Have the Highest Share in Health Care Spending in Developing Countries 1-6
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CD Mistry Is
C. D. Mistry Born: 1933, Chikhali, Dist. Navsari, Gujarat, India. Diploma in Painting (G.DA) Art Master (A.M.) C. D. Mistry is a painter from Ahmedabad, Gujarat. He is practicing painting from the last 40 years. Born: 1933, Chikhali, Dist. Navsari, Gujarat, India. Diploma in Painting (G.DA), Art Master (A.M.) AWARDS All India Exhibition of Art, Mysore, 1962. Gold Medal and cash award-Hydrabad Art Society, Andhra Pradesh, 1972. All India Exhibition of Art for Kalidas, Samaroh, Ujjan, 1974 . All India Exhibition of Art for Kalidas Samaroh, Gwalior, 1975. Bombay Art Society, Mumbai, 1976-1977. All India Fine Arts and Crafts Society, New Delhi, 1976. Indo-Arab Society, Mumbai - Glimpses of Patestine War and Peace Exhibition, 1977, a return ticket by Syrian Arab Airlines to Egypt, Cairo, Damascus, Palestine, Jerusalem etc. as a first award. National Award as a best designer for Printing and Decoration from Ministry of Information, New Delhi,1975. 3rd All India Contemporary Miniature Biennale on Folk Concept by Andhra Pradesh Council of Artists, Hyderabad, 1980. Hyderabad Art Society's cash award on Folk Painting, 1981. Gujarat State Lalit Kala Akademi award, 1985, 1988. National Lalit Kala Academy award, New Delhi, 1989. National Kalidas Akademi, Ujjain, 1990 . Awarded 'Senior Fellowship' from the Department of Culture and Human Resource, New Delhi, 1989 . Awarded an Award of Fellowship to the most Eminent Artist Senior Fellowship by Gujarat State Lalit Kala Akademi, 2001 . KALAVIBHUSHAN'-'A Title Award', AIFACS, (New Delhi), 2001. Konark Samman Award nominated by Orissa State Council of Culture, Bhuvneshwar, 1997. ONE MAN SHOW Sanskar Kendra-Musuem, Ahmedabad, 1972. -

Proposal for a Gujarati Script Root Zone Label Generation Ruleset (LGR)
Proposal for a Gujarati Root Zone LGR Neo-Brahmi Generation Panel Proposal for a Gujarati Script Root Zone Label Generation Ruleset (LGR) LGR Version: 3.0 Date: 2019-03-06 Document version: 3.6 Authors: Neo-Brahmi Generation Panel [NBGP] 1 General Information/ Overview/ Abstract The purpose of this document is to give an overview of the proposed Gujarati LGR in the XML format and the rationale behind the design decisions taken. It includes a discussion of relevant features of the script, the communities or languages using it, the process and methodology used and information on the contributors. The formal specification of the LGR can be found in the accompanying XML document: proposal-gujarati-lgr-06mar19-en.xml Labels for testing can be found in the accompanying text document: gujarati-test-labels-06mar19-en.txt 2 Script for which the LGR is proposed ISO 15924 Code: Gujr ISO 15924 Key N°: 320 ISO 15924 English Name: Gujarati Latin transliteration of native script name: gujarâtî Native name of the script: ગજુ રાતી Maximal Starting Repertoire (MSR) version: MSR-4 1 Proposal for a Gujarati Root Zone LGR Neo-Brahmi Generation Panel 3 Background on the Script and the Principal Languages Using it1 Gujarati (ગજુ રાતી) [also sometimes written as Gujerati, Gujarathi, Guzratee, Guujaratee, Gujrathi, and Gujerathi2] is an Indo-Aryan language native to the Indian state of Gujarat. It is part of the greater Indo-European language family. It is so named because Gujarati is the language of the Gujjars. Gujarati's origins can be traced back to Old Gujarati (circa 1100– 1500 AD). -

