Airway Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -
Spring 2009 Student Journal
Volume 8 Number 1 Spring 2009 The International Student Journal of Nurse Anesthesia TOPICS IN THIS ISSUE MS & ECT Cardioprotection of Volatile Agents Hyperthermic Chemotherapy Intubating LMA Pierre Robin Syndrome Alpha Thalassemia Latex Allergy & Spina Bifida Distorted Upper Airway Volunteerism – Honduras INTERNATIONAL STUDENT JOURNAL OF NURSE ANESTHESIA Vol. 8 No. 1 Spring 2009 Editor - in - Chief Ronald L. Van Nest, CRNA, JD Associate Editors Vicki C. Coopmans, CRNA, PhD Julie A. Pearson, CRNA, PhD EDITORIAL BOARD & SECTION EDITORS Pediatrics Janet A. Dewan, CRNA, MS Northeastern University Obstetrics Greg Nezat, CRNA, PhD Navy Nurse Corps Anesthesia Program Research & Capstone Joseph E. Pellegrini, CRNA, University of Maryland PhD Regional / Pain Christopher Oudekerk, CRNA, Uniformed Services Universi- DNP ty of the Health Sciences Cardiovascular Michele Gold, CRNA, PhD University of Southern Cali- fornia Thoracic/ Fluid Balance Lori Ann Winner, CRNA, MSN University of Pennsylvania Unique Patient Syndromes Kathleen R. Wren, CRNA, PhD Florida Hospital College of Health Sciences Equipment Carrie C. Bowman Dalley, Georgetown University CRNA, MS Pharmacology Maria Magro, CRNA, MS, University of Pennsylvania MSN Pathophysiology JoAnn Platko, CRNA, MSN University of Scranton Special Surgical Techniques Russell Lynn, CRNA, MSN University of Pennsylvania 1 Airway & Respiration Michael Rieker, CRNA, DNP Wake Forest University Baptist Medical Center ,Nurse Anesthesia Program, Univer- sity of North Carolina at Greensboro Neurology & Neurosurgery -
TCCC CLS Skill Instructions Mod 7 25 JAN 20
MODULE 07: AIRWAY MANAGEMENT IN TFC SKILL INSTRUCTIONS 25 JAN 2020 COMBAT LIFESAVER (CLS) TACTICAL COMBAT CASUALTY CARE SKILL INSTRUCTIONS HEAD-TILT/CHIN-LIFT INSTRUCTION TASK: Open an airway using the head-tilt/chin-lift maneuver CONDITION: Given a simulated scenario where a casualty and responder are in combat gear and the casualty is unconscious without a patent airway STANDARD: EffeCtively open the airway by performing the head-tilt/chin-lift maneuver following all steps and measures correctly without Causing further harm to the Casualty EQUIPMENT: N/A PERFORMANCE MEASURES: step-by-step instructions NOTE: Do not use if a spinal or neck injury is suspected. 01 Roll the Casualty onto their back, if necessary, and place them on a hard, flat surface. 02 Kneel at the level of the Casualty’s shoulders. Position yourself at the side of the Casualty. 03 Open the mouth and looK for visible airway obstruCtions (e.g., laCerations, obstructions, broken teeth, burns, or swelling or other debris, such as vomit). NOTE: If foreign material or vomit is in the mouth, remove it as quiCKly as possible. NOTE: Do not perform a blind finger sweep. 04 PlaCe one hand on the Casualty's forehead and apply firm, backward pressure with the palm to tilt the head back. 05 PlaCe the fingertips of the other hand under the bony part of the lower jaw and lift, bringing the Chin forward. NOTE: Do not use the thumb to lift the chin. 06 While maintaining the open airway position, place an ear over the casualty's mouth and nose, looking toward the chest and stomaCh. -

Tracheal Intubation Following Traumatic Injury)
CLINICAL MANAGEMENT UPDATE The Journal of TRAUMA Injury, Infection, and Critical Care Guidelines for Emergency Tracheal Intubation Immediately after Traumatic Injury C. Michael Dunham, MD, Robert D. Barraco, MD, David E. Clark, MD, Brian J. Daley, MD, Frank E. Davis III, MD, Michael A. Gibbs, MD, Thomas Knuth, MD, Peter B. Letarte, MD, Fred A. Luchette, MD, Laurel Omert, MD, Leonard J. Weireter, MD, and Charles E. Wiles III, MD for the EAST Practice Management Guidelines Work Group J Trauma. 2003;55:162–179. REFERRALS TO THE EAST WEB SITE and impaired laryngeal reflexes are nonhypercarbic hypox- Because of the large size of the guidelines, specific emia and aspiration, respectively. Airway obstruction can sections have been deleted from this article, but are available occur with cervical spine injury, severe cognitive impairment on the Eastern Association for the Surgery of Trauma (EAST) (Glasgow Coma Scale [GCS] score Յ 8), severe neck injury, Web site (www.east.org/trauma practice guidelines/Emergency severe maxillofacial injury, or smoke inhalation. Hypoventi- Tracheal Intubation Following Traumatic Injury). lation can be found with airway obstruction, cardiac arrest, severe cognitive impairment, or cervical spinal cord injury. I. STATEMENT OF THE PROBLEM Aspiration is likely to occur with cardiac arrest, severe cog- ypoxia and obstruction of the airway are linked to nitive impairment, or severe maxillofacial injury. A major preventable and potentially preventable acute trauma clinical concern with thoracic injury is the development of Hdeaths.1–4 There is substantial documentation that hyp- nonhypercarbic hypoxemia. Lung injury and nonhypercarbic oxia is common in severe brain injury and worsens neuro- hypoxemia are also potential sequelae of aspiration. -
