Personality Differences Between Patients with Lichen Simplex
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Diagnostic Approach to Pruritus
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by DigitalCommons@University of Nebraska University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln U.S. Air Force Research U.S. Department of Defense 2011 A Diagnostic Approach to Pruritus Brian V. Reamy Christopher W. Bunt Stacy Fletcher Follow this and additional works at: https://digitalcommons.unl.edu/usafresearch This Article is brought to you for free and open access by the U.S. Department of Defense at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in U.S. Air Force Research by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. A Diagnostic Approach to Pruritus BRIAN V. REAMY, MD, Uniformed Services University of the Health Sciences, Bethesda, Maryland CHRISTOPHER W. BUNT, MAJ, USAF, MC, and STACY FLETCHER, CAPT, USAF, MC Ehrling Bergquist Family Medicine Residency Program, Offutt Air Force Base, Nebraska, and the University of Nebraska Medical Center, Omaha, Nebraska Pruritus can be a symptom of a distinct dermatologic condition or of an occult underlying systemic disease. Of the patients referred to a dermatologist for generalized pruritus with no apparent primary cutaneous cause, 14 to 24 percent have a systemic etiology. In the absence of a primary skin lesion, the review of systems should include evaluation for thyroid disorders, lymphoma, kidney and liver diseases, and diabetes mellitus. Findings suggestive of less seri- ous etiologies include younger age, localized symptoms, acute onset, involvement limited to exposed areas, and a clear association with a sick contact or recent travel. Chronic or general- ized pruritus, older age, and abnormal physical findings should increase concern for underly- ing systemic conditions. -
Hyperhidrosis: Sweating out the Details
Focus on CME at the Université de Montréal Hyperhidrosis: Sweating Out the Details Antranik Benohanian, MD, FRCPC; and Nowell Solish, MD, FRCPC Presented at the 250th meeting of the Montreal Dermatological Society, April 2003 yperhidrosis (HH) remains a relatively Table 1 Hunknown disorder to the general public Most commonly affected sites and health-care professionals. According to the literature, 0.5% to 1% of the population is Site Prevalence affected by HH. However, a recent survey held Facial 68.9% in the U.S. places that figure at 2.8%; thus, Axillary 50.8% revealing that the prevalence is underrated. Plantar 28.7% Among those affected, only 38% had discussed Palmar 24.8% the problem with a health professional.1 HH may be classified as primary or sec- ondary; either type can be localized or gen- Besides affecting quality of life, HH predis- eralized. Table 1 lists the most commonly poses its victims to a host of dermatologic dis- affected sites. orders (Table 2).3 The control of HH would also control the associated disease condition, as has Impact on quality of life been recently reported with the treatment of dyshidrotic hand dermatitis with intradermal HH is known to be a socially embarrassing and botulinum toxin.4 occupationally disabling disorder. Many patients suffer in silence. Figure 1 illustrates the How is HH treated? impact HH has on quality of life.2 Those with axillary HH often have to change Systemic approach clothing several times a day and throw out Minor sedatives, such as amitriptyline and clothing because of the damage caused to fabric hydroxyzine, produce an anticholinergic, as and leather. -

ORIGINAL ARTICLE a Clinical and Histopathological Study of Lichenoid Eruption of Skin in Two Tertiary Care Hospitals of Dhaka
ORIGINAL ARTICLE A Clinical and Histopathological study of Lichenoid Eruption of Skin in Two Tertiary Care Hospitals of Dhaka. Khaled A1, Banu SG 2, Kamal M 3, Manzoor J 4, Nasir TA 5 Introduction studies from other countries. Skin diseases manifested by lichenoid eruption, With this background, this present study was is common in our country. Patients usually undertaken to know the clinical and attend the skin disease clinic in advanced stage histopathological pattern of lichenoid eruption, of disease because of improper treatment due to age and sex distribution of the diseases and to difficulties in differentiation of myriads of well assess the clinical diagnostic accuracy by established diseases which present as lichenoid histopathology. eruption. When we call a clinical eruption lichenoid, we Materials and Method usually mean it resembles lichen planus1, the A total of 134 cases were included in this study prototype of this group of disease. The term and these cases were collected from lichenoid used clinically to describe a flat Bangabandhu Sheikh Mujib Medical University topped, shiny papular eruption resembling 2 (Jan 2003 to Feb 2005) and Apollo Hospitals lichen planus. Histopathologically these Dhaka (Oct 2006 to May 2008), both of these are diseases show lichenoid tissue reaction. The large tertiary care hospitals in Dhaka. Biopsy lichenoid tissue reaction is characterized by specimen from patients of all age group having epidermal basal cell damage that is intimately lichenoid eruption was included in this study. associated with massive infiltration of T cells in 3 Detailed clinical history including age, sex, upper dermis. distribution of lesions, presence of itching, The spectrum of clinical diseases related to exacerbating factors, drug history, family history lichenoid tissue reaction is wider and usually and any systemic manifestation were noted. -

Common Dermatoses in Patients with Obsessive Compulsive Disorders Mircea Tampa Carol Davila University of Medicine and Pharmacy, Tampa [email protected]
Journal of Mind and Medical Sciences Volume 2 | Issue 2 Article 7 2015 Common Dermatoses in Patients with Obsessive Compulsive Disorders Mircea Tampa Carol Davila University of Medicine and Pharmacy, [email protected] Maria Isabela Sarbu Victor Babes Hospital for Infectious and Tropical Diseases, [email protected] Clara Matei Carol Davila University of Medicine and Pharmacy Vasile Benea Victor Babes Hospital for Infectious and Tropical Diseases Simona Roxana Georgescu Carol Davila University of Medicine and Pharmacy Follow this and additional works at: http://scholar.valpo.edu/jmms Part of the Medicine and Health Sciences Commons Recommended Citation Tampa, Mircea; Sarbu, Maria Isabela; Matei, Clara; Benea, Vasile; and Georgescu, Simona Roxana (2015) "Common Dermatoses in Patients with Obsessive Compulsive Disorders," Journal of Mind and Medical Sciences: Vol. 2 : Iss. 2 , Article 7. Available at: http://scholar.valpo.edu/jmms/vol2/iss2/7 This Review Article is brought to you for free and open access by ValpoScholar. It has been accepted for inclusion in Journal of Mind and Medical Sciences by an authorized administrator of ValpoScholar. For more information, please contact a ValpoScholar staff member at [email protected]. JMMS 2015, 2(2): 150- 158. Review Common dermatoses in patients with obsessive compulsive disorders Mircea Tampa1, Maria Isabela Sarbu2, Clara Matei1, Vasile Benea2, Simona Roxana Georgescu1 1 Carol Davila University of Medicine and Pharmacy, Department of Dermatology and Venereology 2 Victor Babes Hospital for Infectious and Tropical Diseases, Department of Dermatology and Venereology Corresponding author: Maria Isabela Sarbu, e-mail: [email protected] Running title: Dermatoses in obsessive compulsive disorders Keywords: Factitious disorders, obsessive-compulsive disorders, acne excoriee www.jmms.ro 2015, Vol. -

Lichen Simplex Chronicus
LICHEN SIMPLEX CHRONICUS http://www.aocd.org Lichen simplex chronicus is a localized form of lichenified (thickened, inflamed) atopic dermatitis or eczema that occurs in well defined plaques. It is the result of ongoing, chronic rubbing and scratching of the skin in localized areas. It is generally seen in patients greater than 20 years of age and is more frequent in women. Emotional stress can play a part in the course of this skin disease. There is mainly one symptom: itching. The rubbing and scratching that occurs in response to the itch can become automatic and even unconscious making it very difficult to treat. It can be magnified by seeming innocuous stimuli such as putting on clothes, or clothes rubbing the skin which makes the skin warmer resulting in increased itch sensation. The lesions themselves are generally very well defined areas of thickened, erythematous, raised area of skin. Frequently they are linear, oval or round in shape. Sites of predilection include the back of the neck, ankles, lower legs, upper thighs, forearms and the genital areas. They can be single lesions or multiple. This can be a very difficult condition to treat much less resolve. It is of utmost importance that the scratching and rubbing of the skin must stop. Treatment is usually initiated with topical corticosteroids for larger areas and intralesional steroids might also be considered for small lesion(s). If the patient simply cannot keep from rubbing the area an occlusive dressing might be considered to keep the skin protected from probing fingers. Since this is not a histamine driven itch phenomena oral antihistamines are generally of little use in these cases. -

Triamcinolone Acetonide Injectable Suspension, USP)
KENALOG®-10 INJECTION (triamcinolone acetonide injectable suspension, USP) NOT FOR USE IN NEONATES CONTAINS BENZYL ALCOHOL For Intra-articular or Intralesional Use Only NOT FOR INTRAVENOUS, INTRAMUSCULAR, INTRAOCULAR, EPIDURAL, OR INTRATHECAL USE DESCRIPTION Kenalog®-10 Injection (triamcinolone acetonide injectable suspension, USP) is triamcinolone acetonide, a synthetic glucocorticoid corticosteroid with marked anti-inflammatory action, in a sterile aqueous suspension suitable for intralesional and intra-articular injection. THIS FORMULATION IS SUITABLE FOR INTRA-ARTICULAR AND INTRALESIONAL USE ONLY. Each mL of the sterile aqueous suspension provides 10 mg triamcinolone acetonide, with 0.66% sodium chloride for isotonicity, 0.99% (w/v) benzyl alcohol as a preservative, 0.63% carboxymethylcellulose sodium, and 0.04% polysorbate 80. Sodium hydroxide or hydrochloric acid may have been added to adjust pH between 5.0 and 7.5. At the time of manufacture, the air in the container is replaced by nitrogen. The chemical name for triamcinolone acetonide is 9-Fluoro-11β,16α,17,21-tetrahydroxypregna- 1,4-diene-3,20-dione cyclic 16,17-acetal with acetone. Its structural formula is: 1 Reference ID: 4241593 MW 434.50 CLINICAL PHARMACOLOGY Glucocorticoids, naturally occurring and synthetic, are adrenocortical steroids that are readily absorbed from the gastrointestinal tract. Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt- retaining properties, are used as replacement therapy in adrenocortical deficiency states. -

Fundamentals of Dermatology Describing Rashes and Lesions
Dermatology for the Non-Dermatologist May 30 – June 3, 2018 - 1 - Fundamentals of Dermatology Describing Rashes and Lesions History remains ESSENTIAL to establish diagnosis – duration, treatments, prior history of skin conditions, drug use, systemic illness, etc., etc. Historical characteristics of lesions and rashes are also key elements of the description. Painful vs. painless? Pruritic? Burning sensation? Key descriptive elements – 1- definition and morphology of the lesion, 2- location and the extent of the disease. DEFINITIONS: Atrophy: Thinning of the epidermis and/or dermis causing a shiny appearance or fine wrinkling and/or depression of the skin (common causes: steroids, sudden weight gain, “stretch marks”) Bulla: Circumscribed superficial collection of fluid below or within the epidermis > 5mm (if <5mm vesicle), may be formed by the coalescence of vesicles (blister) Burrow: A linear, “threadlike” elevation of the skin, typically a few millimeters long. (scabies) Comedo: A plugged sebaceous follicle, such as closed (whitehead) & open comedones (blackhead) in acne Crust: Dried residue of serum, blood or pus (scab) Cyst: A circumscribed, usually slightly compressible, round, walled lesion, below the epidermis, may be filled with fluid or semi-solid material (sebaceous cyst, cystic acne) Dermatitis: nonspecific term for inflammation of the skin (many possible causes); may be a specific condition, e.g. atopic dermatitis Eczema: a generic term for acute or chronic inflammatory conditions of the skin. Typically appears erythematous, -

“The Red Face” and More Clinical Pearls
“The Red Face” and More Clinical Pearls Courtney R. Schadt, MD, FAAD Assistant Professor Residency Program Director University of Louisville Associates in Dermatology I have no disclosures or conflicts of interest Part 1: The Red Face: Objectives • Distinguish and diagnose common eruptions of the face • Recognize those with potential implications for internal disease • Learn basic treatment options Which patient(s) has an increased risk of hypertension and hyperlipidemia? A B C Which patient(s) has an increased risk of hypertension and hyperlipidemia? A Seborrheic Dermatitis B C Psoriasis Seborrheic Dermatitis Goodheart HP. Goodheart's photoguide of common skin disorders, 2nd ed, Lippincott Williams & Wilkins, Philadelphia 2003. Copyright © 2003 Lippincott Williams & Wilkins. Seborrheic Dermatitis • Erythematous scaly eruption • Infants= “Cradle Cap” • Reappear in adolescence or later in life • Chronic, remissions and flares; worse with stress, cold weather • Occurs on areas of body with increased sebaceous glands • Unclear role of Malassezia; could be immune response; no evidence of overgrowth Seborrheic Dermatitis Severe Seb Derm: THINK: • HIV (can also be more diffuse on trunk) • Parkinson’s (seb derm improves with L-dopa therapy) • Other neurologic disorders • Neuroleptic agents • Unclear etiology 5MinuteClinicalConsult Clinical Exam • Erythema/fine scale • Scalp • Ears • Nasolabial folds • Beard/hair bearing areas Goodheart HP. Goodheart's photoguide of common skin disorders, 2nd ed, Lippincott • Ill-defined Williams & Wilkins, Philadelphia -

Therapies for Common Cutaneous Fungal Infections
MedicineToday 2014; 15(6): 35-47 PEER REVIEWED FEATURE 2 CPD POINTS Therapies for common cutaneous fungal infections KENG-EE THAI MB BS(Hons), BMedSci(Hons), FACD Key points A practical approach to the diagnosis and treatment of common fungal • Fungal infection should infections of the skin and hair is provided. Topical antifungal therapies always be in the differential are effective and usually used as first-line therapy, with oral antifungals diagnosis of any scaly rash. being saved for recalcitrant infections. Treatment should be for several • Topical antifungal agents are typically adequate treatment weeks at least. for simple tinea. • Oral antifungal therapy may inea and yeast infections are among the dermatophytoses (tinea) and yeast infections be required for extensive most common diagnoses found in general and their differential diagnoses and treatments disease, fungal folliculitis and practice and dermatology. Although are then discussed (Table). tinea involving the face, hair- antifungal therapies are effective in these bearing areas, palms and T infections, an accurate diagnosis is required to ANTIFUNGAL THERAPIES soles. avoid misuse of these or other topical agents. Topical antifungal preparations are the most • Tinea should be suspected if Furthermore, subsequent active prevention is commonly prescribed agents for dermatomy- there is unilateral hand just as important as the initial treatment of the coses, with systemic agents being used for dermatitis and rash on both fungal infection. complex, widespread tinea or when topical agents feet – ‘one hand and two feet’ This article provides a practical approach fail for tinea or yeast infections. The pharmacol- involvement. to antifungal therapy for common fungal infec- ogy of the systemic agents is discussed first here. -
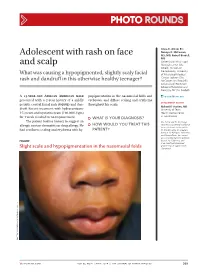
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Chronic Pruritic Vulva Lesion
Photo RoUNDS Stephen Colden Cahill, DO Chronic pruritic vulva lesion College of Osteopathic Medicine, Michigan State University, East Lansing; The patient was not sexually active and denied any and Lakeshore Health vaginal discharge. So what was causing the intense Partners, Holland, Mich itching on her labia? [email protected] Department eDItOr richard p. Usatine, mD University of Texas Health Science Center at San Antonio During a routine exam, a 45-year-old Cau- both of her labia majora (FIGURE). Throughout casian woman complained of intense itching the lesion, there were scattered areas of exco- The author reported no potential conflict of interest on her labia. She said that the itching had been riation. Her labia minor were spared. relevant to this article. an issue for more than 9 months and that she A speculum and bimanual exam were found herself scratching several times a day. normal. No inguinal lymphadenopathy was She denied any vaginal discharge and said she present. hadn’t been sexually active in years. She had tried over-the-counter antifungals and topical ● WhaT is your diagnosis? Benadryl, but they provided only limited relief. The patient had red thickened plaques ● HoW Would you TREAT THIS with accentuated skin lines (furrows) covering PATIENT? Figure Red thickened plaques on labia majora p ho T o cour T esy of: St ephen c olden c ahill, DO jfponline.com Vol 62, no 2 | february 2013 | The journal of family pracTice 97 PHOTO RoUNDS Diagnosis: taneous lesion of unknown etiology. It can Lichen simplex chronicus be found throughout the body, including the This patient was given a diagnosis of lichen mucous membranes. -

Or Moisture-Associated Skin Damage, Due to Perspiration: Expert Consensus on Best Practice
A Practical Approach to the Prevention and Management of Intertrigo, or Moisture-associated Skin Damage, due to Perspiration: Expert Consensus on Best Practice Consensus panel R. Gary Sibbald MD Professor, Medicine and Public Health University of Toronto Toronto, ON Judith Kelley RN, BSN, CWON Henry Ford Hospital – Main Campus Detroit, MI Karen Lou Kennedy-Evans RN, FNP, APRN-BC KL Kennedy LLC Tucson, AZ Chantal Labrecque RN, BSN, MSN CliniConseil Inc. Montreal, QC Nicola Waters RN, MSc, PhD(c) Assistant Professor, Nursing Mount Royal University A supplement of Calgary, AB The development of this consensus document has been supported by Coloplast. Editorial support was provided by Joanna Gorski of Prescriptum Health Care Communications Inc. This supplement is published by Wound Care Canada and is available at www.woundcarecanada.ca. All rights reserved. Contents may not be reproduced without written permission of the Canadian Association of Wound Care. © 2013. 2 Wound Care Canada – Supplement Volume 11, Number 2 · Fall 2013 Contents Introduction ................................................................... 4 Complications of Intertrigo ......................................11 Moisture-associated skin damage Secondary skin infection ...................................11 and intertrigo ................................................................. 4 Organisms in intertrigo ..............................11 Consensus Statements ................................................ 5 Specific types of infection .................................11