How 'Masterchef'
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Awards + Accolades
AWARDS + ACCOLADES *** James Beard Foundation Awards Michelin 2015 Outstanding Pastry Chef – Christina Tosi 2009, 2010, 2011, 2012, 2013, 2014, 2015, 2016 2 Stars – Ko 2014 Who's Who of Food and Beverage – David Chang 2014 MFK Fisher Distinguished Writing Award Michelin Bib Gourmand “I Placed a Jar in Tennessee,” Lucky Peach, Issue 7 2009, 2010, 2011, 2012, 2013, 2014, 2015, 2016 Ssäm Bar 2014 Profile – "A Day on Long Island with Alex Lee,” 2008, 2009, 2010, 2011, 2012, 2013, 2014, 2015, 2016 Noodle Bar Lucky Peach, Issue 9 2014 Humor – “On the Trail with Wylie,” Lucky Peach, Issue 9 The Sydney Morning Herald Good Food Guide 2014 Personal Essay – “Dick Soup,” Lucky Peach, Issue 8 (2013, 2014, 2015) 2016 Two Hats – Seiōbo 2014 Food and Culture – "America, Your Food Is So Gay,” 2015 Best Bar Restaurant– Seiōbo Lucky Peach, Issue 7 2014 Sommelier of the Year – Richard Hargreave 2013 Outstanding Chef – David Chang 2013 Best New Restaurant – Seiōbo 2013 Personal Essay – "London Town," Lucky Peach, Issue 5 2012 Chef of the Year Nomination – Ben Greeno 2013 TV Program On Location – The Mind of a Chef 2012 Rising Star Chef of the Year – Christina Tosi The Australian 2012 Outstanding Chef Nomination – David Chang 2012 Hottest Restaurant of the Year – Seiōbo 2010 Cookbook Nomination – Momofuku 2009 Best New Restaurant – Ko Gourmet Traveller 2008 Best Chef, New York City – David Chang 2015 3 out of 3 stars - Seiōbo 2007 Best New Restaurant Nomination – Ssäm Bar 2014 Restaurant of the Year – Seiōbo 2007 Rising Star Chef of the Year – David Chang -

21St Annual Restaurant Industry Conference
21ST ANNUAL RESTAURANT INDUSTRY CONFERENCE WEDNESDAY, MAY 3, 2017, COVEL COMMONS, UCLA WELCOME UCLA Extension is proud to present the 22nd Annual Restaurant Industry Conference, with this year’s focus on Dining Disrupted! The “digital tsunami” is powerful and unrelenting, posing life-changing challenges, opportunities, and seeming to require immediate responsiveness. It’s no secret that many established restaurants and suppliers are not only facing economic volatility but are continuously challenged by more informed and demanding diners. This year we honor Robert Brozin, who built Nando’s Roger Torneden from one restaurant to a truly world-wide brand serving millions of diners. As chief executive of Nando’s until Associate Dean, Executive Director of UCLA Online 2010, he used sheer creativity (and Portuguese- Director, Department of Business, Management style peri-peri sauce) to take a little restaurant from & Legal Programs, UCLA Extension Rosettenville, South Africa, to the world. Today, Nando’s is loved in America, Australia, the United Kingdom, and 20 other countries as diverse as Fiji and Bangladesh. UCLA Extension serves approximately 40,000 students annually through Westwood, Downtown Los Angeles, and Woodland Hills campuses, plus a substantial selection of online courses. Our students typically already have degrees and years of experience but are seeking enhanced or new careers. Our instructors are “best in class” practitioners approved by UCLA’s campus schools for academic and teaching qualifications. In the Business, Management & Legal Programs Department, we focus on certificate programs and courses across industries (e.g., web analytics and social media marketing, small business management, credit analysis, finance, accounting, etc.) and on specific industries (hospitality, financial services, consulting, security, real estate, etc.). -

