The Age of Phage: Friend Or Foe in the New Dawn of Therapeutic and Biocontrol Applications?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mobile Genetic Elements in Streptococci
Curr. Issues Mol. Biol. (2019) 32: 123-166. DOI: https://dx.doi.org/10.21775/cimb.032.123 Mobile Genetic Elements in Streptococci Miao Lu#, Tao Gong#, Anqi Zhang, Boyu Tang, Jiamin Chen, Zhong Zhang, Yuqing Li*, Xuedong Zhou* State Key Laboratory of Oral Diseases, National Clinical Research Center for Oral Diseases, West China Hospital of Stomatology, Sichuan University, Chengdu, PR China. #Miao Lu and Tao Gong contributed equally to this work. *Address correspondence to: [email protected], [email protected] Abstract Streptococci are a group of Gram-positive bacteria belonging to the family Streptococcaceae, which are responsible of multiple diseases. Some of these species can cause invasive infection that may result in life-threatening illness. Moreover, antibiotic-resistant bacteria are considerably increasing, thus imposing a global consideration. One of the main causes of this resistance is the horizontal gene transfer (HGT), associated to gene transfer agents including transposons, integrons, plasmids and bacteriophages. These agents, which are called mobile genetic elements (MGEs), encode proteins able to mediate DNA movements. This review briefly describes MGEs in streptococci, focusing on their structure and properties related to HGT and antibiotic resistance. caister.com/cimb 123 Curr. Issues Mol. Biol. (2019) Vol. 32 Mobile Genetic Elements Lu et al Introduction Streptococci are a group of Gram-positive bacteria widely distributed across human and animals. Unlike the Staphylococcus species, streptococci are catalase negative and are subclassified into the three subspecies alpha, beta and gamma according to the partial, complete or absent hemolysis induced, respectively. The beta hemolytic streptococci species are further classified by the cell wall carbohydrate composition (Lancefield, 1933) and according to human diseases in Lancefield groups A, B, C and G. -

Horizontal Gene Transfer
Genetic Variation: The genetic substrate for natural selection Horizontal Gene Transfer Dr. Carol E. Lee, University of Wisconsin Copyright ©2020; Do not upload without permission What about organisms that do not have sexual reproduction? In prokaryotes: Horizontal gene transfer (HGT): Also termed Lateral Gene Transfer - the lateral transmission of genes between individual cells, either directly or indirectly. Could include transformation, transduction, and conjugation. This transfer of genes between organisms occurs in a manner distinct from the vertical transmission of genes from parent to offspring via sexual reproduction. These mechanisms not only generate new gene assortments, they also help move genes throughout populations and from species to species. HGT has been shown to be an important factor in the evolution of many organisms. From some basic background on prokaryotic genome architecture Smaller Population Size • Differences in genome architecture (noncoding, nonfunctional) (regulatory sequence) (transcribed sequence) General Principles • Most conserved feature of Prokaryotes is the operon • Gene Order: Prokaryotic gene order is not conserved (aside from order within the operon), whereas in Eukaryotes gene order tends to be conserved across taxa • Intron-exon genomic organization: The distinctive feature of eukaryotic genomes that sharply separates them from prokaryotic genomes is the presence of spliceosomal introns that interrupt protein-coding genes Small vs. Large Genomes 1. Compact, relatively small genomes of viruses, archaea, bacteria (typically, <10Mb), and many unicellular eukaryotes (typically, <20 Mb). In these genomes, protein-coding and RNA-coding sequences occupy most of the genomic sequence. 2. Expansive, large genomes of multicellular and some unicellular eukaryotes (typically, >100 Mb). In these genomes, the majority of the nucleotide sequence is non-coding. -
Transduction by Bacteriophage Ti * Henry Drexler
