Mefenamic Acid Induced Autoimmune Hemolytic Anemia- a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

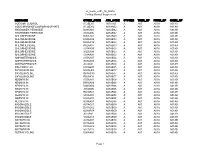
Table S1: Sensitivity, Specificity, PPV, NPV, and F1 Score of NLP Vs. ICD for Identification of Symptoms for (A) Biome Developm
Table S1: Sensitivity, specificity, PPV, NPV, and F1 score of NLP vs. ICD for identification of symptoms for (A) BioMe development cohort; (B) BioMe validation cohort; (C) MIMIC-III; (D) 1 year of notes from patients in BioMe calculated using manual chart review. A) Fatigue Nausea and/or vomiting Anxiety Depression NLP (95% ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P CI) 0.99 (0.93- 0.59 (0.43- <0.00 0.25 (0.12- <0.00 <0.00 0.54 (0.33- Sensitivity 0.99 (0.9 – 1) 0.98 (0.88 -1) 0.3 (0.15-0.5) 0.85 (0.65-96) 0.02 1) 0.73) 1 0.42) 1 1 0.73) 0.57 (0.29- 0.9 (0.68- Specificity 0.89 (0.4-1) 0.75 (0.19-1) 0.68 0.97 (0.77-1) 0.03 0.98 (0.83-1) 0.22 0.81 (0.53-0.9) 0.96 (0.79-1) 0.06 0.82) 0.99) 0.99 (0.92- 0.86 (0.71- 0.94 (0.79- 0.79 (0.59- PPV 0.96 (0.82-1) 0.3 0.95 (0.66-1) 0.02 0.95 (0.66-1) 0.16 0.93 (0.68-1) 0.12 1) 0.95) 0.99) 0.92) 0.13 (0.03- <0.00 0.49 (0.33- <0.00 0.66 (0.48- NPV 0.89 (0.4-1) 0.007 0.94 (0.63-1) 0.34 (0.2-0.51) 0.97 (0.81-1) 0.86 (0.6-0.95) 0.04 0.35) 1 0.65) 1 0.81) <0.00 <0.00 <0.00 F1 Score 0.99 0.83 0.88 0.57 0.95 0.63 0.82 0.79 0.002 1 1 1 Itching Cramp Pain NLP (95% ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P CI) 0.98 (0.86- 0.24 (0.09- <0.00 0.09 (0.01- <0.00 0.52 (0.37- <0.00 Sensitivity 0.98 (0.85-1) 0.99 (0.93-1) 1) 0.45) 1 0.29) 1 0.66) 1 0.89 (0.72- 0.5 (0.37- Specificity 0.96 (0.8-1) 0.98 (0.86-1) 0.68 0.98 (0.88-1) 0.18 0.5 (0-1) 1 0.98) 0.66) 0.88 (0.69- PPV 0.96 (0.8-1) 0.8 (0.54-1) 0.32 0.8 (0.16-1) 0.22 0.99 (0.93-1) 0.98 (0.87-1) NA* 0.97) 0.98 (0.85- 0.57 (0.41- <0.00 0.58 (0.43- <0.00 NPV 0.98 (0.86-1) 0.5 (0-1) 0.02 (0-0.08) NA* 1) 0.72) 1 0.72) 1 <0.00 <0.00 <0.00 F1 Score 0.97 0.56 0.91 0.28 0.99 0.68 1 1 1 *Denotes 95% confidence intervals and P values that could not be calculated due to insufficient cells in 2x2 tables. -

Health Reports for Mutual Recognition of Medical Prescriptions: State of Play
The information and views set out in this report are those of the author(s) and do not necessarily reflect the official opinion of the European Union. Neither the European Union institutions and bodies nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein. Executive Agency for Health and Consumers Health Reports for Mutual Recognition of Medical Prescriptions: State of Play 24 January 2012 Final Report Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Acknowledgements Matrix Insight Ltd would like to thank everyone who has contributed to this research. We are especially grateful to the following institutions for their support throughout the study: the Pharmaceutical Group of the European Union (PGEU) including their national member associations in Denmark, France, Germany, Greece, the Netherlands, Poland and the United Kingdom; the European Medical Association (EMANET); the Observatoire Social Européen (OSE); and The Netherlands Institute for Health Service Research (NIVEL). For questions about the report, please contact Dr Gabriele Birnberg ([email protected] ). Matrix Insight | 24 January 2012 2 Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Executive Summary This study has been carried out in the context of Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross- border healthcare (CBHC). The CBHC Directive stipulates that the European Commission shall adopt measures to facilitate the recognition of prescriptions issued in another Member State (Article 11). At the time of submission of this report, the European Commission was preparing an impact assessment with regards to these measures, designed to help implement Article 11. -