MISSISSIPPI LEGISLATURE REGULAR SESSION 2011 By
MISSISSIPPI LEGISLATURE REGULAR SESSION 2011 By: Representatives Frierson, Formby To: Rules HOUSE RESOLUTION NO. 40 1 A RESOLUTION COMMENDING AND CONGRATULATING MISS WHITNEY 2 MILLER OF POPLARVILLE, MISSISSIPPI, FOR WINNING THE TITLE OF 3 "MASTERCHEF" IN SEASON ONE OF FOX TELEVISION NETWORK'S REALITY 4 COOKING COMPETITION SERIES "MASTERCHEF." 5 WHEREAS, on September 15, 2010, University of Southern 6 Mississippi senior, Whitney Miller, was crowned "MasterChef" of 7 FOX Television's first season of "MasterChef," a reality cooking 8 competition series hosted by celebrity Chef Gordon Ramsay; and 9 WHEREAS, she auditioned for the show in New Orleans, 10 Louisiana, and was one of 50 top chefs selected from around the 11 nation; and 12 WHEREAS, in the competition's finale, this 22-year-old 13 college student prevailed against a 29-year-old software engineer 14 from Boston, capturing the title of "MasterChef," $250,000.00 in 15 prize money and a contract to publish her own cookbook; and 16 WHEREAS, her winning meal included an appetizer of sweet 17 shrimp on a crispy corn cake, a main course of fried chicken with 18 creamed collard greens, and a dessert of bread pudding with 19 raspberry coulis and white chocolate sauce; and 20 WHEREAS, the second of three children born to Mary and John 21 Miller of Poplarville, Mississippi, Whitney developed her passion 22 and love for food at a young age by creating delicious meals with 23 her mother; and 24 WHEREAS, coined the "Pastry Princess" by the judges, her 25 giggly cute-as-could-be exterior concealed a steely 26 self-confidence that propelled this nutrition and biology major to 27 become a culinary champion; and H. -

A Cultural Study of Gendered Onscreen
VEG-GENDERED: A CULTURAL STUDY OF GENDERED ONSCREEN REPRESENTATIONS OF FOOD AND THEIR IMPLICATIONS FOR VEGANISM by Paulina Aguilera A Thesis Submitted to the Faculty of The Dorothy F. Schmidt College of Arts & Letters In Partial Fulfillment of the Requirements for the Degree of Master of Arts Florida Atlantic University Boca Raton, FL August 2014 Copyright by Paulina Aguilera, 2014 11 VEG-GENDERED: A STUDY OF GENDERED ONSCREEN REPRESENTATIONS OF FOOD AND THEIR IMPLICATIONS FOR VEGANISM by Paulina Aguilera This thesis was prepared under the direction of the candidate's thesis advisor, Dr. Christine Scodari, School of Communication and Multimedia Studies, and has been approved by the members of her supervisory committee. It was submitted to the faculty of The Dorothy F. Schmidt College of Arts and Letters and was accepted in partial fulfillment of the requirements for the degree of Master of Arts. SUPERVISORY COMMITTEE: ~t~;,~ obe, Ph.D. David C. Williams, Ph.D. Interim Director, School of Communication and Multimedia Studies Heather Coltman, DMA Dean, ;~~of;candLetters 0'7/0 /:fdf4 8 ~T.Fioyd, Ed.D~ -D-at_e _ _,__ ______ Interim Dean, Graduate College 111 ACKNOWLEDGEMENTS The author wishes to acknowledge Dr. Christi ne Scodari for her incredible guidance and immeasurable patience during the research and writing of this thesis. Acknowledgements are also in order to the participating committee members, Dr. Chris Robe and Dr. Fred Fejes, who provided further feedback and direction. Lastly, a special acknowledgement to Chandra Holst-Maldonado is necessary for her being an amazing source of moral support throughout the thesis process. -