Annexure-V State/Circle Wise List of Post Offices Modernised/Upgraded
State/Circle wise list of Post Offices modernised/upgraded for Automatic Teller Machine (ATM) Annexure-V Sl No. State/UT Circle Office Regional Office Divisional Office Name of Operational Post Office ATMs Pin 1 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA PRAKASAM Addanki SO 523201 2 Andhra Pradesh ANDHRA PRADESH KURNOOL KURNOOL Adoni H.O 518301 3 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM AMALAPURAM Amalapuram H.O 533201 4 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Anantapur H.O 515001 5 Andhra Pradesh ANDHRA PRADESH Vijayawada Machilipatnam Avanigadda H.O 521121 6 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA TENALI Bapatla H.O 522101 7 Andhra Pradesh ANDHRA PRADESH Vijayawada Bhimavaram Bhimavaram H.O 534201 8 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA VIJAYAWADA Buckinghampet H.O 520002 9 Andhra Pradesh ANDHRA PRADESH KURNOOL TIRUPATI Chandragiri H.O 517101 10 Andhra Pradesh ANDHRA PRADESH Vijayawada Prakasam Chirala H.O 523155 11 Andhra Pradesh ANDHRA PRADESH KURNOOL CHITTOOR Chittoor H.O 517001 12 Andhra Pradesh ANDHRA PRADESH KURNOOL CUDDAPAH Cuddapah H.O 516001 13 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM VISAKHAPATNAM Dabagardens S.O 530020 14 Andhra Pradesh ANDHRA PRADESH KURNOOL HINDUPUR Dharmavaram H.O 515671 15 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA ELURU Eluru H.O 534001 16 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudivada Gudivada H.O 521301 17 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudur Gudur H.O 524101 18 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Guntakal H.O 515801 19 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA -

Karachi KATRAK BANDSTAND, CLIFTON PHOTO by KHUDABUX ABRO
FEZANA PAIZ 1377 AY 3746 ZRE VOL. 22, NO. 3 FALL/SEPTEMBER 2008 MahJOURJO Mehr-Avan-Adar 1377 (Fasli) G Mah Ardebehest-Khordad-Tir 1378 AY (Shenshai)N G Mah Khordad-Tir-AmardadAL 1378 AY (Kadmi) “Apru” Karachi KATRAK BANDSTAND, CLIFTON PHOTO BY KHUDABUX ABRO Also Inside: 2008 FEZANA AGM in Westminster, CA NextGenNow 2008 Conference 10th Anniversary Celebrations in Houston A Tribute to Gen. Sam Manekshaw PUBLICATION OF THE FEDERATION OF ZOROASTRIAN ASSOCIATIONS OF NORTH AMERICA PUBLICATION OF THE FEDERATION OF ZOROASTRIAN ASSOCIATIONS OF NORTH AMERICA Vol 22 No 3 Fall 2008, PAIZ 1377 AY 3746 ZRE President Bomi V Patel www.fezana.org Editor in Chief: Dolly Dastoor 2 Editorial [email protected] Technical Assistan: Coomi Gazdar Dolly Dastoor Consultant Editor: Lylah M. Alphonse, 3 Message from the President [email protected] 5 FEZANA Update Graphic & Layout: Shahrokh Khanizadeh, www.khanizadeh.info 6 Financial Report Cover design: Feroza Fitch, [email protected] 35 APRU KARACHI 50 Publications Chair: Behram Pastakia Columnists: Hoshang Shroff:: [email protected] Shazneen Rabadi Gandhi : 56 Renovations of Community Places of [email protected] Fereshteh Khatibi:: [email protected] Worship-Andheri Patel Agiary Behram Panthaki::[email protected] Behram Pastakia: [email protected] 78 In The News Mahrukh Motafram: [email protected] Nikan Khatibi: [email protected] 92 Interfaith /Interalia Copy editors: R Mehta, V Canteenwalla 99 North American Mobeds’ Council Subscription Managers: Kershaw Khumbatta : 106 Youthfully -