United States Patent 19 11 Patent Number: 5,366,505 Farber 45 Date of Patent: Nov
O USOO5366505A United States Patent 19 11 Patent Number: 5,366,505 Farber 45 Date of Patent: Nov. 22, 1994 54 METHOD OF REDUCING MEDICAL 4,886,505 12/1989 Haynes et al. ...................... 604/265 DEVICE RELATED INFECTIONS 4,925,668 5/1990 Khan et al. ......................... 424/422 75 Inventor: Bruce Farber, Port Washington, OTHER PUBLICATIONS N.Y. D. G. Maki et al., Clinical Trial of a Novel Antiseptic 73 Assignee: North Shore University Hospital Central Venous Catheter, Abstracts of the 1991 Inter Research Corporation, Manhasset, science Conference on Antimicrobial Agents and Che N.Y. motherapy, p. 176 (1991). C. J. Stephens et al. Randomized Double-Blind Trial 21 Appl. No.: 35,553 Comparing the Risk of Peripheral Vein Thrombophle 22 Filed: Mar. 23, 1993 bitis (T) Between Chlorhexidine (CHA) Coated Cathe ters (C) with Uncoated Control, Abstracts of the 1991 Related U.S. Application Data Interscience Conference on Antimicrobial Agents and Chemotherapy, p. 277 (1991). 63)63 Continuation-in-Tian in-part off Ser. NoNo. 802,891, Dec.ec 6, 1991, M. Tojo et al., Isolation and Characterization of a Cap 5 sular Polysaccharide Adhesin from Staphylococcus epi 51) Int. Cli................................................ A61F 2/02 dermidis, J. Infect. Dis. 157(4): 713-722 (1987). 52 U.S. C. ....................................... 623/11; 604/265 58) Field of Search ........................ 428/413:523/112, Primary Examiner-David Isabella 623/11, 12, 1, 2; 427/2, 604/265 Attorney, Agent, or Firm-Kenyon & Kenyon 56 References Cited 57 ABSTRACT U.S. PATENT DOCUMENTS The growth of microorganisms on catheters and other 4,581,028 4/1986 Fox, Jr. -

The Challenge of Drug-Induced Aseptic Meningitis Revisited
Letters cardioverter-defibrillator generator replacements and upgrade procedures: brospinal fluid (CSF) findings and reviews added to the litera- results from the REPLACE registry. Circulation. 2010;122(16):1553-1561. ture from 1999 to date. Tables have been assembled from 6. Kramer DB, Buxton AE, Zimetbaum PJ. Time for a change: a new approach to information derived from 192 studies (these data are avail- ICD replacement. N Engl J Med. 2012;366(4):291-293. able from the authors on request). The Challenge of Drug-Induced Aseptic Results | Four groups of drugs continue to be associated Meningitis Revisited with DIAM (Table 1): nonsteroidal anti-inflammatory Cases of drug-induced aseptic meningitis (DIAM) are likely drugs (NSAIDs), antibiotics, immunosuppressive- underreported, and only a few reviews of the literature have immunomodulatory (IS-IM), and antiepileptic drugs.1 Prior been performed. We have updated (to February 2014) a pre- exposure to the associated drug was present in 26% to 35% vious review (1999)1 to identify newer agents associated with of cases (Table 1). The interval between exposure and men- DIAM, as well as distinctive new features. ingitis ranged from minutes to 5 months (Table 1). Most patients presented with headache, fever, meningismus, and Methods | Using the MEDLINE database, we searched the lit- mental status changes (Table 2). Underlying systemic disor- erature to February 2014 and included those cases with cere- ders were often present, particularly systemic lupus ery- Table 1. Drugs Involved in Drug-Induced -