Prehospital Airway Management Using the Laryngeal Tube an Emergency Department Point of View
Notfallmedizin Anaesthesist 2014 · 63:589–596 M. Bernhard1 · W. Beres2 · A. Timmermann3 · R. Stepan4 · C.-A. Greim5 · U.X. Kaisers6 · DOI 10.1007/s00101-014-2348-1 A. Gries1 Published online: 2. Juli 2014 1 Emergency Department, University Hospital of Leipzig, Leipzig © Springer-Verlag Berlin Heidelberg 2014 2 Department of Anaesthesiology and Intensive Care Medicine, Main Klinik Ochsenfurt, Ochsenfurt 3 Department of Anaesthesiology, Pain Therapy, Intensive Care Medicine and Emergency Medicine, DRK Kliniken Berlin Westend und Mitte, Berlin Redaktion 4 Department of Public Health, Fulda County, Fulda A. Gries, Leipzig 5 Department of Anesthesiology, Intensive Care Medicine and Emergency Medicine, Hospital of Fulda, Fulda V. Wenzel, Innsbruck 6 Department of Anesthesiology and Intensive Care Medicine, University Leipzig, Medical Faculty, Leipzig Prehospital airway management using the laryngeal tube An emergency department point of view Securing the airway and maintaining ox- Studies describing the successful use of mittee of the Medical Faculty of Leipzig, ygenation and ventilation represent es- the laryngeal tube in the prehospital setting Germany. Single cases were documented sential life-saving strategies in emergen- sound promising [9, 10, 22]. However, the initially after ED admission. The case se- cy medicine [1, 2, 3, 40]. Depending on results of these studies and of case reports ries was evaluated retrospectively, was not the experience of the person performing were not reported by an independent ob- preregistered, and written informed con- the procedure and on the individual in- server and, therefore, reporting bias could tent could not be obtained. tubation conditions, endotracheal intuba- be possible [11, 22]. Only one prospective, tion (ETI) is still considered to be the gold randomized study has confirmed that the Results standard [4, 5, 40]. -

Airway – Oropharyngeal: Insertion; Maintenance; Suction; Removal
Policies & Procedures Title: AIRWAY – OROPHARYNGEAL: INSERTION; MAINTENANCE; SUCTION; REMOVAL I.D. Number: 1159 Authorization Source: Nursing Date Revised: September 2014 [X] SHR Nursing Practice Committee Date Effective: October 2002 Date Reaffirmed: January 2016 Scope: SHR Acute, Parkridge Centre Any PRINTED version of this document is only accurate up to the date of printing 30-May-16. Saskatoon Health Region (SHR) cannot guarantee the currency or accuracy of any printed policy. Always refer to the Policies and Procedures site for the most current versions of documents in effect. SHR accepts no responsibility for use of this material by any person or organization not associated with SHR. No part of this document may be reproduced in any form for publication without permission of SHR. 1. PURPOSE 1.1 To safely and effectively use Oropharyngeal Airway (OPA). 2. POLICY 2.1 The Registered Nurse (RN), Registered Psychiatric Nurse (RPN), Licensed Practical Nurse (LPN), Graduate Nurse (GN), Graduate Psychiatric Nurse (GPN), Graduate Licensed Practical Nurse (GLPN) will insert, maintain, suction and remove an oropharyngeal airway (OPA). 2.2 The OPA may be inserted to establish and assist in maintaining a patent airway. 2.3 An OPA should only be used in patients with decreased level of consciousness or decreased gag reflex. 2.4 Patients with OPAs that have been inserted for airway protection should not be left unattended due to risk of aspiration if gag reflex returns unexpectedly. Page 1 of 4 Policies and Procedures: Airway – Oropharyngeal: Insertion; Maintenance; I.D. # 1159 Suction; Removal 3. PROCEDURE 3.1 Equipment: • Oropharyngeal airway of appropriate size • Tongue blade (optional) • Clean gloves • Optional: suction equipment, bag-valve-mask device 3.2 Estimate the appropriate size of airway by aligning the tube on the side of the patient’s face parallel to the teeth and choosing an airway that extends from the ear lobe to the corner of the mouth. -
