Synthesis and Structure Activity Relationship of Some Indole Derivatives As Potential Anti-Inflammatory Agents Samar S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Acemetacin.Pdf
Methods and Findings in Experimental and Clinical Pharmacology 2010, 32(2): ???-??? THOMSON REUTERS Copyright © 2010 Prous Science, S.A.U. or its licensors. All rights reserved. CCC: 0379-0355/2010 DOI: 10.1358/mf.2010.32.2.1423883 ORIGINAL ARTICLE ACEMETACIN ANTINOCICEPTIVE MECHANISM IS NOT RELATED TO NO OR K+ CHANNEL PATHWAYS. M. Gil-Flores1, M.I. Ortiz2, G. Castañeda-Hernández1 and A.E. Chávez-Piña1 1Departamento de Farmacología, Centro de Investigación y de Estudios Avanzados del Instituto Politécnico Nacional, México, D.F., México. 2Área Académica de Medicina del Instituto de Ciencias de la Salud, Universidad Autónoma del Estado de Hidalgo, Pachuca, Hidalgo, México SUMMARY Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) used for the treatment of acute gout and inflammation. However, its use is limited due to side effects. Acemetacin is a prodrug of indomethacin that exhibits better gastric tolerability in preclinical and clinical tri- als. The aim of this study was to examine if the systemic administration of acemetacin involved the sequential participation of nitric oxide (NO) or K+ channel pathways to confer its antinociceptive effect, as compared to indomethacin. The antinociceptive effect of both drugs was studied with the formalin test. Equimolar doses of acemetacin or indomethacin were administered orally. The intraplantar administra- tion of either L-NAME, glibenclamide, apamin or charybdotoxin plus indomethacin or acemetacin was studied using the formalin test and the anti-inflammatory and antihyperalgesic effects were measured. The antinociceptive effect of acemetacin or indomethacin was not sig- nificantly different when pretreatment with L-NAME, glibenclamide, apamin or charybdotoxin was done. The antihyperalgesic and anti- inflammatory effects were also similar for both indomethacin and acemetacin. -

Binding of Nonsteroidal Anti-Inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects
4132 Langmuir 2008, 24, 4132-4139 Binding of Nonsteroidal Anti-inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects Marlene Lu´cio,*,†,⊥ Frank Bringezu,‡,|,⊥ Salette Reis,† Jose´ L. F. C. Lima,† and Gerald Brezesinski§,⊥ REQUIMTE, Faculdade de Farma´cia, UniVersidade do Porto, Rua Anı´bal Cunha, 4099-030 Porto, Portugal, Institute of Medical Physics and Biophysics, UniVersity of Leipzig, Ha¨rtelstrasse 16, D-04103 Leipzig, Germany, and Max-Planck Institute of Colloids and Interfaces, Research Campus Golm, Am Mu¨hlenberg 1, D-14476 Potsdam, Germany ReceiVed NoVember 16, 2007. In Final Form: January 8, 2008 The effect of nonsteroidal anti-inflammatory drugs (NSAIDs) on the phase transition and phase properties of 1,2-dipalmitoylphosphatidylcholine (DPPC) has been investigated in both 2D (monolayers at the air/water interface) and 3D (multilayers in lipid/water dispersions) model systems. The 2D membrane models have been characterized by means of pressure-area isotherms and grazing incidence X-ray diffraction (GIXD) measurements. Differential scanning calorimetry (DSC) and simultaneous small- and wide-angle X-ray diffraction have been applied to lipid aqueous dispersions. All NSAIDs studied altered the main transition temperature of the gel to liquid-crystalline phase transition, with the arylacetic acid derivatives (acemetacin and indomethacin) showing the largest effects. A comparison of the results reveals distinct structural features of the membrane models after interaction with the NSAID. All drugs induced perturbations in the lipid liquid-crystalline phase, suggesting a major change in the hydration behavior of DPPC. Again, the largest effects on the structural parameters are found for the arylacetic acid derivatives. The results obtained in the different model systems give indications of the role of the membrane/NSAID interactions that might also be important for NSAID gastric injury. -
Download Product Insert (PDF)
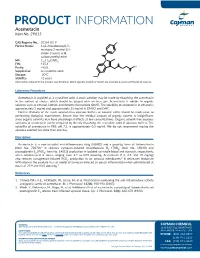
PRODUCT INFORMATION Acemetacin Item No. 29615 CAS Registry No.: 53164-05-9 Cl Formal Name: 1-(4-chlorobenzoyl)-5- methoxy-2-methyl-1H- indole-3-acetic acid, O carboxymethyl ester N MF: C21H18ClNO6 FW: 415.8 O OH Purity: ≥98% O Supplied as: A crystalline solid O Storage: -20°C O Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Acemetacin is supplied as a crystalline solid. A stock solution may be made by dissolving the acemetacin in the solvent of choice, which should be purged with an inert gas. Acemetacin is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of acemetacin in ethanol is approximately 3 mg/ml and approximately 25 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of acemetacin can be prepared by directly dissolving the crystalline solid in aqueous buffers. The solubility of acemetacin in PBS, pH 7.2, is approximately 0.5 mg/ml. We do not recommend storing the aqueous solution for more than one day. Description Acemetacin is a non-steroidal anti-inflammatory drug (NSAID) and a prodrug form of indomethacin 1 (Item No. 70270). It reduces zymosan-induced thromboxane B2 (TXB2; Item No. 19030) and prostaglandin E2 (PGE2; Item No. 14010) production in isolated rat whole blood and stomach, respectively, when administered at doses ranging from 2.7 to 83.8 µmol/kg. -