Proceedings of the National Academy of Sciences Vol. 66, No. 4, pp. 1083-1088, August 1970 Transduction by Bacteriophage Ti * Henry Drexler DEPARTMENT OF MICROBIOLOGY, BOWMAN GRAY SCHOOL OF MEDICINE, WAKE FOREST UNIVERSITY, WINSTON-SALEM, NORTH CAROLINA Communicated by Edward L. Tatum, May 25, 1970 Abstract. Amber mutants of the virulent coliphage T1 are able to transduce a wide variety of genetic characteristics from permissive to nonpermissive K strains of Escherichia coli. The virulent coliphage T1 is not known to be related to any temperate phage. Certain of the characteristics of T1 seem to be incompatible with its potential existence as a temperate phage; for example, the average latent period for T1 is only 13 min' and about 70% of its DNA is derived from the host.2 In order to demonstrate transduction by T1 it is necessray to provide condi- tions in which potential transductants are able to survive; this is accomplished by using amber mutants of T1 to transduce nonpermissive recipients. Experi- ments which show that T1 is a transducing phage are presented and have been designed chiefly to illustrate the following points: (1) Infection by T1 is able to cause heritable changes in recipients; (2) the genotype of the donor host is im- portant in determining what characteristics can be transferred to recipients; (3) the changes in the recipients are not caused by transformation; and (4) there is a similarity between the transducing activity and the plaque-forming ability of T1 with respect to serology, host range, and density. Materials and Methods. Bacterial strains: The abbreviations and symbols of Demerec et al.3 and Taylor and Trotter4 are used to describe all pertinent genotypes. -
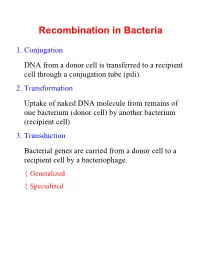
Recombination in Bacteria
Recombination in Bacteria 1. Conjugation DNA from a donor cell is transferred to a recipient cell through a conjugation tube (pili). 2. Transformation Uptake of naked DNA molecule from remains of one bacterium (donor cell) by another bacterium (recipient cell). 3. Transduction Bacterial genes are carried from a donor cell to a recipient cell by a bacteriophage. { Generalized { Specialized Conjugation Ability to conjugate located on the F-plasmid F+ Cells act as donors F- Cells act as recipients F+/F- Conjugation: { F Factor “replicates off” a single strand of DNA. { New strand goes through pili to recipient cell. { New strand is made double stranded. { If entire F-plasmid crosses, then recipient cell becomes F+, otherwise nothing happens Conjugation with Hfr Hfr cell (High Frequency Recombination) cells have F-plasmid integrated into the Chromosome. Integration into the Chromosome is unique for each F-plasmid strain. When F-plasmid material is replicated and sent across pili, Chromosomal material is included. (Figure 6.10 in Klug & Cummings) When chromosomal material is in recipient cell, recombination can occur: { Recombination is double stranded. { Donor genes are recombined into the recipient cell. { Corresponding genes from recipient cell are recombined out of the chromosome and reabsorbed by the cell. Interrupted Mating Mapping 1. Allow conjugation to start Genes closest to the origin of replication site (in the direction of replication) are moved through the pili first. 2. After a set time, interrupt conjugation Only those genes closest to the origin of replication site will conjugate. The long the time, the more that is able to conjugate. 3. -

Microbial Genetics by Dr Preeti Bajpai
Dr. Preeti Bajpai Genes: an overview ▪ A gene is the functional unit of heredity ▪ Each chromosome carry a linear array of multiple genes ▪ Each gene represents segment of DNA responsible for synthesis of RNA or protein product ▪ A gene is considered to be unit of genetic information that controls specific aspect of phenotype DNA Chromosome Gene Protein-1 Prokaryotic Courtesy: Team Shrub https://twitter.com/realscientists/status/927 cell 667237145767937 Genetic exchange within Prokaryotes The genetic exchange occurring in bacteria involve transfers of genes from one bacterium to another. The gene transfer in prokaryotic cells is thus unidirectional and the recombination events usually occur between a fragment of one chromosome (from a donor cell) and a complete chromosome (in a recipient cell) Mechanisms for genetic exchange Bacteria exchange genetic material through three different parasexual processes* namely transformation, conjugation and transduction. *Parasexual process involves recombination of genes from genetically distinct cells occurring without involvement of meiosis and fertilization Principles of Genetics-sixth edition Courtesy: Beatrice the Biologist.com by D. Peter Snustad & Michael J. Simmons (http://www.beatricebiologist.com/2014/08/bacterial-gifts/) Transformation: an introduction Transformation involves the uptake of free DNA molecules released from one bacterium (the donor cell) by another bacterium (the recipient cell). Frederick Griffith discovered transformation in Streptococcus pneumoniae (pneumococcus) in 1928. In his experiments, Griffith used two related strains of bacteria, known as R and S. The R bacteria (nonvirulent) formed colonies, or clumps of related bacteria, that Frederick Griffith 1877-1941 had a rough appearance (hence the abbreviation "R"). The S bacteria (virulent) formed colonies that were rounded and smooth (hence the abbreviation "S"). -