Scope of Practice Statements
Scope of Practice Statements Emergency Medical Services Authority California Health and Human Services Agency EMSA # 300 November 2017 HOWARD BACKER, MD, MPH, FACEP DIRECTOR DANIEL R. SMILEY CHIEF DEPUTY DIRECTOR SEAN TRASK DIVISION CHIEF EMSA # 300 Released November 2017 EMSA #300 • Page 1 Table of Contents Introduction ........................................................................................................................................... 4 The EMS Authority ................................................................................................................................ 4 Local EMS Agencies ............................................................................................................................. 4 California EMS Personnel Levels .......................................................................................................... 4 Reading the Scope of Practice Pages .................................................................................................. 5 Airway and Breathing ............................................................................................................................ 6 Airway Suctioning .............................................................................................................................. 7 Automatic Transport Ventilator .......................................................................................................... 8 Bag Valve Mask – BVM .................................................................................................................... -

Authors Conducted an E-Mail Survey of Anesthesiologists in the US in 2010
Appendix 2: Reference 1 Methods: Authors conducted an e-mail survey of Anesthesiologists in the US in 2010. Results: “Five thousand anesthesiologists were solicited; 615 (12.3%) responses were received. Twenty-four percent of respondents had installed an AIMS, while 13% were either installing a system now or had selected one, and an additional 13% were actively searching. Larger anesthesiology groups with large case loads, urban settings, and government affiliated or academic institutions were more likely to have adopted AIMS. Initial cost was the most frequently cited AIMS barrier. The most commonly cited benefit was more accurate clinical documentation (79%), while unanticipated need for ongoing information technology support (49%) and difficult integration of AIMS with an existing EMR (61%) were the most commonly cited problems.” [Trentman TL, Mueller JT, Ruskin KJ, Noble BN, Doyle CA. Adoption of anesthesia information management systems by US anesthesiologists. J Clin Monit Comput 2011;25:129–35.] Reference 2 Joint Commission Report. 60 [Kohn L, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Report from the Committee on Quality of Health Care in America. Washington DC: The Joint Commission journal on quality improvement, 1999:227–34.] Reference 3 Excerpt: “The Department of Health and Human Services (DHHS) released two proposed regulations affecting HIT (www.healthit.hhs.gov). The first, a notice of proposed rule- making (NPRM), describes how hospitals, physicians, and other health care professionals can qualify for billions of dollars of extra Medicare and Medicaid payments through the meaningful use of electronic health records (EHRs). The second, an interim final regulation, describes the standards and certification criteria that those EHRs must meet for their users to collect the payments. -

Airway Management for COVID 19
Airway Management in Critically Ill COVID-19 Patients KATHERINE HELLER, MD ASSISTANT PROFESSOR UNIVERSITY OF WASHINGTON SCHOOL OF MEDICINE DEPARTMENT OF ANESTHESIOLOGY MEDICAL DIRECTOR: UWMC SICU Disclosures (none) Outline Staff safety PPE Patient factors/ timing Adjuncts for oxygenation Intubation procedure Preparation Equipment/technique Unusual situations Difficult airways Tracheostomy Emergencies Opening Questions Please navigate to pollev.com/katherinehel603 Priorities Priority #1: Staff Safety Considerations for Staff Procedural planning Appropriate PPE takes time Avoid emergencies when able Consider rounding (remotely?) on known COVID patients PPE Any airway management is an Aerosol Generating Procedure (AGP) Need respirator level protections airborne + contact/droplet N95 vs PAPR N95 PAPR Pro Pro Easy to don Comfortable Fast Protect face, neck, head Allow use of stethoscope Reusable More readily available Con Con Allows contamination of Require power source face and neck Need assistance to don Less comfortable and doff May not fit everyone Noisy Fit can change Infection Control Choose what work for you and your institution More important to have clear protocols and expectations Minimize in room staff Have equipment easily available Filter in line on circuit Infection control Barrier Devices Not recommended Additional encumbrance to intubation without proven benefit Not a replacement for PPE May actually increase risk [11] Failed airway Breach of PPE FDA revoked EUA for barrier devices in -