List of Officers Who Attended Courses at NCRB
List of officers who attened courses at NCRB Sr.No State/Organisation Name Rank YEAR 2000 SQL & RDBMS (INGRES) From 03/04/2000 to 20/04/2000 1 Andhra Pradesh Shri P. GOPALAKRISHNAMURTHY SI 2 Andhra Pradesh Shri P. MURALI KRISHNA INSPECTOR 3 Assam Shri AMULYA KUMAR DEKA SI 4 Delhi Shri SANDEEP KUMAR ASI 5 Gujarat Shri KALPESH DHIRAJLAL BHATT PWSI 6 Gujarat Shri SHRIDHAR NATVARRAO THAKARE PWSI 7 Jammu & Kashmir Shri TAHIR AHMED SI 8 Jammu & Kashmir Shri VIJAY KUMAR SI 9 Maharashtra Shri ABHIMAN SARKAR HEAD CONSTABLE 10 Maharashtra Shri MODAK YASHWANT MOHANIRAJ INSPECTOR 11 Mizoram Shri C. LALCHHUANKIMA ASI 12 Mizoram Shri F. RAMNGHAKLIANA ASI 13 Mizoram Shri MS. LALNUNTHARI HMAR ASI 14 Mizoram Shri R. ROTLUANGA ASI 15 Punjab Shri GURDEV SINGH INSPECTOR 16 Punjab Shri SUKHCHAIN SINGH SI 17 Tamil Nadu Shri JERALD ALEXANDER SI 18 Tamil Nadu Shri S. CHARLES SI 19 Tamil Nadu Shri SMT. C. KALAVATHEY INSPECTOR 20 Uttar Pradesh Shri INDU BHUSHAN NAUTIYAL SI 21 Uttar Pradesh Shri OM PRAKASH ARYA INSPECTOR 22 West Bengal Shri PARTHA PRATIM GUHA ASI 23 West Bengal Shri PURNA CHANDRA DUTTA ASI PC OPERATION & OFFICE AUTOMATION From 01/05/2000 to 12/05/2000 1 Andhra Pradesh Shri LALSAHEB BANDANAPUDI DY.SP 2 Andhra Pradesh Shri V. RUDRA KUMAR DY.SP 3 Border Security Force Shri ASHOK ARJUN PATIL DY.COMDT. 4 Border Security Force Shri DANIEL ADHIKARI DY.COMDT. 5 Border Security Force Shri DR. VINAYA BHARATI CMO 6 CISF Shri JISHNU PRASANNA MUKHERJEE ASST.COMDT. 7 CISF Shri K.K. SHARMA ASST.COMDT. -

Rohinton Mistry
Chronology i 1 Rohinton Mistry Mistrey_00_prelims1 9/6/04, 4:05 pm ii Chronology CCONTEMPORARY WWORLD WWRITERS series editor john thieme already published in the series Peter Carey bruce woodcock Kazuo Ishiguro barry lewis Hanif Kureishi bart moore-gilbert Timothy Mo elaine yee lin ho Toni Morrison jill matus Alice Munro coral ann howells Les Murray steven matthews Caryl Phillips bénédicte ledent Ngugi wa Thiong’o patrick williams Derek Walcott john thieme forthcoming Anita Desai shirley chew Hanif Kureishi bart moore-gilbert Les Murray steven matthews R. K. Narayan john thieme Caryl Phillips benedicte ledent Wole Soyinka abdulrazak gurnah CWW Mistrey_00_prelims2 9/6/04, 4:05 pm Chronology iii Rohinton Mistry PETER MOREY Manchester University Press Manchester and New York distributed exclusively in the USA by Palgrave Mistrey_00_prelims3 9/6/04, 4:05 pm iv Chronology Copyright © Peter Morey 2004 The right of Peter Morey to be identified as the author of this work has been asserted by him in accordance with the Copyright, Designs and Patents Act 1988. Published by Manchester University Press Oxford Road, Manchester m13 9nr, uk and Room 400, 175 Fifth Avenue, New York, ny 10010, usa www.manchesteruniversitypress.co.uk Distributed exclusively in the USA by Palgrave, 175 Fifth Avenue, New York, ny 10010, usa Distributed exclusively in Canada by ubc Press, University of British Columbia, 2029 West Mall, Vancouver, bc, Canada v6t 1z2 British Library Cataloguing-in-Publication Data A catalogue record for this book is available from the British -

Investor First Name Investor Middle Name Investor Last Name Father
