims that may arise out of the use of any information contained herein. References to certain drugs, instruments, and other products in the POC are made for illustrative purposes only and are not intended to constitute an endorsement of such. Such material may include information on applications that are not considered community standard, that reflect indications not included in approved FDA labeling, or that are approved for use only in restricted research settings. The FDA has stated that it is the responsibility of the physician to determine the FDA status of each drug or device he or she wishes to use, and to use them with appropriate patient consent in compliance with applicable law. -

ANATOMY of EAR Basic Ear Anatomy
ANATOMY OF EAR Basic Ear Anatomy • Expected outcomes • To understand the hearing mechanism • To be able to identify the structures of the ear Development of Ear 1. Pinna develops from 1st & 2nd Branchial arch (Hillocks of His). Starts at 6 Weeks & is complete by 20 weeks. 2. E.A.M. develops from dorsal end of 1st branchial arch starting at 6-8 weeks and is complete by 28 weeks. 3. Middle Ear development —Malleus & Incus develop between 6-8 weeks from 1st & 2nd branchial arch. Branchial arches & Development of Ear Dev. contd---- • T.M at 28 weeks from all 3 germinal layers . • Foot plate of stapes develops from otic capsule b/w 6- 8 weeks. • Inner ear develops from otic capsule starting at 5 weeks & is complete by 25 weeks. • Development of external/middle/inner ear is independent of each other. Development of ear External Ear • It consists of - Pinna and External auditory meatus. Pinna • It is made up of fibro elastic cartilage covered by skin and connected to the surrounding parts by ligaments and muscles. • Various landmarks on the pinna are helix, antihelix, lobule, tragus, concha, scaphoid fossa and triangular fossa • Pinna has two surfaces i.e. medial or cranial surface and a lateral surface . • Cymba concha lies between crus helix and crus antihelix. It is an important landmark for mastoid antrum. Anatomy of external ear • Landmarks of pinna Anatomy of external ear • Bat-Ear is the most common congenital anomaly of pinna in which antihelix has not developed and excessive conchal cartilage is present. • Corrections of Pinna defects are done at 6 years of age.