The Walking Dead,” Which Starts Its Final We Are Covid-19 Safe-Practice Compliant Season Sunday on AMC
Las Cruces Transportation August 20 - 26, 2021 YOUR RIDE. YOUR WAY. Las Cruces Shuttle – Taxi Charter – Courier Veteran Owned and Operated Since 1985. Jeffrey Dean Morgan Call us to make is among the stars of a reservation today! “The Walking Dead,” which starts its final We are Covid-19 Safe-Practice Compliant season Sunday on AMC. Call us at 800-288-1784 or for more details 2 x 5.5” ad visit www.lascrucesshuttle.com PHARMACY Providing local, full-service pharmacy needs for all types of facilities. • Assisted Living • Hospice • Long-term care • DD Waiver • Skilled Nursing and more Life for ‘The Walking Dead’ is Call us today! 575-288-1412 Ask your provider if they utilize the many benefits of XR Innovations, such as: Blister or multi-dose packaging, OTC’s & FREE Delivery. almost up as Season 11 starts Learn more about what we do at www.rxinnovationslc.net2 x 4” ad 2 Your Bulletin TV & Entertainment pullout section August 20 - 26, 2021 What’s Available NOW On “Movie: We Broke Up” “Movie: The Virtuoso” “Movie: Vacation Friends” “Movie: Four Good Days” From director Jeff Rosenberg (“Hacks,” Anson Mount (“Hell on Wheels”) heads a From director Clay Tarver (“Silicon Glenn Close reunited with her “Albert “Relative Obscurity”) comes this 2021 talented cast in this 2021 actioner that casts Valley”) comes this comedy movie about Nobbs” director Rodrigo Garcia for this comedy about Lori and Doug (Aya Cash, him as a professional assassin who grapples a straight-laced couple who let loose on a 2020 drama that casts her as Deb, a mother “You’re the Worst,” and William Jackson with his conscience and an assortment of week of uninhibited fun and debauchery who must help her addict daughter Molly Harper, “The Good Place”), who break up enemies as he tries to complete his latest after befriending a thrill-seeking couple (Mila Kunis, “Black Swan”) through four days before her sister’s wedding but decide job. -
Haley Messner 619-312-1212 [email protected]
Haley Messner 619-312-1212 [email protected] FOR IMMEDIATE RELEASE GRAHAM ELLIOT INVITES YOU TO TAKE A BITE OF SOMETHING AWESOME AT THE 15TH ANNUAL SAN DIEGO BAY WINE + FOOD FESTIVAL® Celebrity Chefs, Winemakers, And Tastemakers To Host Epic Festival of Food, Wine and Culture, November 11-18, 2018 San Diego, CA (October 24, 2018) – Travel to San Diego. Arrive at Awesome. As one of the country’s most talked about weeks in food and wine, the San Diego Bay Wine + Food Festival® announces an impressive lineup of celebrity chefs, winemakers, and artisans for its 15th annual festival held November 11-18, 2018. This year’s talent lineup includes, nationally recognized celebrity chefs, legendary winemakers, guest mixologists, James Beard Award-winning authors, Master Sommeliers, brewmasters, artisans and tastemakers, such as: Graham Elliot, Television Personality and Author; Alex Thomopoulos, Chef, Host and Food Blogger; Duskie Estes of Zazu Kitchen + Farm; Michael Ruhlman, American Author and Cook; Abraham Conlon, of Fat Rice; Michael Schlow, of Schlow Restaurant Group; the Hearty Boys television personalities, Dan Smith and Steve McDonagh; Stephanie Prida of The Pool; Dean James Max of DJM Restaurants; Katsuya Fukushima of Daikaya; Javier Plascencia of Jazamango, Mision 19, Erizo, Finca Altozano, Caffe Saverios, and ¡Lupe!; Domenica Catelli of Catelli’s; Laura Werlin, Author of The All American Cheese and Wine Book; Suzette Gresham of Acquerello; Gale Gand, acclaimed pastry chef; Flor Franco of Encuentro Guadalupe, Convivia, Resguardo; Travis Swikard formerly of Boulud Sud, Bar Boulud, and Epicerie Boulud; Matt Zubrod of The Little Nell; Chad White of Zona Blanca; and more. -