Bacteria Definitions.Pdf
Antibiotic -- a type of antimicrobial substance active against bacteria Archae-bacteria -- microorganisms that are similar to bacteria in size and simplicity of structure but radically different in molecular organization Bacilli -- a taxonomic class of bacteria that includes two orders, Bacillales and Lactobacillales Bacillus anthracis -- the cause of anthrax Bacteria – ubiquitous one-celled organisms involved in fermentation, putrefaction, infectious diseases, and nitrogen fixation Bacteriophage -- a virus that infects and replicates within bacteria and archaea Binary fission -- the process that bacteria use to carry out cell division Capsid – structure that encloses a virus’ nucleic acid Chemo-heterotroph -- an organism that derives its energy from chemicals, and needs to consume other organisms in order to live Class -- A taxonomic group comprised of organisms that share a common attribute Cocci – spherical bacteria Conjugation – temporary union of two bacteria Coronavirus -- when viewed under an electron microscopic each virion in this type of virus is surrounded by a halo Domain -- the highest taxonomic rank of organisms Endospore – spore formed within a cell of a rod-shaped organism Eubacteria -- single-celled prokaryotic microorganisms that have a range of characteristics and are found in various conditions throughout all parts of the world. All types of bacteria fall under this title, except for archaebacteria Eykaryote -- organisms whose cells have a nucleus enclosed within a nuclear envelope Family -- A taxonomic rank in the -

Jewels in the Crown
Jewels in the crown CSHL’s 8 Nobel laureates Eight scientists who have worked at Cold Max Delbrück and Salvador Luria Spring Harbor Laboratory over its first 125 years have earned the ultimate Beginning in 1941, two scientists, both refugees of European honor, the Nobel Prize for Physiology fascism, began spending their summers doing research at Cold or Medicine. Some have been full- Spring Harbor. In this idyllic setting, the pair—who had full-time time faculty members; others came appointments elsewhere—explored the deep mystery of genetics to the Lab to do summer research by exploiting the simplicity of tiny viruses called bacteriophages, or a postdoctoral fellowship. Two, or phages, which infect bacteria. Max Delbrück and Salvador who performed experiments at Luria, original protagonists in what came to be called the Phage the Lab as part of the historic Group, were at the center of a movement whose members made Phage Group, later served as seminal discoveries that launched the revolutionary field of mo- Directors. lecular genetics. Their distinctive math- and physics-oriented ap- Peter Tarr proach to biology, partly a reflection of Delbrück’s physics train- ing, was propagated far and wide via the famous Phage Course that Delbrück first taught in 1945. The famous Luria-Delbrück experiment of 1943 showed that genetic mutations occur ran- domly in bacteria, not necessarily in response to selection. The pair also showed that resistance was a heritable trait in the tiny organisms. Delbrück and Luria, along with Alfred Hershey, were awarded a Nobel Prize in 1969 “for their discoveries concerning the replication mechanism and the genetic structure of viruses.” Barbara McClintock Alfred Hershey Today we know that “jumping genes”—transposable elements (TEs)—are littered everywhere, like so much Alfred Hershey first came to Cold Spring Harbor to participate in Phage Group wreckage, in the chromosomes of every organism. -

Phylogenomic Networks Reveal Limited Phylogenetic Range of Lateral Gene Transfer by Transduction