DAYPRO ALTA™ (Oxaprozin Potassium) 600Mg Tablets Cardiovascular Risk • Nsaids May Cause an Increased Risk of Serious Cardiov
DAYPRO ALTA™ (oxaprozin potassium) 600mg tablets Cardiovascular Risk NSAIDs may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patient’s with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk (see WARNINGS). Daypro ALTA is contraindicated for treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery (see WARNINGS). Gastrointestinal Risk NSAID’s cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events (see WARNINGS). DESCRIPTION DAYPRO ALTA (oxaprozin potassium tablets) is a member of the propionic acid group of nonsteroidal anti-inflammatory drugs (NSAIDs). Each blue, capsule-shaped tablet contains oxaprozin potassium (678mg equivalent to 600mg of oxaprozin) for oral administration. The chemical name for oxaprozin potassium is 4,5-diphenyl-2-oxazolepropionic acid, potassium salt. Its empirical formula is C18H14NO3K, and molecular weight is 331. Oxaprozin potassium is a white to off white powder with a melting point of 215°C. It is slightly soluble in alcohol and very soluble in water. The PK in water is 9.7. It has the following structural formula: Inactive ingredients in DAYPRO ALTA tablets include microcrystalline cellulose, hydroxypropyl methylcellulose, pregelatinized corn starch, stearic acid, colloidal silicon dioxide, polyethylene glycol, titanium dioxide, FD&C Blue #1 Aluminum Lake, and pharmaceutical glaze. -

Fentiazac (BAN, USAN, Rinn) Preparations Mate Aluminium); 16449-54-0 (Flufenamate Aluminium)
60 Analgesics Anti-inflammatory Drugs and Antipyretics sia after caesarean section confirmed an additive analgesic effect Fepradinol (rINN) Floctafenine (BAN, USAN, rINN) for the combination, there was no demonstrable clinical benefit ± α Floctafenina; Floctafénine; Floctafeninum; R-4318; RU-15750. compared with fentanyl alone in this patient group who expect Fépradinol; Fepradinolum. ( )- -{[(2-Hydroxy-1,1-dimethyle- N early mobilisation. However, the combination may be of greater thyl)amino]methyl}benzyl alcohol. 2,3-Dihydroxypropyl -(8-trifluoromethyl-4-quinolyl)anthrani- benefit in patients for whom early ambulation is not routine. Фепрадинол late. Флоктафенин Fentanyl has also been given by epidural injection to children for C12H19NO2 = 209.3. 7 postoperative analgesia. CAS — 63075-47-8. C20H17F3N2O4 = 406.4. Fentanyl has been tried by intrathecal injection for postoperative CAS — 23779-99-9. pain.8 ATC — N02BG04. As mentioned in Administration, Transdermal Route, above, an OH ATC Vet — QN02BG04. iontophoretic transdermal system for postoperative pain is also available.9-11 CH 3 OH 1. Mitchell RWD, Smith G. The control of acute postoperative N pain. Br J Anaesth 1989; 63: 147–58. HO O O 2. Morgan M. The rational use of intrathecal and extradural opio- H CH3 ids. Br J Anaesth 1989; 63: 165–88. OH H 3. Grass JA, et al. A randomized, double-blind, dose-response comparison of epidural fentanyl versus sufentanil analgesia af- N ter cesarean section. Anesth Analg 1997; 85: 365–71. Profile CF3 4. Swarm RA, et al. Pain treatment in the perioperative period. Fepradinol is an NSAID (p.96) that has been used topically in a N Curr Probl Surg 2001; 38: 835–920. -

Original Paper Enhancement of Chemotherapeutic Drug Toxicity To
European Journal of Cancer, Vol. 34, No. 8, pp. 1250±1259, 1998 # 1998 Elsevier Science Ltd. All rights reserved Pergamon Printed in Great Britain 0959-8049/98 $19.00+0.00 PII: S0959-8049(98)00045-8 Original Paper Enhancement of Chemotherapeutic Drug Toxicity to Human Tumour Cells In Vitro by a Subset of Non-steroidal Anti-in¯ammatory Drugs (NSAIDs) C.P. DuVy, C.J. Elliott, R.A. O'Connor, M.M. Heenan, S. Coyle, I.M. Cleary, K. Kavanagh, S. Verhaegen, C.M. O'Loughlin, R. NicAmhlaoibh and M. Clynes National Cell and Tissue Culture Centre, Dublin City University, Glasnevin, Dublin 9, Ireland The eVect on cytotoxicity of combining a range of clinically important non-steroidal anti-in¯amma- tory drugs (NSAIDs) with a variety of chemotherapeutic drugs was examined in the human lung cancer cell lines DLKP, A549, COR L23P and COR L23R and in a human leukaemia line HL60/ADR. A speci®c group of NSAIDs (indomethacin, sulindac, tolmetin, acemetacin, zomepirac and mefenamic acid) all at non-toxic levels, signi®cantly increased the cytotoxicity of the anthracyclines (doxorubicin, daunorubicin and epirubicin), as well as teniposide, VP-16 and vincristine, but not the other vinca alkaloids vinblastine and vinorelbine. Asubstantial number of other anticancer drugs, including methotrexate, 5-¯uorouracil, cytarabine, hydroxyurea, chlorambucil, cyclophosphamide, cisplatin, carboplatin, mitoxantrone, actinomycin D, bleomycin, paclitaxel and camptothecin, were also tested, but displayed no synergy in combination with the NSAIDs. The synergistic eVect was concentration dependent. The eVect appears to be independent of the cyclo-oxygenase inhibitory ability of the NSAIDs, as (i) the synergistic combination could not be reversed by the addition of prostaglandins D2 or E2; (ii) sulindac sulphone, a metabolite of sulindac that does not inhibit the cyclooxygenase enzyme, was positive in the combination assay: and (iii) many NSAIDs known to be cyclo-oxygenase inhibitors, e.g. -
Vr Meds Ex01 3B 0825S Coding Manual Supplement Page 1
vr_meds_ex01_3b_0825s Coding Manual Supplement MEDNAME OTHER_CODE ATC_CODE SYSTEM THER_GP PHRM_GP CHEM_GP SODIUM FLUORIDE A12CD01 A01AA01 A A01 A01A A01AA SODIUM MONOFLUOROPHOSPHATE A12CD02 A01AA02 A A01 A01A A01AA HYDROGEN PEROXIDE D08AX01 A01AB02 A A01 A01A A01AB HYDROGEN PEROXIDE S02AA06 A01AB02 A A01 A01A A01AB CHLORHEXIDINE B05CA02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D08AC02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D09AA12 A01AB03 A A01 A01A A01AB CHLORHEXIDINE R02AA05 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S01AX09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S02AA09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S03AA04 A01AB03 A A01 A01A A01AB AMPHOTERICIN B A07AA07 A01AB04 A A01 A01A A01AB AMPHOTERICIN B G01AA03 A01AB04 A A01 A01A A01AB AMPHOTERICIN B J02AA01 A01AB04 A A01 A01A A01AB POLYNOXYLIN D01AE05 A01AB05 A A01 A01A A01AB OXYQUINOLINE D08AH03 A01AB07 A A01 A01A A01AB OXYQUINOLINE G01AC30 A01AB07 A A01 A01A A01AB OXYQUINOLINE R02AA14 A01AB07 A A01 A01A A01AB NEOMYCIN A07AA01 A01AB08 A A01 A01A A01AB NEOMYCIN B05CA09 A01AB08 A A01 A01A A01AB NEOMYCIN D06AX04 A01AB08 A A01 A01A A01AB NEOMYCIN J01GB05 A01AB08 A A01 A01A A01AB NEOMYCIN R02AB01 A01AB08 A A01 A01A A01AB NEOMYCIN S01AA03 A01AB08 A A01 A01A A01AB NEOMYCIN S02AA07 A01AB08 A A01 A01A A01AB NEOMYCIN S03AA01 A01AB08 A A01 A01A A01AB MICONAZOLE A07AC01 A01AB09 A A01 A01A A01AB MICONAZOLE D01AC02 A01AB09 A A01 A01A A01AB MICONAZOLE G01AF04 A01AB09 A A01 A01A A01AB MICONAZOLE J02AB01 A01AB09 A A01 A01A A01AB MICONAZOLE S02AA13 A01AB09 A A01 A01A A01AB NATAMYCIN A07AA03 A01AB10 A A01 -

Søgeprotokol for Nationale Kliniske Retningslinjer
Søgeprotokol for nationale kliniske retningslinjer Projekttitel/aspekt NKR behandling af patienter med lumbal spinalstenose – Søgning efter primærlitteratur Fagkonsulent /projektleder Rikke Rousing / Maria Herlev Ahrenfeldt Søgespecialist Kirsten Birkefoss Senest opdateret 23.12.2016 Fokuserede spørgsmål Bør patienter med lumbal spinalstenose have tilbudt aktiv PICO 1: behandling i form af superviseret træning fremfor vanlig behandling? PICO 2: Bør patienter med lumbal spinalstenose have tilbudt ledmobiliserende behandling frem for vanlig behandling? PICO 3: Bør patienter med lumbal spinalstenose have tilbudt paracetamol frem for ingen smertestillende behandling? PICO 4: Bør patienter med lumbal spinalstenose have tilbudt non steroid antiinflammatorisk medicin (NSAID) frem for ingen smertestillende behandling? PICO 5: Bør patienter med lumbal spinalstenose have tilbudt smertestillende medicin i form af opioider i tillæg til eventuel behandling med svage smertestillende? PICO 6: Bør patienter med lumbal spinalstenose have tilbudt muskelrelaxantia i tillæg til eventuel behandling med svage smertestillende? PICO 7: Bør patienter med lumbaspinalstenose have tilbudt medicin for neuropatiske smerter? PICO 8: Bør patienter med lumbal spinalstenose have tilbudt kirurgisk dekompression i tilfælde af manglende effekt af ikke kirurgisk behandling? PICO 9: Bør patienter med lumbal spinalstenose have tilbudt stivgørende operation med eller uden instrumentering i tillæg til dekompression? PICO 10: Bør patienter opereret for lumbal spinalstenose tilbydes -

Formulary Drug Listing Decisions PIROXICAM
March 1, 2010 Formulary Drug Listing Decisions PIROXICAM Indication (s) of chronic arthritis (e.g., osteoarthritis, rheumatoid arthritis and ankylosing Piroxicam is used to treat pain and a spondylitis). This labeling change for variety of inflammatory conditions. piroxicam is relevant for the WSIB population, many of whom are pre- DAC Recommendation scribed NSAIDs for treatment of acute, The Drug Advisory Committee (DAC) has short-term pain. recommended that piroxicam be removed Piroxicam was cited as having an from all WSIB formularies following a increased risk of serious skin reactions Health Canada safety review that cited (e.g., Stevens-Johnson syndrome and piroxicam’s, acute, short-term increased toxic epidermal necrolysis) and gas- risk of serious skin conditions and trointestinal problems relative to other gastrointestinal intestinal (GI) problems NSAIDs. compared to other nonsteroidal anti- Drug Profile inflammatory drugs (NSAIDs). There are a number of equally effective NSAIDs (e.g., ibuprofen, diclofenac) that Products available can be used for treatment of inflamma- in Canada: The WSIB Decision tory conditions, both on an acute and Apo-Piroxicam, Based on the DAC’s recommendations, the chronic basis. Dom-Piroxicam, WSIB has decided to remove piroxicam Gen-Piroxicam, from all formularies at this time. The DAC recommended that piroxicam Novo-Pirox, Nu-Pirox, be removed from WSIB formularies PMS-Piroxicam, Formulary Status based on a Health Canada review of Pro-Piroxicam studies suggesting an increase in GI MANUFACTURER: Variety Piroxicam HAS BEEN REMOVED from toxicity and an increased risk of devel- of generic manufac- WSIB formularies at this time. opment of serious skin reactions (which turers has resulted in labeling changes by Recommendation Highlights Health Canada) and on the availability of Piroxicam is a non-selective NSAID that equally effective NSAIDs for treatment has been used in the treatment of pain of inflammatory conditions. -

United States Patent (19) 11 Patent Number: 5,192,753 Mcgeer Et Al
USOO5192753A United States Patent (19) 11 Patent Number: 5,192,753 McGeer et al. 45 Date of Patent: Mar. 9, 1993 54 ANTI-RHEUMATOID ARTHRITIC DRUGS mentia: Prevalance and Incidence', In: B. Reisberg (ed) N THE TREATMENT OF DEMENTIA Alzheimer's Disease, The Free Press, 1983, 141-148. 76 Inventors: Patrick L. McGeer, 4727 West 2nd R. Sulkava, J. Wikstrom, A. Aromaa et al., "Prevalence Ave., Vancouver, B. C., Canada, of Severe Dementia in Finland’, Neurology 1985; 35: V6T Cl; Joseph Rogers, 7646 W. 1025-1029. Julie Dr., Glendale, Ariz. 85308; S. Itagaki, P. L. McGeer, H. Akiyama, "Presence of John Sibley, 87 Leddy Crescent, T-cytotoxic Suppressor and Leucocyte Common Anti Saskatoon, Saskatchewan, Canada, gen Positive Cells in Alzheimer's Disease Brain Tissue", S7H 3Y9; Edith McGeer, 4727 West Neuroscience Letters 1988; 91: 259-264. 2nd Ave., Vancouver, B.C., Canada, J. Rogers, J. Luber-Narod, S. D. Styren, and W. H. V6T 1C Civin, "Expression of Immune System-Associated An tigens By Cells of the Human Central Nervous System: (21) Appl. No.: 689,499 Relationship to the Pathology of Alzheimer's Disease" (22 Filed: Apr. 23, 1991 Neurobiology of Aging, 1988, vol. 9. 339-349. 51 Int. Cl. ................... A61K 31/60; A61K 31/615; P. L. McGeer, H. Akiyama, S. Itagaki, and E. G. A61K 31/54; A61K 31/44; A61K 3/425; McGeer, "Immune System Response in Alzheimer's A61K 31/42; A61K 31/415, A61K 31/40; Disease', The Canadian Journal of Neurological Sci A61K 31/38; A61K 31/195; A61K 31/19 ences 1989; 16:56-527. -

Nonsteroidal Anti-Inflammatory Drug Use Among Persons with Chronic Kidney Disease in the United States
Nonsteroidal Anti-Infl ammatory Drug Use Among Persons With Chronic Kidney Disease in the United States 1,2 Laura Plantinga, ScM ABSTRACT 1 Vanessa Grubbs, MD PURPOSE Because avoidance of nonsteroidal anti-infl ammatory drugs (NSAIDs) is Urmimala Sarkar, MD1,2 recommended for most individuals with chronic kidney disease (CKD), we sought to characterize patterns of NSAID use among persons with CKD in the United States. Chi-yuan Hsu, MD1 METHODS A total of 12,065 adult (aged 20 years or older) participants in the 3 Elizabeth Hedgeman, MS cross-sectional National Health and Nutrition Examination Survey (1999-2004) Bruce Robinson, MD4 responded to a questionnaire regarding their use of over-the-counter and pre- 3 scription NSAIDs. NSAIDs (excluding aspirin and acetaminophen) were defi ned by Rajiv Saran, MD self-report. CKD was categorized as no CKD, mild CKD (stages 1 and 2; urinary Linda Geiss, MS5 albumin-creatinine ratio of ≥30 mg/g) and moderate to severe CKD (stages 3 and 4; estimated glomerular fi ltration rate of 15-59 mL/min/1.73 m2). Adjusted MPH5 Nilka Ríos Burrows, prevalence was calculated using multivariable logistic regression with appropriate Mark Eberhardt, PhD6 population-based weighting. 1,2 Neil Powe, MD RESULTS Current use (nearly every day for 30 days or longer) of any NSAID was For the CDC CKD Surveillance reported by 2.5%, 2.5%, and 5.0% of the US population with no, mild, and Team moderate to severe CKD, respectively; nearly all of the NSAIDs used were avail- able over-the-counter. Among those with moderate to severe CKD who were 1 Department of Medicine, University of currently using NSAIDs, 10.2% had a current NSAID prescription and 66.1% had California, San Francisco, California used NSAIDs for 1 year or longer.