Board of Zoning Appeal for the City of Cambridge
1 BOARD OF ZONING APPEAL FOR THE CITY OF CAMBRIDGE GENERAL HEARING THURSDAY, SEPTEMBER 28, 2017 7:00 p.m. in Senior Center 806 Massachusetts Avenue First Floor Cambridge, Massachusetts 02139 Constantine Alexander, Chair Brendan Sullivan, Vice Chair Janet Green, Member Andrea A. Hickey, Member Patrick Tedesco, Member Slater W. Anderson, Associate Member Sean O'Grady, Zoning Specialist ____________________________ REPORTERS, INC. CAPTURING THE OFFICIAL RECORD 617.786.7783/617.639.0396 (Fax) www.reportersinc.com I N D E X CASE PAGE 2 BZA-013691-2017 -- 346 Washington Street Original Hearing Date: 07/27/17 7 BZA-013611-2017 -- 35-37 Berkshire Street Original Hearing Date: 07/13/17 295 BZA-013730-2017 -- 8 Brattle Street Original Hearing Date: 08/1017 12 BZA-014160-2017 -- 1160 Massachusetts Avenue 320 BZA-014181-2017 -- 81 Kirkland Street #2 279 BZA-014217-2017 -- 144-146 Raymond Street 335 BZA-014237-2017 -- 156 Line Street 342 KeyWordIndex 3 P R O C E E D I N G S * * * * * (7:00 p.m.) (Sitting Members: Constantine Alexander, Brendan Sullivan, Janet Green, Andrea A. Hickey, Patrick Tedesco.) CONSTANTINE ALEXANDER: The Chair will call this meeting of the Zoning Board of Appeals to order. As is our custom, we will start with continued cases. These are cases that started at an earlier night and for one reason or another have been continued until tonight. And then we'll turn to our regular agenda. Before I start the meeting, I'd like to read a statement: After notifying the Chair, any person may make a video or audio recording of our open sessions or may transmit the meeting through any medium subject to reasonable requirements that the Chair may impose -- UNIDENTIFIED MEMBER FROM THE AUDIENCE: Microphone? CONSTANTINE ALEXANDER: Sorry? 4 JANET GREEN: Microphone. -
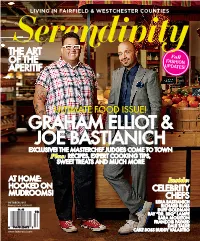
Graham Elliot & Joe Bastianich
LIVING IN FAIRFIELD & WESTCHESTER COUNTIES Serendipity THE ART Fall OF THE FASHION APERITIF UPDATES! ULTIMATE FOOD ISSUE! GRAHAM ELLIOT & JOE BASTIANICH EXCLUSIVE! THE MASTERCHEF JUDGES COME TO TOWN Plus: RECIPES, EXPERT COOKING TIPS, SWEET TREATS AND MUCH MORE AT HOME: Inside: HOOKED ON CELEBRITY MUDROOMS! CHEFS OCTOBER 2013 LIDIA BASTIANICH Display Until 11/4/2013 RICHARD BLAIS DUFF GOLDMAN RAY “DR. BBQ” LAMPE SARA MOULTON FRANÇOIS PAYARD DALE TALDE serendipitysocial.com CAKE BOSS BUDDY VALASTRO FOODIES A P S AUTY E B ROVA, ROVA, E LON & Z I What a pear! Elliot, left, and Bastianich, A S M GRAHAM ELLIOT AND JOE BASTIANICH ARE MORE THAN CO-JUDGES right, were photographed by Serendipity NA A friends ON FOX’s MASTERCHEF, THE TWO CULINARY GREATS ARE ALSO on August 30 at Tarry Market (co-owned LAND Z O by Bastianich and Mario Batali) in N GREAT FRIENDS. ON AIR, THEIR DEMEANORS DIFFer — Joe is Port Chester, NY. In between takes, the guys, who are both musicians, had a THE SERIOUS ONE, GRAHAM IS THE EVERyman — but oFF CAMERA, great time looking through the market’s AND AT SERENDIPITY’s 2013 GREENWICH WINE+FOOD FESTIVAL, collection of rock ’n’ roll LPs. GROOMING BY ZU CHRISTOPHER THEIR CHEMISTRY IS DELICIOUSLY FUN. PHOTOGRAPHS BY STEVE GIRALT 100 OCTOBER 2013 Elliot, right, with a MasterChef contestant and Joe Bastianich. ELLIOT BECAME THE grahamYOUNGEST FOUR-STAR CHEF IN THE COUNTRY AT AGE 27. NINE We’ve all goTTEN ALONG FROM DAY ONE. YEARS LATER, THE MUSICIAN, HUSBAND AND FATHER OF THREE IS STILL WINNING AWARDS, AND FANS, ON FOX’S MASTERCHEF AND WE HAVE A SIMILAR SENSE WITH HIS THREE RESTAURANTS IN HIS NATIVE CHICAGO. -