Investor First Name Investor Middle Name Investor Last Name Father/Husband First Name Father/Husband Middle Name Father/Husband Last Name Address Country State District Pin Code Folio No. DP.ID-CL.ID. Account No. Invest Type Amount Transferred Proposed Date of Transfer to IEPF PAN Number Aadhar Number 74/153 GANDHI NAGAR A ARULMOZHI NA INDIA Tamil Nadu 636102 IN301774-10480786-0000 Amount for unclaimed and unpaid dividend 160.00 15-Sep-2019 ATTUR 1/26, VALLAL SEETHAKATHI SALAI A CHELLAPPA NA KILAKARAI (PO), INDIA Tamil Nadu 623517 12010900-00960311-TE00 Amount for unclaimed and unpaid dividend 60.00 15-Sep-2019 RAMANATHAPURAM KILAKARAI OLD NO E 109 NEW NO D A IRUDAYAM NA 6 DALMIA COLONY INDIA Tamil Nadu 621651 IN301637-40636357-0000 Amount for unclaimed and unpaid dividend 20.00 15-Sep-2019 KALAKUDI VIA LALGUDI OPP ANANDA PRINTERS I A J RAMACHANDRA JAYARAMACHAR STAGE DEVRAJ URS INDIA Karnataka 577201 IN300360-10245686-0000 Amount for unclaimed and unpaid dividend 8.00 15-Sep-2019 ACNPR4902M NAGAR SHIMOGA NEW NO.12 3RD CROSS STREET VADIVEL NAGAR A J VIJAYAKUMAR NA INDIA Tamil Nadu 632001 12010600-01683966-TE00 Amount for unclaimed and unpaid dividend 100.00 15-Sep-2019 SANKARAN PALAYAM VELLORE THIRUMANGALAM A M NIZAR NA OZHUKUPARAKKAL P O INDIA Kerala 691533 12023900-00295421-TE00 Amount for unclaimed and unpaid dividend 20.00 15-Sep-2019 AYUR AYUR FLAT - 503 SAI DATTA A MALLIKARJUNAPPA ANAGABHUSHANAPPA TOWERS RAMNAGAR INDIA Andhra Pradesh 515001 IN302863-10200863-0000 Amount for unclaimed and unpaid dividend 80.00 15-Sep-2019 AGYPA3274E -
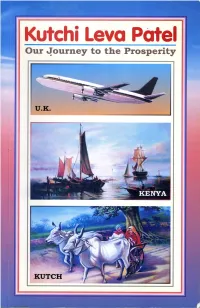
Kutchi Leva Patel Index Our Journey to the Prosperity Chapter Article Page No
Kutchi Leva Patel Index Our Journey to the Prosperity Chapter Article Page No. Author Shree S. P. Gorasia 1 Cutch Social & Cultural Society 10 First Published on: 2 Leva Patel Migration 14 Vikram Samvat – 2060 Ashadh Sood – 2nd (Ashadhi Beej) 3 Present Times 33 Date: 20th June 2004 4 Village of Madhapar 37 Second Published on: Recollection of Community Service Vikram Samvat – 2063 Ashadh Sood – 1st 5 Present Generation 55 Date: 15th July 2007 6 Kurmi-Kanbi - History 64 (Translated on 17 December 2006) 7 Our Kutch 77 Publication by Cutch Social and Cultural Society 8 Brief history of Kutch 81 London 9 Shyamji Krishna Varma 84 Printed by Umiya Printers- Bhuj 10 Dinbandhu John Hubert Smith 88 Gujarati version of this booklet (Aapnu Sthalantar) was 11 About Kutch 90 published by Cutch Social & Cultural Society at Claremont High School, London, during Ashadhi Beej celebrations on 12 Leva Patel Villages : 20th June 2004 (Vikram Savant 2060) with a generous support from Shree Harish Karsan Hirani. Madhapar 95 Kutchi Leva Patel Index Our Journey to the Prosperity Chapter Article Page No. Author Shree S. P. Gorasia 1 Cutch Social & Cultural Society 10 First Published on: 2 Leva Patel Migration 14 Vikram Samvat – 2060 Ashadh Sood – 2nd (Ashadhi Beej) 3 Present Times 33 Date: 20th June 2004 4 Village of Madhapar 37 Second Published on: Recollection of Community Service Vikram Samvat – 2063 Ashadh Sood – 1st 5 Present Generation 55 Date: 15th July 2007 6 Kurmi-Kanbi - History 64 (Translated on 17 December 2006) 7 Our Kutch 77 Publication by Cutch Social and Cultural Society 8 Brief history of Kutch 81 London 9 Shyamji Krishna Varma 84 Printed by Umiya Printers- Bhuj 10 Dinbandhu John Hubert Smith 88 Gujarati version of this booklet (Aapnu Sthalantar) was 11 About Kutch 90 published by Cutch Social & Cultural Society at Claremont High School, London, during Ashadhi Beej celebrations on 12 Leva Patel Villages : 20th June 2004 (Vikram Savant 2060) with a generous support from Shree Harish Karsan Hirani. -