Evaluation of Different Positive End-Expiratory Pressures Using Supreme™ Airway Laryngeal Mask During Minor Surgical Procedure
medicina Article Evaluation of Different Positive End-Expiratory Pressures Using Supreme™ Airway Laryngeal Mask during Minor Surgical Procedures in Children Mascha O. Fiedler 1,* , Elisabeth Schätzle 2, Marius Contzen 3, Christian Gernoth 4, Christel Weiß 5, Thomas Walter 6, Tim Viergutz 2 and Armin Kalenka 7 1 Clinic of Anesthesiology, Heidelberg University Hospital, 69120 Heidelberg, Germany 2 Clinic of Anesthesiology and Surgical Intensive Care Medicine, University Medical Centre Mannheim, 68167 Mannheim, Germany; [email protected] (E.S.); [email protected] (T.V.) 3 Department of Anesthesiology and Intensive Care Medicine, Heilig-Geist-Hospital Bensheim, 64625 Bensheim, Germany; [email protected] 4 Department of Anesthesiology, Surgical Intensive Care Medicine, Pain Therapy, Helios Hospital Duisburg, 47166 Duisburg, Germany; [email protected] 5 Department of Medical Statistics, University Medical Centre Mannheim, 68167 Mannheim, Germany; [email protected] 6 Emergency Department, University Medical Centre Mannheim, 68167 Mannheim, Germany; [email protected] 7 Department of Anesthesiology and Intensive Care Medicine, Hospital Bergstrasse, 64646 Heppenheim, Germany; [email protected] * Correspondence: mascha.fi[email protected]; Tel.: +49-(0)-6222-1563-9434 Received: 21 September 2020; Accepted: 19 October 2020; Published: 21 October 2020 Abstract: Background and objectives: The laryngeal mask is the method of choice for airway management in children during minor surgical procedures. There is a paucity of data regarding optimal management of mechanical ventilation in these patients. The Supreme™ airway laryngeal mask offers the option to insert a gastric tube to empty the stomach contents of air and/or gastric juice. -

The Laryngeal Mask Airway: Potential Applications in Neonates
F485 Arch Dis Child Fetal Neonatal Ed: first published as 10.1136/adc.2003.038430 on 21 October 2004. Downloaded from PERSONAL PRACTICE The laryngeal mask airway: potential applications in neonates D Trevisanuto, M Micaglio, P Ferrarese, V Zanardo ............................................................................................................................... Arch Dis Child Fetal Neonatal Ed 2004;89:F485–F489. doi: 10.1136/adc.2003.038430 The laryngeal mask airway is a safe and reliable airway 2.5–5 kg.11 It has been postulated that a smaller size (0.5) could be useful in preterm management device. This review describes the insertion newborns. However, there are reports of techniques, advantages, limitations, and potential successful use of size 1 in preterm neonates applications of the laryngeal mask airway in neonates. weighing 0.8–1.5 kg.12–15 ........................................................................... (2) Fully deflate the cuff as described in the manual, and lubricate the back of the mask tip (for neonates in the labour ward, he ability to maintain a patent airway and lubrication may not be necessary, as oral provide effective positive pressure ventilation and pharyngeal secretions may reproduce T(PPV) is the main objective of neonatal this function). resuscitation and all anaesthesiological proce- (3) Press (flatten) the tip of the LMA against the dures.1–6 This is currently achieved with the use hard palate. During this manoeuvre, the of a face mask or an endotracheal tube. Both of these devices have major limitations from a operator should grasp the LMA like a pen strictly anatomical point of view and require with the index finger at the junction adequate operator skills. In certain situations, between the mask and the distal end of the both face mask ventilation and tracheal intuba- airway tube. -
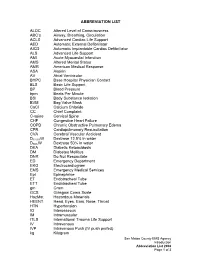
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt.