Therapies for Common Cutaneous Fungal Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Estimated Burden of Serious Fungal Infections in Ghana
Journal of Fungi Article Estimated Burden of Serious Fungal Infections in Ghana Bright K. Ocansey 1, George A. Pesewu 2,*, Francis S. Codjoe 2, Samuel Osei-Djarbeng 3, Patrick K. Feglo 4 and David W. Denning 5 1 Laboratory Unit, New Hope Specialist Hospital, Aflao 00233, Ghana; [email protected] 2 Department of Medical Laboratory Sciences, School of Biomedical and Allied Health Sciences, College of Health Sciences, University of Ghana, P.O. Box KB-143, Korle-Bu, Accra 00233, Ghana; [email protected] 3 Department of Pharmaceutical Sciences, Faculty of Health Sciences, Kumasi Technical University, P.O. Box 854, Kumasi 00233, Ghana; [email protected] 4 Department of Clinical Microbiology, School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi 00233, Ghana; [email protected] 5 National Aspergillosis Centre, Wythenshawe Hospital and the University of Manchester, Manchester M23 9LT, UK; [email protected] * Correspondence: [email protected] or [email protected] or [email protected]; Tel.: +233-277-301-300; Fax: +233-240-190-737 Received: 5 March 2019; Accepted: 14 April 2019; Published: 11 May 2019 Abstract: Fungal infections are increasingly becoming common and yet often neglected in developing countries. Information on the burden of these infections is important for improved patient outcomes. The burden of serious fungal infections in Ghana is unknown. We aimed to estimate this burden. Using local, regional, or global data and estimates of population and at-risk groups, deterministic modelling was employed to estimate national incidence or prevalence. Our study revealed that about 4% of Ghanaians suffer from serious fungal infections yearly, with over 35,000 affected by life-threatening invasive fungal infections. -

Tinea Infections: Athlete's Foot, Jock Itch and Ringworm
Tinea Infections: Athlete’s Fo ot, Jock Itch and Ringworm What is tinea? Tinea is caused by a fungus that grows on your skin, hair or nails. As it grows, it spreads out in a circle, leaving normal-looking skin in the middle. This makes it look like a ring. At the edge of the ring, the skin is lifted up by the irritation and looks like a red and scaly rash. To some people, the infection looks like a worm is under the skin. Because of the way it looks, tinea infection is often called “ringworm.” However, there really is not a worm under the skin. How did I get a ringworm/tinea? You can get a fungal infection by contact with person or environment. Some fungi live on damp surfaces, like the floors of showers or locker rooms. You can even catch a fungal infection from your pets. Dogs and cats, as well as farm animals, can be infected with a fungus. Often this infection looks like a patch of skin where fur is missing (mange). What areas of the body are affected by tinea infections? Fungal infections are named for the part of the body they infect. Tinea corporis is a fungal infection of the skin on the body. If you have this infection, you may see small, red spots that grow into large rings almost anywhere on your arms, legs or chest. Tinea pedis is usually called “athlete’s foot.” The moist skin between your toes is a perfect place for a fungus to grow. The skin may become itchy and red, with a white, wet surface. -

Introduction
Notes Introduction 1. In the book, we use the terms ‘fungal infections’ and ‘mycoses’ (or singular fungal infection and mycosis) interchangeably, mostly following the usage of our historical actors in time and place. 2. The term ‘ringworm’ is very old and came from the circular patches of peeled, inflamed skin that characterised the infection. In medicine at least, no one understood it to be associated with worms of any description. 3. Porter, R., ‘The patient’s view: Doing medical history from below’, Theory and Society, 1985, 14: 175–198; Condrau, F., ‘The patient’s view meets the clinical gaze’, Social History of Medicine, 2007, 20: 525–540. 4. Burnham, J. C., ‘American medicine’s golden age: What happened to it?’, Sci- ence, 1982, 215: 1474–1479; Brandt, A. M. and Gardner, M., ‘The golden age of medicine’, in Cooter, R. and Pickstone, J. V., eds, Medicine in the Twentieth Century, Amsterdam, Harwood, 2000, 21–38. 5. The Oxford English Dictionary states that the first use of ‘side-effect’ was in 1939, in H. N. G. Wright and M. L. Montag’s textbook: Materia Med Pharma- col & Therapeutics, 112, when it referred to ‘The effects which are not desired in any particular case are referred to as “side effects” or “side actions” and, in some instances, these may be so powerful as to limit seriously the therapeutic usefulness of the drug.’ 6. Illich, I., Medical Nemesis: The Expropriation of Health, London, Calder & Boyars, 1975. 7. Beck, U., Risk Society: Towards a New Society, New Delhi, Sage, 1992, 56 and 63; Greene, J., Prescribing by Numbers: Drugs and the Definition of Dis- ease, Baltimore, Johns Hopkins University Press, 2007; Timmermann, C., ‘To treat or not to treat: Drug research and the changing nature of essential hypertension’, Schlich, T. -

Fungal Infections from Human and Animal Contact
Journal of Patient-Centered Research and Reviews Volume 4 Issue 2 Article 4 4-25-2017 Fungal Infections From Human and Animal Contact Dennis J. Baumgardner Follow this and additional works at: https://aurora.org/jpcrr Part of the Bacterial Infections and Mycoses Commons, Infectious Disease Commons, and the Skin and Connective Tissue Diseases Commons Recommended Citation Baumgardner DJ. Fungal infections from human and animal contact. J Patient Cent Res Rev. 2017;4:78-89. doi: 10.17294/2330-0698.1418 Published quarterly by Midwest-based health system Advocate Aurora Health and indexed in PubMed Central, the Journal of Patient-Centered Research and Reviews (JPCRR) is an open access, peer-reviewed medical journal focused on disseminating scholarly works devoted to improving patient-centered care practices, health outcomes, and the patient experience. REVIEW Fungal Infections From Human and Animal Contact Dennis J. Baumgardner, MD Aurora University of Wisconsin Medical Group, Aurora Health Care, Milwaukee, WI; Department of Family Medicine and Community Health, University of Wisconsin School of Medicine and Public Health, Madison, WI; Center for Urban Population Health, Milwaukee, WI Abstract Fungal infections in humans resulting from human or animal contact are relatively uncommon, but they include a significant proportion of dermatophyte infections. Some of the most commonly encountered diseases of the integument are dermatomycoses. Human or animal contact may be the source of all types of tinea infections, occasional candidal infections, and some other types of superficial or deep fungal infections. This narrative review focuses on the epidemiology, clinical features, diagnosis and treatment of anthropophilic dermatophyte infections primarily found in North America. -

Seborrheic Dermatitis: an Overview ROBERT A
Seborrheic Dermatitis: An Overview ROBERT A. SCHWARTZ, M.D., M.P.H., CHRISTOPHER A. JANUSZ, M.D., and CAMILA K. JANNIGER, M.D. University of Medicine and Dentistry at New Jersey-New Jersey Medical School, Newark, New Jersey Seborrheic dermatitis affects the scalp, central face, and anterior chest. In adolescents and adults, it often presents as scalp scaling (dandruff). Seborrheic dermatitis also may cause mild to marked erythema of the nasolabial fold, often with scaling. Stress can cause flare-ups. The scales are greasy, not dry, as commonly thought. An uncommon generalized form in infants may be linked to immunodeficiencies. Topical therapy primarily consists of antifungal agents and low-potency steroids. New topical calcineurin inhibitors (immunomodulators) sometimes are administered. (Am Fam Physician 2006;74:125-30. Copyright © 2006 American Academy of Family Physicians.) eborrheic dermatitis can affect patients levels, fungal infections, nutritional deficits, from infancy to old age.1-3 The con- neurogenic factors) are associated with the dition most commonly occurs in condition. The possible hormonal link may infants within the first three months explain why the condition appears in infancy, S of life and in adults at 30 to 60 years of age. In disappears spontaneously, then reappears adolescents and adults, it usually presents as more prominently after puberty. A more scalp scaling (dandruff) or as mild to marked causal link seems to exist between seborrheic erythema of the nasolabial fold during times dermatitis and the proliferation of Malassezia of stress or sleep deprivation. The latter type species (e.g., Malassezia furfur, Malassezia tends to affect men more often than women ovalis) found in normal dimorphic human and often is precipitated by emotional stress. -
Hyperhidrosis: Sweating out the Details
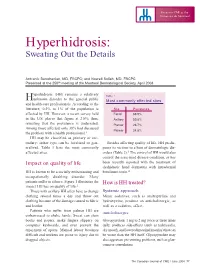
Focus on CME at the Université de Montréal Hyperhidrosis: Sweating Out the Details Antranik Benohanian, MD, FRCPC; and Nowell Solish, MD, FRCPC Presented at the 250th meeting of the Montreal Dermatological Society, April 2003 yperhidrosis (HH) remains a relatively Table 1 Hunknown disorder to the general public Most commonly affected sites and health-care professionals. According to the literature, 0.5% to 1% of the population is Site Prevalence affected by HH. However, a recent survey held Facial 68.9% in the U.S. places that figure at 2.8%; thus, Axillary 50.8% revealing that the prevalence is underrated. Plantar 28.7% Among those affected, only 38% had discussed Palmar 24.8% the problem with a health professional.1 HH may be classified as primary or sec- ondary; either type can be localized or gen- Besides affecting quality of life, HH predis- eralized. Table 1 lists the most commonly poses its victims to a host of dermatologic dis- affected sites. orders (Table 2).3 The control of HH would also control the associated disease condition, as has Impact on quality of life been recently reported with the treatment of dyshidrotic hand dermatitis with intradermal HH is known to be a socially embarrassing and botulinum toxin.4 occupationally disabling disorder. Many patients suffer in silence. Figure 1 illustrates the How is HH treated? impact HH has on quality of life.2 Those with axillary HH often have to change Systemic approach clothing several times a day and throw out Minor sedatives, such as amitriptyline and clothing because of the damage caused to fabric hydroxyzine, produce an anticholinergic, as and leather. -

Estimated Burden of Fungal Infections in Oman
Journal of Fungi Article Estimated Burden of Fungal Infections in Oman Abdullah M. S. Al-Hatmi 1,2,3,* , Mohammed A. Al-Shuhoumi 4 and David W. Denning 5 1 Department of microbiology, Natural & Medical Sciences Research Center, University of Nizwa, Nizwa 616, Oman 2 Department of microbiology, Centre of Expertise in Mycology Radboudumc/CWZ, 6500 Nijmegen, The Netherlands 3 Foundation of Atlas of Clinical Fungi, 1214GP Hilversum, The Netherlands 4 Ibri Hospital, Ministry of Health, Ibri 115, Oman; [email protected] 5 Manchester Fungal Infection Group, Manchester Academic Health Science Centre, The University of Manchester, Manchester M13 9PL, UK; [email protected] * Correspondence: [email protected]; Tel.: +968-25446328; Fax: +968-25446612 Abstract: For many years, fungi have emerged as significant and frequent opportunistic pathogens and nosocomial infections in many different populations at risk. Fungal infections include disease that varies from superficial to disseminated infections which are often fatal. No fungal disease is reportable in Oman. Many cases are admitted with underlying pathology, and fungal infection is often not documented. The burden of fungal infections in Oman is still unknown. Using disease frequencies from heterogeneous and robust data sources, we provide an estimation of the incidence and prevalence of Oman’s fungal diseases. An estimated 79,520 people in Oman are affected by a serious fungal infection each year, 1.7% of the population, not including fungal skin infections, chronic fungal rhinosinusitis or otitis externa. These figures are dominated by vaginal candidiasis, followed by allergic respiratory disease (fungal asthma). An estimated 244 patients develop invasive aspergillosis and at least 230 candidemia annually (5.4 and 5.0 per 100,000). -

Scalp Eczema Factsheet the Scalp Is an Area of the Body That Can Be Affected by Several Types of Eczema
12 Scalp eczema factsheet The scalp is an area of the body that can be affected by several types of eczema. The scalp may be dry, itchy and scaly in a chronic phase and inflamed (red), weepy and painful in an acute (eczema flare) phase. Aside from eczema, there are a number of reasons why the scalp can become dry and itchy (e.g. psoriasis, fungal infection, ringworm, head lice etc.), so it is wise to get a firm diagnosis if there is uncertainty. Types of eczema • Hair clips and headgear – especially those containing that affect the scalp rubber or nickel. Seborrhoeic eczema (dermatitis) is one of the most See the NES booklet on Contact Dermatitis for more common types of eczema seen on the scalp and hairline. details. It can affect babies (cradle cap), children and adults. The Irritant contact dermatitis is a type of eczema that skin appears red and scaly and there is often dandruff as occurs when the skin’s surface is irritated by a substance well, which can vary in severity. There may also be a rash that causes the skin to become dry, red and itchy. on other parts of the face, such as around the eyebrows, For example, shampoos, mousses, hair gels, hair spray, eyelids and sides of the nose. Seborrhoeic eczema can perm solution and fragrance can all cause irritant contact become infected. See the NES factsheets on Adult dermatitis. See the NES booklet on Contact Dermatitis for Seborrhoeic Dermatitis and Infantile Seborrhoeic more details. Dermatitis and Cradle Cap for more details. -

Molecular Analysis of Dermatophytes Suggests Spread of Infection Among Household Members
Molecular Analysis of Dermatophytes Suggests Spread of Infection Among Household Members Mahmoud A. Ghannoum, PhD; Pranab K. Mukherjee, PhD; Erin M. Warshaw, MD; Scott Evans, PhD; Neil J. Korman, MD, PhD; Amir Tavakkol, PhD, DipBact Practice Points When a patient presents with tinea pedis or onychomycosis, inquire if other household members also have the infection, investigate if they have a history of concomitant tinea pedis and onychomycosis, and examine for plantar scaling and/or nail discoloration. If the variables above areCUTIS observed, think about spread of infection and treatment options. Dermatophyte infection from the same strains may Drs. Ghannoum, Mukherjee, and Korman are from University be an important route for transmission of derma- Hospitals Case Medical Center, Cleveland, Ohio. Dr. Warshaw is from the University of Minnesota, Minneapolis, and Minneapolis Veterans tophytoses within a household. In this study, we AffairsDo Medical Center. Dr. Evans is from Notthe Harvard School of Public used molecularCopy methods to identify dermatophytes Health, Boston, Massachusetts. Dr. Tavakkol was from Novartis in members of dermatophyte-infected households Pharmaceuticals Corporation, East Hanover, New Jersey, and and evaluated variables associated with the currently is from Topica Pharmaceuticals, Inc, Los Altos, California. spread of infection. Fungal species were identi- This article was supported by a grant from Novartis Pharmaceuticals Corporation. Dr. Ghannoum has served as a consultant and/or fied by polymerase chain reaction (PCR) using speaker for and has received grants and contracts from Merck & Co, primers targeting the internal transcribed spacer Inc; Novartis Pharmaceuticals Corporation; Pfizer Inc; and Stiefel, (ITS) regions (ITS1 and ITS4). For strain differen- a GSK company. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Dermatophyte and Non-Dermatophyte Onychomycosis in Singapore
Australas J. Dermatol 1992; 33: 159-163 DERMATOPHYTE AND NON-DERMATOPHYTE ONYCHOMYCOSIS IN SINGAPORE JOYCE TENG-EE LIM, HOCK CHENG CHUA AND CHEE LEOK GOH Singapore SUMMARY Onychomycosis is caused by dermatophytes, moulds and yeasts. It is important to identify the non-dermatophyte moulds as they are resistant to the usual anti-fungals. A prospective study was undertaken in the National Skin Centre, Singapore to study the pattern of dermatophyte and non-dermatophyte onychomycosis. 53 male and 47 female patients seen between June 1990 and June 1991 were entered into the study. Direct microscopy was done and the nail clippings were cultured. Toe and finger nails were equally infected. Dermatophytes were isolated from 21 patients namely, T. rubrum (12/21), T. interdigitale (5/21), T. mentagrophytes (3/21) and T. violaceum (1/21). Candida onychomycosis occurred in 39 patients and was caused by C. albicans (38/39) and C. parapsilosis (1/39). 37/39 patients had associated paronychia. 5 types of moulds were isolated from 12 patients, namely Fusarium species (6/12), Aspergillus species (3/12), S. brevicaulis (1/12), Aureobasilium species (1/12) and Penicillium species (1/12). Although the clinical pattern and microscopy may predict the type of organisms, in practice this is difficult. Only cultures were confirmatory. 28% (28/100) had negative cultures despite a positive microscopy, and moulds (12/100) grown might be contaminants rather than pathogens. Key words: Moulds, yeasts, fungi, tinea, onychomycosis, dermatophyte, non-dermatophyte INTRODUCTION METHODS AND MATERIALS Onychomycosis, a common nail disorder, is 100 consecutive patients, seen in our centre caused by dermatophytes, non-dermatophyte between June 1990 and June 1991, with a new moulds, or yeasts. -

Introduction to Bacteriology and Bacterial Structure/Function
INTRODUCTION TO BACTERIOLOGY AND BACTERIAL STRUCTURE/FUNCTION LEARNING OBJECTIVES To describe historical landmarks of medical microbiology To describe Koch’s Postulates To describe the characteristic structures and chemical nature of cellular constituents that distinguish eukaryotic and prokaryotic cells To describe chemical, structural, and functional components of the bacterial cytoplasmic and outer membranes, cell wall and surface appendages To name the general structures, and polymers that make up bacterial cell walls To explain the differences between gram negative and gram positive cells To describe the chemical composition, function and serological classification as H antigen of bacterial flagella and how they differ from flagella of eucaryotic cells To describe the chemical composition and function of pili To explain the unique chemical composition of bacterial spores To list medically relevant bacteria that form spores To explain the function of spores in terms of chemical and heat resistance To describe characteristics of different types of membrane transport To describe the exact cellular location and serological classification as O antigen of Lipopolysaccharide (LPS) To explain how the structure of LPS confers antigenic specificity and toxicity To describe the exact cellular location of Lipid A To explain the term endotoxin in terms of its chemical composition and location in bacterial cells INTRODUCTION TO BACTERIOLOGY 1. Two main threads in the history of bacteriology: 1) the natural history of bacteria and 2) the contagious nature of infectious diseases, were united in the latter half of the 19th century. During that period many of the bacteria that cause human disease were identified and characterized. 2. Individual bacteria were first observed microscopically by Antony van Leeuwenhoek at the end of the 17th century.