Best Airway and Ventilation Strategy During CPR and After Resuscitation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -

Airway – Oropharyngeal: Insertion; Maintenance; Suction; Removal
Policies & Procedures Title: AIRWAY – OROPHARYNGEAL: INSERTION; MAINTENANCE; SUCTION; REMOVAL I.D. Number: 1159 Authorization Source: Nursing Date Revised: September 2014 [X] SHR Nursing Practice Committee Date Effective: October 2002 Date Reaffirmed: January 2016 Scope: SHR Acute, Parkridge Centre Any PRINTED version of this document is only accurate up to the date of printing 30-May-16. Saskatoon Health Region (SHR) cannot guarantee the currency or accuracy of any printed policy. Always refer to the Policies and Procedures site for the most current versions of documents in effect. SHR accepts no responsibility for use of this material by any person or organization not associated with SHR. No part of this document may be reproduced in any form for publication without permission of SHR. 1. PURPOSE 1.1 To safely and effectively use Oropharyngeal Airway (OPA). 2. POLICY 2.1 The Registered Nurse (RN), Registered Psychiatric Nurse (RPN), Licensed Practical Nurse (LPN), Graduate Nurse (GN), Graduate Psychiatric Nurse (GPN), Graduate Licensed Practical Nurse (GLPN) will insert, maintain, suction and remove an oropharyngeal airway (OPA). 2.2 The OPA may be inserted to establish and assist in maintaining a patent airway. 2.3 An OPA should only be used in patients with decreased level of consciousness or decreased gag reflex. 2.4 Patients with OPAs that have been inserted for airway protection should not be left unattended due to risk of aspiration if gag reflex returns unexpectedly. Page 1 of 4 Policies and Procedures: Airway – Oropharyngeal: Insertion; Maintenance; I.D. # 1159 Suction; Removal 3. PROCEDURE 3.1 Equipment: • Oropharyngeal airway of appropriate size • Tongue blade (optional) • Clean gloves • Optional: suction equipment, bag-valve-mask device 3.2 Estimate the appropriate size of airway by aligning the tube on the side of the patient’s face parallel to the teeth and choosing an airway that extends from the ear lobe to the corner of the mouth. -
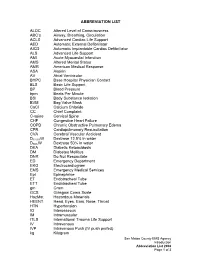
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

The Golden Hour > How Time Shapes Airway Management > by Charlie Eisele,BS,NREMT-P
September 2008 The A supplement to JEMS (the Journal of Emergency Medical Services) Conscience of EMS JOURNAL OF EMERGENCY MEDICAL SERVICES Sponsored by Verathon Inc. ELSEVIER PUBLIC SAFETY The Perfect View How Video Laryngoscopy Is Changing the Face of Prehospital Airway Management A supplement to September 2008 JEMS, sponsored by Verathon Inc. 4 Foreword > To See or Not to See, That Is the Question > By A.J.Heightman,MPA,EMT-P 5 5 The Golden Hour > How Time Shapes Airway Management > By Charlie Eisele,BS,NREMT-P 9 The Video Laryngoscopy Movement > Can-Do Technology at Work > By John Allen Pacey,MD,FRCSc 11 ‘Grounded’ Care > Use of Video Laryngoscopy in a Ground 11 EMS System: Better for You, Better for Your Patients > By Marvin Wayne,MD,FACEP,FAAEM 14 Up in the Air > Video Laryngoscopy Holds Promise for In-Flight Intubation > By Lars P.Bjoernsen,MD,& M.Bruce Lindsay,MD 16 16 The Military Experience > The GlideScope Ranger Improves Visualization in the Combat Setting > By Michael R.Hawkins,MS,CRNA 19 Using Is Believing > Highlights from 72 Cases Involving Video Laryngoscopy at Martin County (Fla.) Fire Rescue > By David Zarker,EMT-P 21 Teaching the Airway > Designing Educational Programs for 21 Emergency Airway Management > By Michael F.Murphy,MD; Ron M.Walls,MD; & Robert C.Luten,MD COVER PHOTO KEVIN LINK Disclosure of Author Relationships: Authors have been asked to disclose any relationships they may have with commercial supporters of this supplement or with companies that may have relevance to the content of the supplement. Such disclosure at the end of each article is intended to provide readers with sufficient information to evaluate whether any material in the supplement has been influenced by the writer’s relationship(s) or financial interests with said companies. -