The ISME Journal (2017) 11, 543–554 OPEN © 2017 International Society for Microbial Ecology All rights reserved 1751-7362/17 www.nature.com/ismej ORIGINAL ARTICLE Phylogenomic networks reveal limited phylogenetic range of lateral gene transfer by transduction Ovidiu Popa1, Giddy Landan and Tal Dagan Institute of General Microbiology, Christian-Albrechts University of Kiel, Kiel, Germany Bacteriophages are recognized DNA vectors and transduction is considered as a common mechanism of lateral gene transfer (LGT) during microbial evolution. Anecdotal events of phage- mediated gene transfer were studied extensively, however, a coherent evolutionary viewpoint of LGT by transduction, its extent and characteristics, is still lacking. Here we report a large-scale evolutionary reconstruction of transduction events in 3982 genomes. We inferred 17 158 recent transduction events linking donors, phages and recipients into a phylogenomic transduction network view. We find that LGT by transduction is mostly restricted to closely related donors and recipients. Furthermore, a substantial number of the transduction events (9%) are best described as gene duplications that are mediated by mobile DNA vectors. We propose to distinguish this type of paralogy by the term autology. A comparison of donor and recipient genomes revealed that genome similarity is a superior predictor of species connectivity in the network in comparison to common habitat. This indicates that genetic similarity, rather than ecological opportunity, is a driver of successful transduction during microbial evolution. A striking difference in the connectivity pattern of donors and recipients shows that while lysogenic interactions are highly species-specific, the host range for lytic phage infections can be much wider, serving to connect dense clusters of closely related species. -

Comprehensive Analysis of Mobile Genetic Elements in the Gut Microbiome Reveals Phylum-Level Niche-Adaptive Gene Pools
bioRxiv preprint doi: https://doi.org/10.1101/214213; this version posted December 22, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Comprehensive analysis of mobile genetic elements in the gut microbiome 2 reveals phylum-level niche-adaptive gene pools 3 Xiaofang Jiang1,2,†, Andrew Brantley Hall2,3,†, Ramnik J. Xavier1,2,3,4, and Eric Alm1,2,5,* 4 1 Center for Microbiome Informatics and Therapeutics, Massachusetts Institute of Technology, 5 Cambridge, MA 02139, USA 6 2 Broad Institute of MIT and Harvard, Cambridge, MA 02142, USA 7 3 Center for Computational and Integrative Biology, Massachusetts General Hospital and Harvard 8 Medical School, Boston, MA 02114, USA 9 4 Gastrointestinal Unit and Center for the Study of Inflammatory Bowel Disease, Massachusetts General 10 Hospital and Harvard Medical School, Boston, MA 02114, USA 11 5 MIT Department of Biological Engineering, Massachusetts Institute of Technology, Cambridge, MA 12 02142, USA 13 † Co-first Authors 14 * Corresponding Author bioRxiv preprint doi: https://doi.org/10.1101/214213; this version posted December 22, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 15 Abstract 16 Mobile genetic elements (MGEs) drive extensive horizontal transfer in the gut microbiome. This transfer 17 could benefit human health by conferring new metabolic capabilities to commensal microbes, or it could 18 threaten human health by spreading antibiotic resistance genes to pathogens. Despite their biological 19 importance and medical relevance, MGEs from the gut microbiome have not been systematically 20 characterized. -
![Max Ludwig Henning Delbruck (1906–1981) [1]](https://docslib.b-cdn.net/cover/0999/max-ludwig-henning-delbruck-1906-1981-1-560999.webp)
Max Ludwig Henning Delbruck (1906–1981) [1]
Published on The Embryo Project Encyclopedia (https://embryo.asu.edu) Max Ludwig Henning Delbruck (1906–1981) [1] By: Hernandez, Victoria Max Ludwig Henning Delbrück applied his knowledge of theoretical physics to biological systems such as bacterial viruses called bacteriophages, or phages, and gene replication during the twentieth century in Germany and the US. Delbrück demonstrated that bacteria undergo random genetic mutations to resist phage infections. Those findings linked bacterial genetics to the genetics of higher organisms. In the mid-twentieth century, Delbrück helped start the Phage Group and Phage Course in the US, which further organized phage research. Delbrück also contributed to the DNA replication debate that culminated in the 1958 Meselson-Stahl experiment, which demonstrated how organisms replicate their genetic information. For his work with phages, Delbrück earned part of the 1969 Nobel Prize for Physiology or Medicine. Delbrück's work helped shape and establish new fields in molecular biology and genetics to investigate the laws of inheritance and development. Delbrück was born on 4 September 1906, as the last of seven children of Lina and Hans Delbrück, in Berlin, Germany. Delbrück grew up in Grunewald, a suburb of Berlin. In 1914, World War I [2] began. During the war, Delbrück's family struggled with food shortages and in 1917 Delbrück's oldest brother died in combat. After the war ended in 1918, Delbrück began to study astronomy. Some nights, Delbrück woke up in the middle of the night to observe the stars with his telescope. He also read about the seventeenth-century astronomer Johannes Kepler, who studied planetary motion in late sixteenth and early seventeenth century Germany. -

