Lichen Simplex Chronicus: Easy Psychological Interventions That Every Dermatologist Should Know
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Diagnostic Approach to Pruritus
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by DigitalCommons@University of Nebraska University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln U.S. Air Force Research U.S. Department of Defense 2011 A Diagnostic Approach to Pruritus Brian V. Reamy Christopher W. Bunt Stacy Fletcher Follow this and additional works at: https://digitalcommons.unl.edu/usafresearch This Article is brought to you for free and open access by the U.S. Department of Defense at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in U.S. Air Force Research by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. A Diagnostic Approach to Pruritus BRIAN V. REAMY, MD, Uniformed Services University of the Health Sciences, Bethesda, Maryland CHRISTOPHER W. BUNT, MAJ, USAF, MC, and STACY FLETCHER, CAPT, USAF, MC Ehrling Bergquist Family Medicine Residency Program, Offutt Air Force Base, Nebraska, and the University of Nebraska Medical Center, Omaha, Nebraska Pruritus can be a symptom of a distinct dermatologic condition or of an occult underlying systemic disease. Of the patients referred to a dermatologist for generalized pruritus with no apparent primary cutaneous cause, 14 to 24 percent have a systemic etiology. In the absence of a primary skin lesion, the review of systems should include evaluation for thyroid disorders, lymphoma, kidney and liver diseases, and diabetes mellitus. Findings suggestive of less seri- ous etiologies include younger age, localized symptoms, acute onset, involvement limited to exposed areas, and a clear association with a sick contact or recent travel. Chronic or general- ized pruritus, older age, and abnormal physical findings should increase concern for underly- ing systemic conditions. -

ORIGINAL ARTICLE a Clinical and Histopathological Study of Lichenoid Eruption of Skin in Two Tertiary Care Hospitals of Dhaka
ORIGINAL ARTICLE A Clinical and Histopathological study of Lichenoid Eruption of Skin in Two Tertiary Care Hospitals of Dhaka. Khaled A1, Banu SG 2, Kamal M 3, Manzoor J 4, Nasir TA 5 Introduction studies from other countries. Skin diseases manifested by lichenoid eruption, With this background, this present study was is common in our country. Patients usually undertaken to know the clinical and attend the skin disease clinic in advanced stage histopathological pattern of lichenoid eruption, of disease because of improper treatment due to age and sex distribution of the diseases and to difficulties in differentiation of myriads of well assess the clinical diagnostic accuracy by established diseases which present as lichenoid histopathology. eruption. When we call a clinical eruption lichenoid, we Materials and Method usually mean it resembles lichen planus1, the A total of 134 cases were included in this study prototype of this group of disease. The term and these cases were collected from lichenoid used clinically to describe a flat Bangabandhu Sheikh Mujib Medical University topped, shiny papular eruption resembling 2 (Jan 2003 to Feb 2005) and Apollo Hospitals lichen planus. Histopathologically these Dhaka (Oct 2006 to May 2008), both of these are diseases show lichenoid tissue reaction. The large tertiary care hospitals in Dhaka. Biopsy lichenoid tissue reaction is characterized by specimen from patients of all age group having epidermal basal cell damage that is intimately lichenoid eruption was included in this study. associated with massive infiltration of T cells in 3 Detailed clinical history including age, sex, upper dermis. distribution of lesions, presence of itching, The spectrum of clinical diseases related to exacerbating factors, drug history, family history lichenoid tissue reaction is wider and usually and any systemic manifestation were noted. -