Serendipity 2013 10.Pdf
What a pear! Elliot, left, and Bastianich, right, were photographed by Serendipity on August 30 at Tarry Market (co-owned by Bastianich and Mario Batali) in Port Chester, NY. In between takes, the guys, who are both musicians, had a great time looking through the market’s collection of rock ’n’ roll LPs. 100 OCTOBER 2013 FOODIES PA S EAUTY B EROVA, Z I ALON & S M GRAHAM ELLIOT AND JOE BASTIANICH ARE MORE THAN CO-JUDGES ANA friends ON FOX’s MASTERCHEF, THE TWO CULINARY GREATS ARE ALSO Z OLAND N GREAT FRIENDS. ON AIR, THEIR DEMEANORS DIFFer — Joe is THE SERIOUS ONE, GRAHAM IS THE EVERyman — but oFF CAMERA, AND AT SERENDIPITY’s 2013 GREENWICH WINE+FOOD FESTIVAL, GROOMING BY ZU CHRISTOPHER THEIR CHEMISTRY IS DELICIOUSLY FUN. PHOTOGRAPHS BY STEVE GIRALT We’ve all goTTEN ALONG FROM DAY ONE. WE HAVE A SIMILAR SENSE OF HUMOR, AND LOVE NOTHING MORE THAN TO BE SURROUNDED BY FOOD AND PEOPLE WHO ARE EXCITED TO COOK IT.” — on fellOW MASTERCHEF JUDGES JOE BASTIANICH AND GORDON RAMSAY 102 OCTOBER 2013 Elliot, right, with a MasterChef contestant and Joe Bastianich. ELLIOT BECAME THE grahamYOUNGEST FOUR-STAR CHEF IN THE COUNTRY AT AGE 27. NINE YEARS LATER, THE MUSICIAN, HUSBAND AND FATHER OF THREE IS STILL WINNING AWARDS, AND FANS, ON FOX’S MASTERCHEF AND WITH HIS THREE RESTAURANTS IN HIS NATIVE CHICAGO. HIS CUR- RENT PROJECTS INCLUDE AN UPCOMING BOOK, AND HE’S OPENING A LOCAL RESTAURANT BEFORE THE END OF THE YEAR! If someone said to you “I want to be a tricks and sharing stories from our past famous chef and open a restaurant,” culinary experiences. -

Praise Prime Time
August 17 - 23, 2019 Adam Devine, Danny McBride, Edi Patterson and John Goodman star in “The Righteous Gemstones” AUTO HOME FLOOD LIFE WORK Praise 101 E. Clinton St., Roseboro, N.C. 910-525-5222 prime time [email protected] We ought to weigh well, what we can only once decide. SEE WHAT YOUR NEIGHBORS Complete Funeral Service including: Traditional Funerals, Cremation Pre-Need-Pre-Planning Independently Owned & Operated ARE TALKING ABOUT! Since 1920’s FURNITURE - APPLIANCES - FLOOR COVERING ELECTRONICS - OUTDOOR POWER EQUIPMENT 910-592-7077 Butler Funeral Home 401 W. Roseboro Street 2 locations to Hwy. 24 Windwood Dr. Roseboro, NC better serve you Stedman, NC www.clintonappliance.com 910-525-5138 910-223-7400 910-525-4337 (fax) 910-307-0353(fax) Sampson Independent — Saturday, August 17, 2019 — Page 3 Sports This Week SATURDAY 9:55 p.m. WUVC MFL Fútbol Morelia From Pinehurst Resort and Country season. From Broncos Stadium at Mile 8:00 a.m. ESPN Get Up! (Live) (2h) 8:00 p.m. WRAZ NFL Football Jack- at Club América. From Estadio Azteca-- Club-- Pinehurst, N.C. (Live) (3h) High-- Denver, Colo. (Live) (3h) ESPN2 SportsCenter (1h) sonville Jaguars at Miami Dolphins. 7:00 a.m. DISC Major League Fishing Mexico City, Mexico (Live) (2h05) 4:00 p.m. WNCN NFL Football New ESPN2 Baseball Little League World 9:00 a.m. ESPN2 SportsCenter (1h) Pre-season. From Hard Rock Stadi- (2h) 10:00 p.m. WRDC Ring of Honor Orleans Saints at Los Angeles Chargers. Series. From Howard J. Lamade Stadi- 10:00 a.m. -

ROTASCOPE June 1, 2021
ROTASCOPE June 1, 2021 President's Message Meetings A Heart Full of Hope June is Rotary Fellowships Month 6/3 Jasmine Stewart - Celebrity Chef 6/10 Sen. John Albers & Rep. Mary Robichaux - State of the Union 6/17 It's a Wrap-Lunch at Lucky's! 6/24 No Meeting Events 6/7 GBI EHT Training - Set Up Crew 6/7 End Human Trafficking Police Training 6/7 GBI EHT Training - Snack Table Manning 6/7 GBI EHT Training - Lunch Serving The greatness of a community is most accurately measured by the compassionate actions of its members. LEADERSHIP Many of you have been involved with the construction, painting, and delivery of our picnic table project. President Lynne Lindsay President-Elect Terry Taylor Last week Past President Harvey and I delivered our table to Jacob’s Ladder. It now Immediate PP Gordon Owens sits proudly on a hill surrounded by trees and bird feeders, overlooking an organic Treasurer Alex Kaufman farm. Secretary John Carruth Foundation Don Horton The students promise to enjoy this hope, truth, love, and joy filled table for years. Membership Mike Agurkis This Week's Speaker Nancy Service Alterman Award Winning Master Chef Public Image Lee Patrick, III PAST DISTRICT GOVERNORS Cheryl Greenway 2012-13 Bob Hagan 2015-16 ROTARY CLUB OF ROSWELL Thursdays, 12:15 pm Roswell Area Park Bill Johnson Community Activity Building 10495 Woodstock Road Roswell, GA 30075 Rotary Online https://roswellrotary.club https://rotary6900.org/ https://rotary.org/ GET CLUB SMS ALERTS Text: CLUBALERTS Jasmine Stewart is the winner of MasterChef Junior, Season 5. -

OUTSTANDING RESTAURATEUR a Working
OUTSTANDING RESTAURATEUR A working restaurateur, actively involved in multiple restaurants in the United States, who has set uniformly high national standards as a creative force in the kitchen and/or in restaurant operations. Candidates must have been in the restaurant business for at least 10 years. Bob Amick Concentrics Restaurants, including One Midtown Kitchen, Two Urban Licks, and Trois, Atlanta, GA. Ashok Bajaj Ardeo, Bardeo, Bombay Club, The Oval Room, Rasika, and 701 Restaurant, Washington, DC. Tom Baron big Burrito Restaurant Group, including Mad Mex, Casbah, Eleven, Kaya, and Umi, Pittsburgh, PA. Joe Bastianich/Mario Batali Including Babbo Ristorante y Enoteca, Esca, Del Posto, Otto, Casa Mono, New York, NY. Pizzeria Mozza and Osteria Mozza, Los Angeles, CA. B&B Ristorante, Las Vegas, NV. Jimmy Bradley Red Cat Restaurants including The Red Cat and The Harrison, New York, NY. Larry and Richard D'Amico D'Amico Cucina, Campiello, Café Lurcat and Bar Lurcat, Masa, and D'Amico & Sons, Minneapolis, MN. Campiello, Café Lurcat and Bar Lurcat, and D'Amico & Sons, Naples, FL. Tom Douglas Tom Douglas Restaurants, including The Dahlia Lounge, Etta's Seafood, Palace Kitchen, Lola, Serious Pie, and The Dahlia Bakery, Seattle, WA. M. Steven Ells Chipotle Mexican Grills, Inc,. Denver, CO. More than 500 locations nationwide. Sam Fox Fox Restaurant Concepts, including The Green House, Olive & Ivy, and Bloom, Scottsdale, AZ. Wildflower and Blanco Tacos & Tequila, Tucson, AZ. North, Scottsdale and Glendale, AZ. Sauce, multiple outlets Tucson, AZ and Denver, CO. Jim Goode Goode Company Restaurants, including Goode Co. Texas Seafood (2 locations) Goode Co. Texas BBQ (2 locations), Goode Co.