Martha Chase Dies
PublisherInfo PublisherName : BioMed Central PublisherLocation : London PublisherImprintName : BioMed Central Martha Chase dies ArticleInfo ArticleID : 4830 ArticleDOI : 10.1186/gb-spotlight-20030820-01 ArticleCitationID : spotlight-20030820-01 ArticleSequenceNumber : 182 ArticleCategory : Research news ArticleFirstPage : 1 ArticleLastPage : 4 RegistrationDate : 2003–8–20 ArticleHistory : OnlineDate : 2003–8–20 ArticleCopyright : BioMed Central Ltd2003 ArticleGrants : ArticleContext : 130594411 Milly Dawson Email: [email protected] Martha Chase, renowned for her part in the pivotal "blender experiment," which firmly established DNA as the substance that transmits genetic information, died of pneumonia on August 8 in Lorain, Ohio. She was 75. In 1952, Chase participated in what came to be known as the Hershey-Chase experiment in her capacity as a laboratory assistant to Alfred D. Hershey. He won a Nobel Prize for his insights into the nature of viruses in 1969, along with Max Delbrück and Salvador Luria. Peter Sherwood, a spokesman for Cold Spring Harbor Laboratory, where the work took place, described the Hershey-Chase study as "one of the most simple and elegant experiments in the early days of the emerging field of molecular biology." "Her name would always be associated with that experiment, so she is some sort of monument," said her longtime friend Waclaw Szybalski, who met her when he joined Cold Spring Harbor Laboratory in 1951 and who is now a professor of oncology at the University of Wisconsin-Madison. Szybalski attended the first staff presentation of the Hershey-Chase experiment and was so impressed that he invited Chase for dinner and dancing the same evening. "I had an impression that she did not realize what an important piece of work that she did, but I think that I convinced her that evening," he said. -

Management of Animal Botulism Outbreaks: from Clinical Suspicion to Practical Countermeasures to Prevent Or Minimize Outbreaks
Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science Volume 11, Supplement 1, 2013 ª Mary Ann Liebert, Inc. DOI: 10.1089/bsp.2012.0089 Management of Animal Botulism Outbreaks: From Clinical Suspicion to Practical Countermeasures to Prevent or Minimize Outbreaks Fabrizio Anniballi, Alfonsina Fiore, Charlotta Lo¨fstro¨m, Hanna Skarin, Bruna Auricchio, Ce´dric Woudstra, Luca Bano, Bo Segerman, Miriam Koene, Viveca Ba˚verud, Trine Hansen, Patrick Fach, Annica Tevell A˚berg, Mikael Hedeland, Eva Olsson Engvall, and Dario De Medici Botulism is a severe neuroparalytic disease that affects humans, all warm-blooded animals, and some fishes. The disease is caused by exposure to toxins produced by Clostridium botulinum and other botulinum toxin–producing clostridia. Botulism in animals represents a severe environmental and economic concern because of its high mortality rate. Moreover, meat or other products from affected animals entering the food chain may result in a publichealthproblem.Tothisend,earlydiagnosisiscrucialto define and apply appropriate veterinary public health measures. Clinical diagnosis is based on clinical findings eliminating other causes of neuromuscular disorders and on the absence of internal lesions observed during postmortem examination. Since clinical signs alone are often insufficient to make a definitive diagnosis, laboratory confirmation is required. Botulinum antitoxin administration and supportive therapies are used to treat sick animals. Once the diagnosis has been made, euthanasia is frequently advisable. Vaccine administration is subject to health authorities’ permission, and it is restricted to a small number of animal species. Several measures can be adopted to prevent or minimize outbreaks. In this article we outline all phases of management of animal botulism outbreaks occurring in wet wild birds, poultry, cattle, horses, and fur farm animals.