INDIAN BUSINESSMEN in KENYA DURING the TWENTIETH CENTURY: a CASE STUDY John Irving Zarwan
INDIAN BUSINESSMEN IN KENYA DURING THE TWENTIETH CENTURY: A CASE STUDY John Irving Zarwan To cite this version: John Irving Zarwan. INDIAN BUSINESSMEN IN KENYA DURING THE TWENTIETH CEN- TURY: A CASE STUDY. History. Yale University, 1977. English. tel-01259828 HAL Id: tel-01259828 https://halshs.archives-ouvertes.fr/tel-01259828 Submitted on 21 Jan 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. This is an authorized facsimile, made from the microfilm master copy of the original dissertation or masters thesis published by UMI. Prior to publishing, UMI microfilms the original manuscript and returns it to the author or institution granting the degree. When an order is placed, the complete document is reproduced, on paper or in microform, from the master film copy. This is called on-demand publishing. The bibliographic information for this thesis is contained in UMI's Dissertation Abstracts database, the only central source for accessing almost every doctoral dissertation accepted in North America since 1861. l Dissertation UMa Information Service University Microfilms International A Bell & Howell Information Company 300 N. Zeeb Road, Ann Arbor, Michigan 48106 800-521-0600 OR 313/761-4700 Printed in 1987 by xerographic process on acid-free paper INFORMATION TO USERS This material was produced from a microfilm copy of the original document. -

Pharmaceutical Resonance 2021 Vol. 3 - Issue 2
Pharmaceutical Resonance 2021 Vol. 3 - Issue 2 REVIEW ARTICLE DRUG INFORMATION CENTER: AN OVERVIEW Vishal V. Laulkar, Mansi Mistry*, Karishma M. Rathi Dr. D. Y. Patil Institute of Pharmaceutical Sciences and Research, Pimpri, Pune, 411018, Maharashtra, India Abstract : Drug Information Centers (DICs) are defined as operational units that provide up-to-date, scientific, evidence backed and critically evaluated information on all aspects of drugs in an objective and timely manner. The different types of DIC’s are Academics, Institutional, Hospital and Industry related DICs. The purpose of establishing a drug information center is to promote rational use of drugs by providing authentic, individualized, critically reviewed, accurate and unbiased drug related information to the inquirer. The DICs help evaluate major drug related problem areas that gets frequent inquiries. The requirements for the DICs and general process to be followed to answer questions, specifically varies for each type. Standard operating procedures and detailed process protocols may help the DICs to produce better health related outcomes. DICs may perform various activities according to their type that are ultimately linked to promote safe, rational and evidence backed use of drugs as well as to promote research and publication work culture. The questions to the DICs are mainly asked by different health-care professionals regarding general properties of active substances, contents of particular preparations, dosage, side effects and indications/contraindications. To answer such scientifically complicated queries, pharmacist plays an important role. Drug information specialist pharmacist may help preparing scientific communications and contribute in education and training of health care professionals on safe and effective medication-use policies and processes. -