Red, Weeping and Oozing P.51 6
DERM CASE Test your knowledge with multiple-choice cases This month–9 cases: 1. Red, Weeping and Oozing p.51 6. A Chronic Condition p.56 2. A Rough Forehead p.52 7. “Why am I losing hair?” p.57 3. A Flat Papule p.53 8. Bothersome Bites p.58 4. Itchy Arms p.54 9. Ring-like Rashes p.59 5. A Patchy Neck p.55 on © buti t ri , h ist oad rig D wnl Case 1 y al n do p ci ca use o er sers nal C m d u rso m rise r pe o utho y fo C d. A cop or bite ngle Red, Weleepirnohig a sind Oozing a se p rint r S ed u nd p o oris w a t f uth , vie o Una lay AN12-year-old boy dpriesspents with a generalized, itchy rash over his body. The rash has been present for two years. Initially, the lesions were red, weeping and oozing. In the past year, the lesions became thickened, dry and scaly. What is your diagnosis? a. Psoriasis b. Pityriasis rosea c. Seborrheic dermatitis d. Atopic dermatitis (eczema) Answer Atopic dermatitis (eczema) (answer d) is a chroni - cally relapsing dermatosis characterized by pruritus, later by a widespread, symmetrical eruption in erythema, vesiculation, papulation, oozing, crust - which the long axes of the rash extend along skin ing, scaling and, in chronic cases, lichenification. tension lines and give rise to a “Christmas tree” Associated findings can include xerosis, hyperlin - appearance. Seborrheic dermatitis is characterized earity of the palms, double skin creases under the by a greasy, scaly, non-itchy, erythematous rash, lower eyelids (Dennie-Morgan folds), keratosis which might be patchy and focal and might spread pilaris and pityriasis alba. -

Common Dermatoses in Patients with Obsessive Compulsive Disorders Mircea Tampa Carol Davila University of Medicine and Pharmacy, Tampa [email protected]
Journal of Mind and Medical Sciences Volume 2 | Issue 2 Article 7 2015 Common Dermatoses in Patients with Obsessive Compulsive Disorders Mircea Tampa Carol Davila University of Medicine and Pharmacy, [email protected] Maria Isabela Sarbu Victor Babes Hospital for Infectious and Tropical Diseases, [email protected] Clara Matei Carol Davila University of Medicine and Pharmacy Vasile Benea Victor Babes Hospital for Infectious and Tropical Diseases Simona Roxana Georgescu Carol Davila University of Medicine and Pharmacy Follow this and additional works at: http://scholar.valpo.edu/jmms Part of the Medicine and Health Sciences Commons Recommended Citation Tampa, Mircea; Sarbu, Maria Isabela; Matei, Clara; Benea, Vasile; and Georgescu, Simona Roxana (2015) "Common Dermatoses in Patients with Obsessive Compulsive Disorders," Journal of Mind and Medical Sciences: Vol. 2 : Iss. 2 , Article 7. Available at: http://scholar.valpo.edu/jmms/vol2/iss2/7 This Review Article is brought to you for free and open access by ValpoScholar. It has been accepted for inclusion in Journal of Mind and Medical Sciences by an authorized administrator of ValpoScholar. For more information, please contact a ValpoScholar staff member at [email protected]. JMMS 2015, 2(2): 150- 158. Review Common dermatoses in patients with obsessive compulsive disorders Mircea Tampa1, Maria Isabela Sarbu2, Clara Matei1, Vasile Benea2, Simona Roxana Georgescu1 1 Carol Davila University of Medicine and Pharmacy, Department of Dermatology and Venereology 2 Victor Babes Hospital for Infectious and Tropical Diseases, Department of Dermatology and Venereology Corresponding author: Maria Isabela Sarbu, e-mail: [email protected] Running title: Dermatoses in obsessive compulsive disorders Keywords: Factitious disorders, obsessive-compulsive disorders, acne excoriee www.jmms.ro 2015, Vol. -

Lichen Simplex Chronicus
LICHEN SIMPLEX CHRONICUS http://www.aocd.org Lichen simplex chronicus is a localized form of lichenified (thickened, inflamed) atopic dermatitis or eczema that occurs in well defined plaques. It is the result of ongoing, chronic rubbing and scratching of the skin in localized areas. It is generally seen in patients greater than 20 years of age and is more frequent in women. Emotional stress can play a part in the course of this skin disease. There is mainly one symptom: itching. The rubbing and scratching that occurs in response to the itch can become automatic and even unconscious making it very difficult to treat. It can be magnified by seeming innocuous stimuli such as putting on clothes, or clothes rubbing the skin which makes the skin warmer resulting in increased itch sensation. The lesions themselves are generally very well defined areas of thickened, erythematous, raised area of skin. Frequently they are linear, oval or round in shape. Sites of predilection include the back of the neck, ankles, lower legs, upper thighs, forearms and the genital areas. They can be single lesions or multiple. This can be a very difficult condition to treat much less resolve. It is of utmost importance that the scratching and rubbing of the skin must stop. Treatment is usually initiated with topical corticosteroids for larger areas and intralesional steroids might also be considered for small lesion(s). If the patient simply cannot keep from rubbing the area an occlusive dressing might be considered to keep the skin protected from probing fingers. Since this is not a histamine driven itch phenomena oral antihistamines are generally of little use in these cases. -

Photodermatoses Update Knowledge and Treatment of Photodermatoses Discuss Vitamin D Levels in Photodermatoses
Ashley Feneran, DO Jenifer Lloyd, DO University Hospitals Regional Hospitals AMERICAN OSTEOPATHIC COLLEGE OF DERMATOLOGY Objectives Review key points of several photodermatoses Update knowledge and treatment of photodermatoses Discuss vitamin D levels in photodermatoses Types of photodermatoses Immunologically mediated disorders Defective DNA repair disorders Photoaggravated dermatoses Chemical- and drug-induced photosensitivity Types of photodermatoses Immunologically mediated disorders Polymorphous light eruption Actinic prurigo Hydroa vacciniforme Chronic actinic dermatitis Solar urticaria Polymorphous light eruption (PMLE) Most common form of idiopathic photodermatitis Possibly due to delayed-type hypersensitivity reaction to an endogenous cutaneous photo- induced antigen Presents within minutes to hours of UV exposure and lasts several days Pathology Superficial and deep lymphocytic infiltrate Marked papillary dermal edema PMLE Treatment Topical or oral corticosteroids High SPF Restriction of UV exposure Hardening – natural, NBUVB, PUVA Antimalarial PMLE updates Study suggests topical vitamin D analogue used prophylactically may provide therapeutic benefit in PMLE Gruber-Wackernagel A, Bambach FJ, Legat A, et al. Br J Dermatol, 2011. PMLE updates Study seeks to further elucidate the pathogenesis of PMLE Found a decrease in Langerhans cells and an increase in mast cell density in lesional skin Wolf P, Gruber-Wackernagel A, Bambach I, et al. Exp Dermatol, 2014. Actinic prurigo Similar to PMLE Common in native -

Triamcinolone Acetonide Injectable Suspension, USP)
KENALOG®-10 INJECTION (triamcinolone acetonide injectable suspension, USP) NOT FOR USE IN NEONATES CONTAINS BENZYL ALCOHOL For Intra-articular or Intralesional Use Only NOT FOR INTRAVENOUS, INTRAMUSCULAR, INTRAOCULAR, EPIDURAL, OR INTRATHECAL USE DESCRIPTION Kenalog®-10 Injection (triamcinolone acetonide injectable suspension, USP) is triamcinolone acetonide, a synthetic glucocorticoid corticosteroid with marked anti-inflammatory action, in a sterile aqueous suspension suitable for intralesional and intra-articular injection. THIS FORMULATION IS SUITABLE FOR INTRA-ARTICULAR AND INTRALESIONAL USE ONLY. Each mL of the sterile aqueous suspension provides 10 mg triamcinolone acetonide, with 0.66% sodium chloride for isotonicity, 0.99% (w/v) benzyl alcohol as a preservative, 0.63% carboxymethylcellulose sodium, and 0.04% polysorbate 80. Sodium hydroxide or hydrochloric acid may have been added to adjust pH between 5.0 and 7.5. At the time of manufacture, the air in the container is replaced by nitrogen. The chemical name for triamcinolone acetonide is 9-Fluoro-11β,16α,17,21-tetrahydroxypregna- 1,4-diene-3,20-dione cyclic 16,17-acetal with acetone. Its structural formula is: 1 Reference ID: 4241593 MW 434.50 CLINICAL PHARMACOLOGY Glucocorticoids, naturally occurring and synthetic, are adrenocortical steroids that are readily absorbed from the gastrointestinal tract. Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt- retaining properties, are used as replacement therapy in adrenocortical deficiency states. -
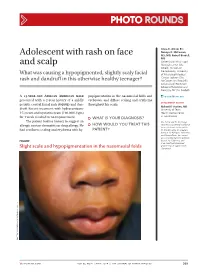
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Guías Diagnósticas Y Terapeúticas De Las 10 Patologías Más Frecuentes
HOSPITAL INFANTIL DE MÉXICO “FEDERICO GÓMEZ” SERVICIO DE DERMATOLOGÍA GUÍAS DIAGNÓSTICAS Y TERAPÉUTICAS DE LAS 10 PATOLOGÍAS MÁS FRECUENTES DR CARLOS ALFREDO MENA CEDILLOS, JEFE DEL SERVICIO DRA ADRIANA MARÍA VALENCIA HERRERA DERMATITIS ATOPICA SINONIMIA. Neurodermatitis, prurigo de Besnier, eccema del lactante. DEFINICION. Enfermedad reaccional, crónica y recidivante de la piel, con un patrón clínico e historia natural característicos. No se conoce la causa específica, pero se ha relacionado con susceptibilidad genética, disturbios inmuológicos y constitucionales, sobre los que actúan factores desencadenantes. EPIDEMIOLOGIA: Es la dermatosis más frecuente en población pediátrica. La prevalencia ha mostrando incremento en las últimas décadas, siendo del 18-20%. Es mas frecuente en áreas urbanas de países industrializados, especialmente en inmigrantes provenientes de países con menor prevalencia. No existe clara predilección racial ni diferencia en cuanto al sexo. Puede presentarse a cualquier edad, con claro predominio en la población pediátrica, 60-85% de los casos inicia en el primer año de vida y 85-95% antes de los 5 años; 10-25% de los casos persiste con recaídas en la edad adulta. ETIOPATOGENIA. La etiología es desconocida pero parece ser resultado de una compleja interacción aspectos genéticos, inmunológicos y defectos en la barrera epidérmica, existiendo múltiples factores descencadenantes, queactúan sobre un terreno constitucionalmente alterado. 1. Anomalías genéticas. Tiene clara naturaleza familiar, pero no se ha precisado el mecanismo de herencia, existiendo en 70% de los pacientes antecedentes de atopia. Los antígenos de histocompatibilidad HL-A9, HL-A3, HL-B12 y HL-Bw40 se han descrito en estos pacientes. 2. Disturbios inmunológicos. Existen cambios significativos en la inmunidad humoral y celular. -

Chronic Pruritic Vulva Lesion
Photo RoUNDS Stephen Colden Cahill, DO Chronic pruritic vulva lesion College of Osteopathic Medicine, Michigan State University, East Lansing; The patient was not sexually active and denied any and Lakeshore Health vaginal discharge. So what was causing the intense Partners, Holland, Mich itching on her labia? [email protected] Department eDItOr richard p. Usatine, mD University of Texas Health Science Center at San Antonio During a routine exam, a 45-year-old Cau- both of her labia majora (FIGURE). Throughout casian woman complained of intense itching the lesion, there were scattered areas of exco- The author reported no potential conflict of interest on her labia. She said that the itching had been riation. Her labia minor were spared. relevant to this article. an issue for more than 9 months and that she A speculum and bimanual exam were found herself scratching several times a day. normal. No inguinal lymphadenopathy was She denied any vaginal discharge and said she present. hadn’t been sexually active in years. She had tried over-the-counter antifungals and topical ● WhaT is your diagnosis? Benadryl, but they provided only limited relief. The patient had red thickened plaques ● HoW Would you TREAT THIS with accentuated skin lines (furrows) covering PATIENT? Figure Red thickened plaques on labia majora p ho T o cour T esy of: St ephen c olden c ahill, DO jfponline.com Vol 62, no 2 | february 2013 | The journal of family pracTice 97 PHOTO RoUNDS Diagnosis: taneous lesion of unknown etiology. It can Lichen simplex chronicus be found throughout the body, including the This patient was given a diagnosis of lichen mucous membranes. -

Skin Manifestations of Systemic Disease
THEME WEIRD SKIN STUFF Adriene Lee BSc(Med), MBBS(Hons), FACD, is visiting dermatologist, St Vincent's Hospital and Monash Medical Centre, and Lecturer, Department of General Practice, Monash University, Victoria. [email protected] Skin manifestations of systemic disease Dermatologic complaints are a common reason for Background presentation to a general practitioner. In such cases, one needs Dermatologic complaints are a common reason for presentation to determine if the complaint may be a manifestation of a more to a general practitioner. In some cases, one needs to determine serious underlying systemic disease. Disorders of the every if the complaint may be a manifestation of a more serious underlying systemic disease. organ system may cause skin symptoms and signs, some of which are due to treatment of these conditions. It is beyond the Objective scope of this review to cover all potential skin manifestations of This article aims to highlight common dermatologic systemic disease. This article highlights the more common, presentations where further assessment is needed to exclude classic and important manifestations in three different groups: an underlying systemic disease, to discuss classic cutaneous features of specific systemic diseases, and to outline rare • ‘When to look further’ – where dermatologic presentations cutaneous paraneoplastic syndromes. require further assessment to exclude underlying systemic disease, and guide appropriate management Discussion • ‘What to look for’ – where certain systemic diseases have Skin manifestations of systemic disease are wide, varied, classic cutaneous findings specific and nonspecific. Generalised pruritus and cutaneous • ‘What not to miss’ – where specific cutaneous signs might be vasculitis are more common cutaneous presentations where an underlying systemic disease may be present and will the initial presentation of an underlying malignancy. -

Atopic Dermatitis (Eczema) •Chronic Inflammatory Skin Disease That Begins During Infancy Or Early Childhood
9/18/2019 Pediatric Dermatology Jennifer Abrahams, MD, FAAD, DTM&H Collaborators: Kate Oberlin, MD; Nayoung Lee MD September 27th, 2019 1 Disclosures • Nothing to disclose 2 1 9/18/2019 Disclaimer *Pediatric dermatology is taught over 3 years of derm-specific residency training and there is an additional year of subspecialized fellowship! *We won’t cover all of pediatric derm in an hour but I hope to give you some common highlights 3 A 9 month old infant presents with the following skin lesions. Which of the following is most likely true of this disease? A.) Asthma generally precedes skin findings B.) The majority of affected children will outgrow the skin disease C.) There is no way to avoid or decrease risk of progression of the disease D.) Genetic factors account for approx 1% of susceptibility to early onset of this disease 4 2 9/18/2019 A 9 month old infant presents with the following skin lesions. Which of the following is most likely true of this disease? A.) Asthma generally precedes skin findings B.) The majority of affected children will outgrow the skin disease C.) There is no way to avoid or decrease risk of progression of the disease D.) Genetic factors account for approx 1% of susceptibility to early onset of this disease 5 6 3 9/18/2019 Atopic Dermatitis (Eczema) •Chronic inflammatory skin disease that begins during infancy or early childhood •Often associated with other “atopic” disorders • Asthma • Allergic rhinitis (seasonal allergies) • Food allergies •Characterized by intense itch and a chronic relapsing course •Prevalence almost 30% in developed countries 7 Table courtesy of Bolognia, et al.