Success Rate of Resuscitation After Out-Of-Hospital Cardiac Arrest
Commentary Success rate of resuscitation after out-of-hospital cardiac arrest Anthony MH Ho1, FRCPC, FCCP, Glenio B Mizubuti1 *, MSc, MD, Adrienne K Ho2, MB, BS, Song Wan3, MD, FRCS, Devin Sydor1, MD, FRCPC, David C Chung4, MD, FRCPC 1Department of Anesthesiology and Perioperative Medicine, Queen’s University, Canada 2Department of Oncology, The Christie NHS Foundation Trust, Manchester, United Kingdom 3Division of Cardiac Surgery, Department of Surgery, The Chinese University of Hong Kong, Shatin, Hong Kong 4Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Shatin, Hong Kong * Corresponding author: [email protected] Hong Kong Med J 2019;25:254–6 https://doi.org/10.12809/hkmj187596 A recent study in Hong Kong documented the low lack of which is linked to poor outcomes.5 However, success rate of resuscitation after adult out-of-hospital because 60% of adult and 38% of paediatric OHCAs cardiac arrest (OHCA). Survival to hospital discharge in Hong Kong are unwitnessed,1,4 these first few with good neurological outcome was 1.5%.1 A median minutes of sufficient oxygen in the blood (for sudden delay of 12 minutes for defibrillation was one factor arrest of cardiac origin) may have already elapsed. that contributed to poor outcomes.1 In ventricular This raises the question of whether a one-size-fits- fibrillation or pulseless ventricular tachycardia, every all bystander CPR with no breathing component minute without defibrillation drastically reduces is advisable. It is not surprising that the rates of the chance of successful resuscitation.2 To partially survival with good neurological outcomes are mitigate the delayed arrival of trained personnel to low. -

ECG, 12-Lead - Procedures P Paramedic Procedure
EMT A A-EMT ECG, 12-Lead - Procedures P Paramedic Procedure: q 1. Prepare ECG monitor and connect patient cable to electrodes q 2. Expose chest and prep as necessary. Modesty of the patient should be respected. q 3. Apply chest leads and extremity leads using the following landmarks: (Distal to shoulder and distal to hip joint for most accurate ECG) § RA: Right Arm § LA: Left Arm § RL: Right Leg § LL: Left Leg § V1: 4th intercostal space at right sternal border § V2: 4th intercostal space at left sternal border § V3: Directly between V2 and V4 § V4: 5th intercostal space at midclavicular line § V5: Level with V4 at left anterior axillary line § V6: Level with V5 at left midaxillary line q 4. Instruct patient to remain still, minimize artifact as able (examples include stopping motion of ambulance and instructing patient to remain still) q 5. Press the brand specific button to acquire the 12-Lead ECG (complete age and gender questions correctly) q 6. Provide 12 Lead to hospital staff, transmit when appropriate q 7. Document the procedure, time, and results on/with the PCR Procedures 146 EMT A A-EMT ECG, Right-Sided - Procedures P Paramedic To detect right ventricular STEMI associated with occlusion of the Right Coronary Artery, obtain a Right Sided ECG. Indications of a Right Ventricle Wall infarct may include: q ST elevation in the inferior leads, II, III and aVF § ST elevation that is greatest in lead III is especially significant q ST elevation in V1 (the only precordial lead that faces the RV on standard 12-lead ECG) q Right Bundle Branch Block, 2nd and 3rd Degree AV Blocks, ST elevation in V2 50% greater than the ST depression in aVF Procedure: q 1. -

Airway Administration Luke Koester AT, ATC, EMT
Airway Administration Luke Koester AT, ATC, EMT The primary function of an airway adjunct is to prevent obstruction of the upper airway by the tongue and allow the passage of air and oxygen to the lungs Nasopharyngeal Airways (NPA) -used in an unresponsive patient or a patient with an altered level of consciousness who has an intact gag reflex and is not able to maintain their airway spontaneously -patients with AMS or who have just had a seizure may also benefit from a NPA Indications Contraindications 1. semiconscious or unconscious patients with an 1. Severe head injury with blood draining from the nose intact gag reflex 2. History of fractured nasal bone 2. patients who otherwise will not tolerate an OPA *If the NPA is accidentally pushed through a hole caused by a fracture of the base of the skull (cribiform plate), it may penetrate into the brain -Inserting a Nasopharyngeal Airway 1. Size the airway by measuring from the tip of the nose to the patient’s earlobe 2. Coat the tip with a water-soluble lubricant 3. Insert the NPA into the right nare with the bevel facing the septum a. If there is trauma to the right nare, invert the NPA so the bevel is facing the septum and insert into the left nare 4. Advance the airway until the flange rests against the nostril a. If using the left nare, advance the NPA until resistance is met, then rotate the NPA 180 degrees into position until the flange rests against the nostril Oropharyngeal Airways (OPA) -used to keep the tongue from blocking the upper airway -makes it easier to suction the oropharynx if necessary Indications Contraindications 1. -