The Challenge of Drug-Induced Aseptic Meningitis Revisited
Letters cardioverter-defibrillator generator replacements and upgrade procedures: brospinal fluid (CSF) findings and reviews added to the litera- results from the REPLACE registry. Circulation. 2010;122(16):1553-1561. ture from 1999 to date. Tables have been assembled from 6. Kramer DB, Buxton AE, Zimetbaum PJ. Time for a change: a new approach to information derived from 192 studies (these data are avail- ICD replacement. N Engl J Med. 2012;366(4):291-293. able from the authors on request). The Challenge of Drug-Induced Aseptic Results | Four groups of drugs continue to be associated Meningitis Revisited with DIAM (Table 1): nonsteroidal anti-inflammatory Cases of drug-induced aseptic meningitis (DIAM) are likely drugs (NSAIDs), antibiotics, immunosuppressive- underreported, and only a few reviews of the literature have immunomodulatory (IS-IM), and antiepileptic drugs.1 Prior been performed. We have updated (to February 2014) a pre- exposure to the associated drug was present in 26% to 35% vious review (1999)1 to identify newer agents associated with of cases (Table 1). The interval between exposure and men- DIAM, as well as distinctive new features. ingitis ranged from minutes to 5 months (Table 1). Most patients presented with headache, fever, meningismus, and Methods | Using the MEDLINE database, we searched the lit- mental status changes (Table 2). Underlying systemic disor- erature to February 2014 and included those cases with cere- ders were often present, particularly systemic lupus ery- Table 1. Drugs Involved in Drug-Induced -

DAYPRO ALTA™ (Oxaprozin Potassium) 600Mg Tablets Cardiovascular Risk • Nsaids May Cause an Increased Risk of Serious Cardiov
DAYPRO ALTA™ (oxaprozin potassium) 600mg tablets Cardiovascular Risk NSAIDs may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patient’s with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk (see WARNINGS). Daypro ALTA is contraindicated for treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery (see WARNINGS). Gastrointestinal Risk NSAID’s cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events (see WARNINGS). DESCRIPTION DAYPRO ALTA (oxaprozin potassium tablets) is a member of the propionic acid group of nonsteroidal anti-inflammatory drugs (NSAIDs). Each blue, capsule-shaped tablet contains oxaprozin potassium (678mg equivalent to 600mg of oxaprozin) for oral administration. The chemical name for oxaprozin potassium is 4,5-diphenyl-2-oxazolepropionic acid, potassium salt. Its empirical formula is C18H14NO3K, and molecular weight is 331. Oxaprozin potassium is a white to off white powder with a melting point of 215°C. It is slightly soluble in alcohol and very soluble in water. The PK in water is 9.7. It has the following structural formula: Inactive ingredients in DAYPRO ALTA tablets include microcrystalline cellulose, hydroxypropyl methylcellulose, pregelatinized corn starch, stearic acid, colloidal silicon dioxide, polyethylene glycol, titanium dioxide, FD&C Blue #1 Aluminum Lake, and pharmaceutical glaze. -

Mefenamic Acid Induced Autoimmune Hemolytic Anemia- a Case Report
The Journal of Medical Research 2020; 6(3): 67-69 Case Report Mefenamic acid induced autoimmune hemolytic anemia- A case JMR 2020; 6(3): 67-69 report May- June ISSN: 2395-7565 Reshmi Mishra1, Sarbeswar Pradhan2, Mahendravarma Madduri Reshmi Mishra3 © 2020, All rights reserved 1 Department of Pediatrics, Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar- 751024, Odisha, India www.medicinearticle.com 2 Associate Professor, Department of Pediatrics, Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar- Received: 15-05-2020 751024, Odisha, India Accepted: 13-06-2020 3 2nd Year PG, Department of Pediatrics, Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar- 751024, Odisha, India Abstract Immune hemolytic anemia (IHA) is an uncommon adverse effect of a wide variety of drugs. The incidence is on the rise due to the extensive use of nonsteroidal anti-inflammatory drugs (NSAID). Mefenamic acid is the most common among NSAIDs causing AIHA by an autoimmune mechanism. We are presenting a case of three years old child presented with history dark colored urine, severe anemia, and jaundice after taking mefenamic acid for fever. Investigations revealed leucocytosis, hyperbilirubinemia, raised reticulocyte count, and negative direct Coombs test. The urinalysis demonstrated proteinuria, hematuria, and pus cell of 18-20/HPF. The urine for free hemoglobin was positive. As all the clinical, as well as investigation reports, were suggestive of the autoimmune hemolytic anemia except for the negative cooms test, the child was diagnosed to be a case of Coombs-negative autoimmune hemolytic anemia (Mefenamic induced) with urosepsis. He was managed conservatively by withdrawing the offending drug, and the latter steroid was added. -

Original Paper Enhancement of Chemotherapeutic Drug Toxicity To
European Journal of Cancer, Vol. 34, No. 8, pp. 1250±1259, 1998 # 1998 Elsevier Science Ltd. All rights reserved Pergamon Printed in Great Britain 0959-8049/98 $19.00+0.00 PII: S0959-8049(98)00045-8 Original Paper Enhancement of Chemotherapeutic Drug Toxicity to Human Tumour Cells In Vitro by a Subset of Non-steroidal Anti-in¯ammatory Drugs (NSAIDs) C.P. DuVy, C.J. Elliott, R.A. O'Connor, M.M. Heenan, S. Coyle, I.M. Cleary, K. Kavanagh, S. Verhaegen, C.M. O'Loughlin, R. NicAmhlaoibh and M. Clynes National Cell and Tissue Culture Centre, Dublin City University, Glasnevin, Dublin 9, Ireland The eVect on cytotoxicity of combining a range of clinically important non-steroidal anti-in¯amma- tory drugs (NSAIDs) with a variety of chemotherapeutic drugs was examined in the human lung cancer cell lines DLKP, A549, COR L23P and COR L23R and in a human leukaemia line HL60/ADR. A speci®c group of NSAIDs (indomethacin, sulindac, tolmetin, acemetacin, zomepirac and mefenamic acid) all at non-toxic levels, signi®cantly increased the cytotoxicity of the anthracyclines (doxorubicin, daunorubicin and epirubicin), as well as teniposide, VP-16 and vincristine, but not the other vinca alkaloids vinblastine and vinorelbine. Asubstantial number of other anticancer drugs, including methotrexate, 5-¯uorouracil, cytarabine, hydroxyurea, chlorambucil, cyclophosphamide, cisplatin, carboplatin, mitoxantrone, actinomycin D, bleomycin, paclitaxel and camptothecin, were also tested, but displayed no synergy in combination with the NSAIDs. The synergistic eVect was concentration dependent. The eVect appears to be independent of the cyclo-oxygenase inhibitory ability of the NSAIDs, as (i) the synergistic combination could not be reversed by the addition of prostaglandins D2 or E2; (ii) sulindac sulphone, a metabolite of sulindac that does not inhibit the cyclooxygenase enzyme, was positive in the combination assay: and (iii) many NSAIDs known to be cyclo-oxygenase inhibitors, e.g. -

Inflammatory Drugs (Nsaids) for People with Or at Risk of COVID-19
Evidence review Acute use of non-steroidal anti- inflammatory drugs (NSAIDs) for people with or at risk of COVID-19 Publication date: April 2020 This evidence review sets out the best available evidence on acute use of non- steroidal anti-inflammatory drugs (NSAIDs) for people with or at risk of COVID-19. It should be read in conjunction with the evidence summary, which gives the key messages. Evidence review commissioned by NHS England Disclaimer The content of this evidence review was up-to-date on 24 March 2020. See summaries of product characteristics (SPCs), British national formulary (BNF) or the MHRA or NICE websites for up-to-date information. For details on the date the searches for evidence were conducted see the search strategy. Copyright © NICE 2020. All rights reserved. Subject to Notice of rights. ISBN: 978-1-4731-3763-9 Contents Contents ...................................................................................................... 1 Background ................................................................................................. 2 Intervention .................................................................................................. 2 Clinical problem ........................................................................................... 3 Objective ...................................................................................................... 3 Methodology ................................................................................................ 4 Summary of included studies -

Formulary Drug Listing Decisions PIROXICAM
March 1, 2010 Formulary Drug Listing Decisions PIROXICAM Indication (s) of chronic arthritis (e.g., osteoarthritis, rheumatoid arthritis and ankylosing Piroxicam is used to treat pain and a spondylitis). This labeling change for variety of inflammatory conditions. piroxicam is relevant for the WSIB population, many of whom are pre- DAC Recommendation scribed NSAIDs for treatment of acute, The Drug Advisory Committee (DAC) has short-term pain. recommended that piroxicam be removed Piroxicam was cited as having an from all WSIB formularies following a increased risk of serious skin reactions Health Canada safety review that cited (e.g., Stevens-Johnson syndrome and piroxicam’s, acute, short-term increased toxic epidermal necrolysis) and gas- risk of serious skin conditions and trointestinal problems relative to other gastrointestinal intestinal (GI) problems NSAIDs. compared to other nonsteroidal anti- Drug Profile inflammatory drugs (NSAIDs). There are a number of equally effective NSAIDs (e.g., ibuprofen, diclofenac) that Products available can be used for treatment of inflamma- in Canada: The WSIB Decision tory conditions, both on an acute and Apo-Piroxicam, Based on the DAC’s recommendations, the chronic basis. Dom-Piroxicam, WSIB has decided to remove piroxicam Gen-Piroxicam, from all formularies at this time. The DAC recommended that piroxicam Novo-Pirox, Nu-Pirox, be removed from WSIB formularies PMS-Piroxicam, Formulary Status based on a Health Canada review of Pro-Piroxicam studies suggesting an increase in GI MANUFACTURER: Variety Piroxicam HAS BEEN REMOVED from toxicity and an increased risk of devel- of generic manufac- WSIB formularies at this time. opment of serious skin reactions (which turers has resulted in labeling changes by Recommendation Highlights Health Canada) and on the availability of Piroxicam is a non-selective NSAID that equally effective NSAIDs for treatment has been used in the treatment of pain of inflammatory conditions. -

Systematic Review Risk of Acute MI with Nsaids in Real
Web Appendix 1 – Systematic review Risk of acute MI with NSAIDs in real-world use: a Bayesian IPD MA Web Table 1: Search strategies for the systematic review of observational studies of NSAIDs and risk of acute MI Individual observational studies PubMed # Keywords 1 (((case-control studies [mh] OR cohort studies [mh] OR cross-over studies [mh] OR epidemiologic studies [mh:noexp] OR cross-sectional studies [mh] OR evaluation studies as topic [mh] OR meta-analysis as topic [mh] OR practice guidelines as topic [mh] OR case control [tw] OR case controlled [tw] OR case controls [tw] OR cohort [tw]OR cohorts [tw] OR follow-up [tw] OR followup [tw] OR longitudinal [tw] OR matched-pair analysis [mh] OR observational studies [tw] OR observational study [tw] OR multicenter study [pt]) AND ((comparative study [pt] OR compare [tw] OR compares [tw] OR compared [tw] OR compared [tw] OR comparing [tw] OR comparison [tw] OR comparative [tw] OR effective [tw] OR effectiveness [tw] OR versus [ti] OR vs [ti]) AND (activities of daily living [mh] OR benefit [tw] OR benefits [tw] OR budgets [mh] OR chronic disease [mh] OR clinical trials data monitoring committees [mh] OR cognitive function [tw] OR ec [sh] OR death [mh] OR diffusion of innovation [mh] OR discharge [tw] OR economics, pharmaceutical [mh] OR evidence based practice [mh] OR functional status [tw] OR guideline adherence [mh] OR harm [tw] OR harms [tw] OR health services research [mh] OR health status [mh] OR hospitalization [mh] OR interventions [tw] OR life expectancy [mh] OR longevity [mh] OR -

Prescription Medications, Drugs, Herbs & Chemicals Associated With
Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus American Tinnitus Association Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form, or by any means, without the prior written permission of the American Tinnitus Association. ©2013 American Tinnitus Association Prescription Medications, Drugs, Herbs & Chemicals Associated with Tinnitus American Tinnitus Association This document is to be utilized as a conversation tool with your health care provider and is by no means a “complete” listing. Anyone reading this list of ototoxic drugs is strongly advised NOT to discontinue taking any prescribed medication without first contacting the prescribing physician. Just because a drug is listed does not mean that you will automatically get tinnitus, or exacerbate exisiting tinnitus, if you take it. A few will, but many will not. Whether or not you eperience tinnitus after taking one of the listed drugs or herbals, or after being exposed to one of the listed chemicals, depends on many factors ‐ such as your own body chemistry, your sensitivity to drugs, the dose you take, or the length of time you take the drug. It is important to note that there may be drugs NOT listed here that could still cause tinnitus. Although this list is one of the most complete listings of drugs associated with tinnitus, no list of this kind can ever be totally complete – therefore use it as a guide and resource, but do not take it as the final word. The drug brand name is italicized and is followed by the generic drug name in bold. -

Nonsteroidal Anti-Inflammatory Drug Use Among Persons with Chronic Kidney Disease in the United States
Nonsteroidal Anti-Infl ammatory Drug Use Among Persons With Chronic Kidney Disease in the United States 1,2 Laura Plantinga, ScM ABSTRACT 1 Vanessa Grubbs, MD PURPOSE Because avoidance of nonsteroidal anti-infl ammatory drugs (NSAIDs) is Urmimala Sarkar, MD1,2 recommended for most individuals with chronic kidney disease (CKD), we sought to characterize patterns of NSAID use among persons with CKD in the United States. Chi-yuan Hsu, MD1 METHODS A total of 12,065 adult (aged 20 years or older) participants in the 3 Elizabeth Hedgeman, MS cross-sectional National Health and Nutrition Examination Survey (1999-2004) Bruce Robinson, MD4 responded to a questionnaire regarding their use of over-the-counter and pre- 3 scription NSAIDs. NSAIDs (excluding aspirin and acetaminophen) were defi ned by Rajiv Saran, MD self-report. CKD was categorized as no CKD, mild CKD (stages 1 and 2; urinary Linda Geiss, MS5 albumin-creatinine ratio of ≥30 mg/g) and moderate to severe CKD (stages 3 and 4; estimated glomerular fi ltration rate of 15-59 mL/min/1.73 m2). Adjusted MPH5 Nilka Ríos Burrows, prevalence was calculated using multivariable logistic regression with appropriate Mark Eberhardt, PhD6 population-based weighting. 1,2 Neil Powe, MD RESULTS Current use (nearly every day for 30 days or longer) of any NSAID was For the CDC CKD Surveillance reported by 2.5%, 2.5%, and 5.0% of the US population with no, mild, and Team moderate to severe CKD, respectively; nearly all of the NSAIDs used were avail- able over-the-counter. Among those with moderate to severe CKD who were 1 Department of Medicine, University of currently using NSAIDs, 10.2% had a current NSAID prescription and 66.1% had California, San Francisco, California used NSAIDs for 1 year or longer.