Understanding Blindness in Cats
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

INDEX Abducent Neurons Anatomy 135 Clinical Signs 137 Diseases
INDEX Abducent neurons Anatomy 135 Clinical signs 137 Diseases 139 Function 135 Abiotrophic sensorineural deafness 438 Abiotrophy 100, 363 Auditory 438 Cerebellar cortical 363 Motor neuron 100 Nucleus ambiguus 159 Peripheral vestibular 336 Abscess-Brainstem 330 Caudal cranial fossa 343 Cerebellar 344 Cerebral 416, 418 Pituitary 162 Streptococcus equi 418 Abyssian cat-Glucocerebrosidosis 427 Myastheina gravis 93 Accessory neurons Anatomy 152 Clinical signs 153 Diseases 153 Acetozolamide 212 Acetylcholine 78, 169, 354, 468, 469 Receptor 78 Acetylcholinesterase 79 Achiasmatic Belgian sheepdog 345 Acoustic stria 434 Acral mutilation 237 Adenohypophysis 483 Releasing factors 483 Adenosylmethionine 262 Adhesion-Interthalamic 33, 476 Adiposogenital syndrome 484 Adipsia 458, 484 Adrenocorticotrophic hormone 485 Adversive syndrome 72, 205, 460 Afghan hound-Inherited myelinolytic encephalomyelopathy 264 Agenized flour 452 Aino virus 44 Akabane virus 43 Akita-Congenital peripiheral vestibular disease 336 Alaskan husky encephalopathy 522 Albinism, ocular 345 Albinotic sensorineural deafness 438 Alexander disease 335 Allodynia 190 Alpha fucosidosis 427 Alpha glucosidosis 427 Alpha iduronidase 427 Alpha mannosidase 427 Alpha melanotropism 484 Alsatian-idiopathic epilepsy 458 Alternative anticonvulsant drugs 466 American Bulldog-Ceroid lipofuscinosis 385, 428 American Miniature Horse-Narcolepsy 470 American StaffordshireTerrier-Cerebellar cortical abiotrophy 367 Amikacin 329 Aminocaproic acid 262 Aminoglycoside antibiotics 329, 439 Amprolium toxicity -

Abyssinian Cat Club Type: Breed
Abyssinian Cat Association Abyssinian Cat Club Asian Cat Association Type: Breed - Abyssinian Type: Breed – Abyssinian Type: Breed – Asian LH, Asian SH www.abycatassociation.co.uk www.abyssiniancatclub.com http://acacats.co.uk/ Asian Group Cat Society Australian Mist Cat Association Australian Mist Cat Society Type: Breed – Asian LH, Type: Breed – Australian Mist Type: Breed – Australian Mist Asian SH www.australianmistcatassociation.co.uk www.australianmistcats.co.uk www.asiangroupcatsociety.co.uk Aztec & Ocicat Society Balinese & Siamese Cat Club Balinese Cat Society Type: Breed – Aztec, Ocicat Type: Breed – Balinese, Siamese Type: Breed – Balinese www.ocicat-classics.club www.balinesecatsociety.co.uk Bedford & District Cat Club Bengal Cat Association Bengal Cat Club Type: Area Type: PROVISIONAL Breed – Type: Breed – Bengal Bengal www.thebengalcatclub.com www.bedfordanddistrictcatclub.com www.bengalcatassociation.co.uk Birman Cat Club Black & White Cat Club Blue Persian Cat Society Type: Breed – Birman Type: Breed – British SH, Manx, Persian Type: Breed – Persian www.birmancatclub.co.uk www.theblackandwhitecatclub.org www.bluepersiancatsociety.co.uk Blue Pointed Siamese Cat Club Bombay & Asian Cats Breed Club Bristol & District Cat Club Type: Breed – Siamese Type: Breed – Asian LH, Type: Area www.bpscc.org.uk Asian SH www.bristol-catclub.co.uk www.bombayandasiancatsbreedclub.org British Shorthair Cat Club Bucks, Oxon & Berks Cat Burmese Cat Association Type: Breed – British SH, Society Type: Breed – Burmese Manx Type: Area www.burmesecatassociation.org -

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

Publications for Julia Beatty 2021 2020 2019
Publications for Julia Beatty 2021 <a href="http://dx.doi.org/10.1089/vbz.2019.2520">[More Mazeau, L., Wylie, C., Boland, L., Beatty, J. (2021). A shift Information]</a> towards early‑age desexing of cats under veterinary care in Australia. Scientific Reports, 11(1), 1-9. <a 2019 href="http://dx.doi.org/10.1038/s41598-020-79513-6">[More Pesavento, P., Jackson, K., Scase, T., Tse, T., Hampson, B., Information]</a> Munday, J., Barrs, V., Beatty, J. (2019). A Novel Hepadnavirus Kay, A., Boland, L., Kidd, S., Beatty, J., Talbot, J., Barrs, V. is Associated with Chronic Hepatitis and Hepatocellular (2021). Complete clinical response to combined antifungal Carcinoma in Cats. Viruses, 11(10), 1-8. <a therapy in two cats with invasive fungal rhinosinusitis caused href="http://dx.doi.org/10.3390/v11100969">[More by cryptic Aspergillus species in section Fumigati. Medical Information]</a> Mycology Case Reports, 34, 13-17. <a Whitney, J., Haase, B., Beatty, J., Barrs, V. (2019). Breed- href="http://dx.doi.org/10.1016/j.mmcr.2021.08.005">[More specific variations in the coding region of toll-like receptor 4 in Information]</a> the domestic cat. Veterinary Immunology and Sacrist�n, I., Acu�a, F., Aguilar, E., Garc�a, S., Jos� Immunopathology, 209, 61-69. <a L�pez, M., Cabello, J., Hidalgo-Hermoso, E., Sanderson, J., href="http://dx.doi.org/10.1016/j.vetimm.2019.02.009">[More Terio, K., Barrs, V., Beatty, J., et al (2021). Cross-species Information]</a> transmission of retroviruses among domestic and wild felids in Van Brussel, K., Carrai, M., Lin, C., Kelman, M., Setyo, L., human-occupied landscapes in Chile. -

Canine Red Eye Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO
PEER REVIEWED Clinical Approach to the CANINE RED EYE Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO he acute red eye is a common clinical challenge for tion of the deep episcleral vessels, and is characterized general practitioners. Redness is the hallmark of by straight and immobile episcleral vessels, which run Tocular inflammation; it is a nonspecific sign related 90° to the limbus. Episcleral injection is an external to a number of underlying diseases and degree of redness sign of intraocular disease, such as anterior uveitis and may not reflect the severity of the ocular problem. glaucoma (Figures 3 and 4). Occasionally, episcleral Proper evaluation of the red eye depends on effective injection may occur in diseases of the sclera, such as and efficient diagnosis of the underlying ocular disease in episcleritis or scleritis.1 order to save the eye’s vision and the eye itself.1,2 • Corneal Neovascularization » Superficial: Long, branching corneal vessels; may be SOURCE OF REDNESS seen with superficial ulcerative (Figure 5) or nonul- The conjunctiva has small, fine, tortuous and movable vessels cerative keratitis (Figure 6) that help distinguish conjunctival inflammation from deeper » Focal deep: Straight, nonbranching corneal vessels; inflammation (see Ocular Redness algorithm, page 16). indicates a deep corneal keratitis • Conjunctival hyperemia presents with redness and » 360° deep: Corneal vessels in a 360° pattern around congestion of the conjunctival blood vessels, making the limbus; should arouse concern that glaucoma or them appear more prominent, and is associated with uveitis (Figure 4) is present1,2 extraocular disease, such as conjunctivitis (Figure 1). -
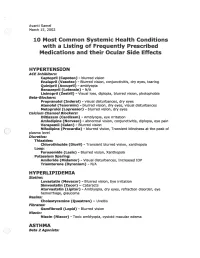
2002 Samel 10 Most Common Systemic Health Conditions with A
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)- -

The Yellow Cat: Diagnostic & Therapeutic Strategies
Peer Reviewed THE YELLOW CAT: DIAGNOSTIC & THERAPEUTIC STRATEGIES The Yellow Cat: Diagnostic & Therapeutic Strategies Craig B. Webb, PhD, DVM, Diplomate ACVIM (Small Animal Internal Medicine) Colorado State University There is no mystery when it comes to a “yellow” cat. Icterus and jaundice—both of which describe a yellowish pigmentation of the skin—indicate hyperbilirubinemia, a 5- to 10-fold elevation in serum bilirubin concentration. However, this is where the certainty ends and the diagnostic challenge begins. The icteric cat presentation is not a sensitive or specific marker of disease, despite the visually obvious and impressive clinical sign (Figure 1).1 The objective of this article is to briefly review differentials for hyperbilirubinemia in the cat, and present a diagnostic and therapeutic strategy that will help practitioners approach this problem in an efficient and effective manner. FIGURE 1. Icteric pinna of a cat in the critical HYPERBILIRUBINEMIA: ORGANIZATION care isolation unit; prehepatic hemolysis BY LOCATION and anemia are a result of Cytauxzoon felis infection. Hyperbilirubinemia The differentials for hyperbilirubinemia should be results when organized by location: prehepatic, hepatic, and serum bilirubin posthepatic. While, in cats, it is common to find Hepatic Disease concentrations concurrent disease processes, starting from this A significant decrease, or loss, of hepatocellular reach 2 to 3 mg/dL foundation is the first step toward an effective and function effects bilirubin metabolism, and (35–50 mcmol/L). efficient diagnostic workup of icteric cats. frequently results in intrahepatic cholestasis (Table 1, page 40). Unconjugated bilirubin from damaged Prehepatic Disease hepatocytes is present, although the majority of Hemolysis releases hemoglobin, which is then bilirubin that appears in the cat’s circulation is metabolized through biliverdin to bilirubin in the conjugated, having completed the metabolic step liver. -
GAZE and AUTONOMIC INNERVATION DISORDERS Eye64 (1)
GAZE AND AUTONOMIC INNERVATION DISORDERS Eye64 (1) Gaze and Autonomic Innervation Disorders Last updated: May 9, 2019 PUPILLARY SYNDROMES ......................................................................................................................... 1 ANISOCORIA .......................................................................................................................................... 1 Benign / Non-neurologic Anisocoria ............................................................................................... 1 Ocular Parasympathetic Syndrome, Preganglionic .......................................................................... 1 Ocular Parasympathetic Syndrome, Postganglionic ........................................................................ 2 Horner Syndrome ............................................................................................................................. 2 Etiology of Horner syndrome ................................................................................................ 2 Localizing Tests .................................................................................................................... 2 Diagnosis ............................................................................................................................... 3 Flow diagram for workup of anisocoria ........................................................................................... 3 LIGHT-NEAR DISSOCIATION ................................................................................................................. -

Intermittent Mydriasis Associated with Carotid Vascular Occlusion
Eye (2018) 32, 457–459 © 2018 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0950-222X/18 www.nature.com/eye 1,2 2 2 Intermittent mydriasis PD Chamberlain , A Sadaka , S Berry CASE SERIES 1,2,3,4,5,6 associated with carotid and AG Lee vascular occlusion Abstract the literature as benign episodic pupillary dilation or BEUM. We report two patients with Purpose To describe two cases of 1 stereotyped, intermittent, neurologically acquired occlusive disease of the ipsilateral ICA Department of Ophthalmology, Blanton isolated, unilateral mydriasis in patients who developed multiple, stereotyped, neurologically isolated, transient episodes of Eye Institute, Houston with a history of acquired internal carotid Methodist Hospital, artery (ICA) occlusive disease on the mydriasis consistent with BEUM. We discuss the Houston, TX, USA ipsilateral side. possible mechanisms, differential diagnosis and 2 Patients Two patients with intermittent recommended evaluation for atypical cases for Department of episodic mydriasis. Ophthalmology, Baylor mydriasis. College of Medicine, Methods Case Series. Houston, TX, USA Results Case one: A 78-year-old man Case one 3 experienced 10 episodes of intermittent, Departments of Ophthalmology, Neurology, unilateral, and painless mydriasis in the left A 78-year-old man presented with 10 episodes of and Neurosurgery, Weill stereotyped, intermittent, unilateral, painless eye and had 100% occlusion of the left ICA Cornell Medical College, artery due to atherosclerotic disease. Case two: pupillary dilation of the left eye (OS) lasting New York, NY, USA A 26-year-old woman with history of migraine minutes to hours at a time without diplopia or fi 4Department of developed new painless, intermittent episodes ptosis. -

Document43 Breed Article Somali, Website Cfa.Org
Breed Article: Somali The Somali Cat: 30 Years and Going Strong! by Kathy Black What comes to mind when we think of the Somali? A longhaired Abyssinian? A cat that resembles a fox? A colorful cat with squirrel markings? Many colorful adjectives could be used to describe the Somali, but I think that the Somali breeders/owners themselves express it the best. Recently at the CFA International Cat Show in Kansas City, I asked some of them to describe the Somali, using the first thought that came to mind. Here are their responses: very loving, lively, playful, large bushy tail, into everything, softest fur ever felt, the king, busy, ready for action, foxy, ornery, strikingly beautiful, lifetime companion, active, mischievous, and colorful. The Somali is a combination of beauty and personality. The first thing that captures your attention is the beauty and uniqueness of the Somali. They are very striking cats, with their colorful coats, Photo: © Carl Widmer bushy tails, facial markings and alert personalities. They come in four recognized colors: ruddy, red, blue and fawn. The combination of ticked, dramatic colored fur, facial markings, large ears, full ruff, dark hocks and bushy tail and britches is what gives the Somali its wild feral look - and is what immediately draws fascinated attention to the breed. As you can see described above, however, the Somali's personality is what their breeders and owners prize the most. Somalis are intelligent cats, very playful and active. They are "people cats" in the truest sense, in that they seek out the attention of their owners. -

Miotic Adie's Pupils
Journal of Cll/lical Neuro-ophtllJllmology 9(1): 43-45, 1989. RilVen Press, Ltd., New York Miotic Adie's Pupils Michael L. Rosenberg, M.D. Two young adults, aged 24 and 31, had a long history of Adie's syndrome or, pupillotonia, is typically small, poorly reactive pupilS. There was no history of characterized by either unilaterally or bilaterally large pupils, and a review of old photographs confirmed enlarged pupils that are unresponsive to light (1). 10 and 5 years, respectively, of miosis. Both were found to have bilateral tonic pupils that were supersensitive to The diagnosis is made clinically by watching for a diluted pilocarpine. Although it is possible that they had tonic constriction to near stimulation followed by a an unusually early onset of bilateral Adie's syndrome tonic redilatation. with dilated pupils that was not noticed, it is suggested Two young adults are described who were noted that some patients might have primary miotic Adie's during routine examinations to have bilaterally mi pupils without ever passing through a mydriatic phase. Key Words: Adie's syndrome-Argyll Robertson pu otic pupils that were thought to be fixed to light. pils-Miosis. They were both referred for the evaluation of Ar gyll Robertson pupils. Evaluation revealed bilat eral tonic reactions to near stimulation in both pa tients, typical of Adie's tonic pupilS. The diagnosis of parasympathetic denervation was confirmed in both patients as their pupils constricted with di luted pilocarpine. The cases reinforce the principle that any pupil regardless of size should be evalu ated for the possibility of pupillotonia. -

Changes in Intraocular Pressure After Pharmacologic Pupil Dilation
UCLA UCLA Previously Published Works Title Changes in intraocular pressure after pharmacologic pupil dilation Permalink https://escholarship.org/uc/item/7nz7c380 Journal BMC Ophthalmology, 12(1) ISSN 1471-2415 Authors Kim, Joon Park, Ki Han, So et al. Publication Date 2012-09-27 DOI http://dx.doi.org/10.1186/1471-2415-12-53 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Kim et al. BMC Ophthalmology 2012, 12:53 http://www.biomedcentral.com/1471-2415/12/53 RESEARCH ARTICLE Open Access Changes in intraocular pressure after pharmacologic pupil dilation Joon Mo Kim1, Ki Ho Park2*, So Young Han1, Kwan Soo Kim1, Dong Myung Kim2, Tae Woo Kim3 and Joseph Caprioli4 Abstract Background: Intraocular pressure (IOP) may vary according to the change of ocular conditions. In this study, we want to assess the effect and mechanism of pupil dilation on IOP in normal subjects. Methods: We prospectively evaluated 32 eyes of 32 patients (age; 61.7 ± 8.2 years) with normal open angles under diurnal IOP. IOP was measured every two hours from 9 AM to 11 PM for one day to establish baseline values and was measured again for one day to assess the differences after dilation. To induce dilation, we administered 2.5% phenylephrine and 1% tropicamide every 5 minutes from 8:30 AM to 8:45 AM and for every two hours from 11 AM to 9 PM to keep the pupil dilated. Diurnal IOP, biometry, Visante OCT, and laser flare photometry were measured before and after dilation. Results: We observed a significant increase in IOP after dilation, 1.85 ± 2.01 mmHg (p = 0.002).