07/01/2021 Airway Management Policy #7000 I. Purpose
Imperial County Public Health Department Emergency Medical Services Agency Policy/Procedure/Protocol Manual Medical Procedure Date: 07/01/2021 Airway Management Policy #7000 I. Purpose: A. To establish indications, guidelines, and the standard procedure for airway management in the pre-hospital setting. II. Authority: A. Health and Safety Code, Section 1797.220, 1798. Title 22, Section 100170. III. Policy: A. The use of airway interventions is limited by certification skill level, and requires annual maintenance and testing completion. B. This policy is to be used when identifying need for airway, breathing or ventilation support, with a current or impending issue. C. Endotracheal intubation is the preferred method of airway management in adults who are suffering from respiratory arrest or failure. In pediatric patients Bag Valve Mask (BVM) ventilation is the preferred method of airway management. 1. Pediatric patients for the purposes of airway management are able to be measured by pediatric length-based tape (or equivalent). If the patient is greater than the length of the pediatric length-based tape, which corresponds to approximately 40 kg, the patient can generally fall under adult airway management, as clinically determined to be appropriate by the managing provider. D. BLS personnel may use OPAs/NPAs (oropharyngeal airways and nasopharyngeal airways) but the use endotracheal or esophageal/tracheal double lumen airway devices (ETDLA) is reserved for ALS personnel, or those with specialized certification. E. Any patient undergoing an airway procedure should have the maximum level of monitoring present including: 1. Pulse oximetry and frequent blood pressure measurements 2. ECG tracing and continuous capnography if ALS present F. -

Airway Management Milwaukee Challenges in Airway Patency
8/22/2014 Airway Management Does this patient need an emergent airway? Milwaukee Challenges in airway patency Tongue Blood Dental Trauma Vomit Distorted Landmarks Reflex Jaw Spasm C-Spine Injury 1 8/22/2014 Immediate Assessment Parameters Adequacy of current ventilation Patency of airway Duration of hypoventilation Need for paralyzing agents C-Spine injury Equipment and Experience Airway Stabilization Techniques Positioning to relieve tongue obstruction Chin Lift or Jaw Thrust (No Neck lift, or extension!!) Elevated head position EAC to sternal notch Elevate with sheets or blanket Nasopharyngeal Airway Prevent tongue from obstructing airway Frees the operator to do other things Insertion technique simple 2 8/22/2014 Nasal Intubation? LaFort III Fracture I wouldn’t Suboptimal intubation Oropharyngeal Airway Prevents tongue from obstructing airway Insert inverted along hard palate then twist Size by corner of mouth to EAC 3 8/22/2014 Bag-Valve-Mask May be the most important airway skill Tight Mask seal is mandatory Two man technique best Incidence of impossible BVM? Cyclists are ideal patients!! Gastric distention… overly concerned Oxygenation Technique Slow 1-2 second breaths TV goal 450cc, every 5 seconds, 12BPM Cricoid pressure? Role for paralytics? Oxygen flow NODESAT technique NC @15LPM Place a nasal cannula too? Definitive Airway Indications Coma and lack of gag reflex (GCS<8) Severe facial trauma Aspiration Risk Expanding neck hematoma, edema or stridor Impending respiratory failure Hypoxia or inability to adequately ventilate with -
Basic Trauma Overview - ABC
Basic Trauma Overview - ABC Dale Dangleben, MD, FACS 1 2 Team 3 Extended Team 4 Team Leader Decrease chaos / optimize care. – Remains calm – Maintains control and provides direction – Stays decisive – Sees the big picture (situational awareness) – Is open to other team members input – Directs resuscitation – Makes early decision to transfer the patients that exceed the local capabilities 5 Team Members − Know your roles in the trauma team − Remain calm − Be responsive to team leader −Voice suggestions or concerns 6 Responsibilities – Perform the Primary and secondary survey – Verbalize patient care – Report completed tasks 7 Responsibilities – Monitors the patient – Manual BP – Obtains IV access – Administers medications – Dresses wounds – Performs or assists in resuscitative procedures 8 Responsibilities Records data Ensures documentation accompanies patient upon transfer Assists team members as needed 9 Responsibilities – Obtains needed supplies – Coordinates communication with local and external resources – Assists team members as needed 10 Responsibilities • Place Oxygen on patient • Manage airway • Hold C spine • Manage ventilator if • Manage rapid infuser line patient intubated where indicated • Assists team members as needed 11 Organization of trauma resuscitation area – Basic adult and pediatric equipment for: • Airway management (cart) • IV access with warm fluids • Chest tube insertion • Hemorrhage control (tourniquets, pelvic binders) • Immobilization • Medications • Pediatric length/weight based tape (Broselow Tape) – Warming -

Basic Airway Management & Decision Making
Roberts: Clinical Procedures in Emergency Medicine, 5th ed. CHAPTER 3 – Basic Airway Management and Decision-Making Robert F. Reardon, Phillip E. Mason, Joseph E. Clinton Over the last few decades, several important changes have occurred in emergency airway management. Bag-mask ventilation has been supplemented by intermediate, or backup, ventilation devices like the laryngeal mask airway (LMA), the Combitube, and the laryngeal tube. These have become important devices for the initial resuscitation of apneic patients and for rescue ventilation when intubation fails.[1] Noninvasive positive-pressure ventilation (NPPV) is now used in place of tracheal intubation in some critically ill patients. Despite these advances, basic techniques such as opening the airway, oxygenation, and bag-mask ventilation remain the cornerstones of good emergency airway management. [2] [3] Airway maintenance without endotracheal intubation is one of the most important emergency [4] airway management techniques to keep patients alive until a definitive airway can be established. This chapter describes basic airway skills including opening the airway, O2 therapy, NPPV, bag-mask ventilation, and intermediate ventilation devices. Because of the complexity of these skills and decisions, providers should develop a simple, organized approach to emergency airway management, being cognizant that when a specific intervention has failed, it is time to move rapidly to a different approach. Developing a simple preconceived algorithm that employs proven techniques and is applicable to a broad range of clinical scenarios will help providers manage difficult, anxiety-provoking emergency airways. THE CHALLENGE OF EMERGENCY AIRWAY MANAGEMENT Although other specialists are sometimes available, most emergency airways are managed by emergency clinicians.[5] Airway management in the emergency department (ED) is much different from airway management in the controlled setting of the operating room. -

9 Nasopharyngeal and Oral Airway Insertion 63
PROCEDURE Nasopharyngeal and Oral 9 Airway Insertion Kimberly Wright PURPOSE: Nasopharyngeal and oral airways are used to provide short-term airway maintenance and to facilitate the removal of tracheobronchial secretions. 5 PREREQUISITE NURSING ❖ Patients with obstructed nasal passageways ❖ Patients with suspected basilar skull or cribriform plate KNOWLEDGE 5 fracture Nasopharyngeal Airway ❖ Patients with facial trauma that prevents the safe inser- • Nasopharyngeal airways are inserted into a single naris tion or use of the airway 3,5 and passed into the posterior oropharynx to the base of the tongue ( Fig. 9-1 ). 2 Oropharyngeal Airway • The nasopharyngeal airway has three parts: the fl ange, • Oropharyngeal airways are typically disposable, curved, cannula, and bevel or tip. The fl ange is the wide trumpet- plastic or hard rubber devices with an opening or channel like end that prevents further slippage into the airway. The to facilitate suctioning. 1 hollow shaft of the cannula permits airfl ow into the hypo- • The oropharyngeal airway is placed over the tongue. The pharynx. The bevel or tip is the opening at the distal end curvature or body of the airway displaces the tongue of the tube. When the correct size is properly inserted, the forward from the posterior pharyngeal wall, a common fl ange will rest against the patient ’ s naris 3 and the tip can site of airway obstruction. be seen resting posterior to the base of the tongue. • An oropharyngeal airway has four parts: the fl ange, body, • The external diameter of the nasopharyngeal airway tip, and channel ( Fig. 9-3 ). The fl ange rests against the should be slightly smaller than the patient’ s external nares lips.