Ethnic Conflict and the Fate of Parsis in India: a Study of Rohinton Mistry's Tales from Firozshah
IOSR Journal Of Humanities And Social Science (IOSR-JHSS) Volume 20, Issue 4, Ver. V (Apr. 2015), PP 60-64 e-ISSN: 2279-0837, p-ISSN: 2279-0845. www.iosrjournals.org Ethnic conflict and the Fate of Parsis in India: a Study of Rohinton Mistry’s Tales from Firozshah Bag Moncy Mathew1, Assistant Professor, Department of English, Govt. Arts and Science College, Calicut Abstract: Rohinton Mistry is an Indian born Parsi writer settled in Canada. He writes about the ethnic conflict that his community faces from the right wing political parties in Bombay like the Shiv Sena. His short story collection titled Tales from Firozshah Bag describes the Bombay city of the 1960s and 70s from a Parsi perspective detailing the present condition of the Parsis and their loss of social, economic and political significance. The short stories in the collection also present the issue of ethnic conflict that the community had to face from the neighbouring communities that call themselves ‘sons of the soil’. This article aims to analyse the issue of ethnic conflict faced by the Parsi community in the post-independence period with reference to Mistry’s first collection of short stories titled Tales from Firozshah Bag. Keywords- Ethnic Conflict, Rohinton Mistry, Parsi Literature, Tales from Firozshah Bag. I. Introduction This paper undertakes to interrogate the conflicts the Parsi community had to face in the post independence period with special reference to the collection of short stories titled Tales From Firozshah Baag. Mistry was born in Bombay in 1952 and migrated to Canada in 1975, as he recollects in an interview with Adil Jussawalla, to become famous in the music world (Bharucha 73).He is a representative of the young Parsis of post independence period who have migrated to the richer countries in search of better opportunities. -
The Parsi Directory
HAMAZOR - ISSUE 1 2017 Kobad Ghandy in his youth, p 38 C o n t e n t s 04 WZO Calendar of Events - 2017 05 WZO Management pays Tribute to Ruby Contractor 07 WZO Gala Dinner-Dance - sammy bhiwandiwalla 08 Atashgah of Khinalig - farroukh jorat 13 Zoroastrian revival in Kurdistan 15 In Search of Zarathushti Kurds - fariborz rahnamoon 19 ZAC, Orange, Atash Kadeh Opening 21 2016 SSZ Conference - jehangir darukhanavala 26 The Global Working Group - dorab mistry 27 The Parsi Directory - now as an Android App 28 Congress 2000 Legacy continues 29 Lions Club at Byculla & WZO Trust 30 The Boomerang Effect - dina mcintyre 34 ‘Sajedo by Juddins’ - hoshang bhoot COVER 36 Lt Commodore Firdous Darabshah Mogal - marzban giara Image of the reconstructed kobad ghandy 38 A Lifelong Search for Freedom & Justice - Atashgah at Khinalig, 43 Combating a Killer Disease - homi khusrokhan Azerbaijan 46 Danny Khursigara - farishta dinshaw PHOTOGRAPHS 50 Three Decades of Expertise - dadrawala & billimoria 53 A Heritage Homestay - katie bhujwala Courtesy of individuals whose articles appear in 58 Ariana Vafadari, a Zarathushti Diva - philippa vafadari the magazine or as 60 Dinaz Vervatwala, against all odds - beyniaz edulji mentioned 62 History of the famous Parsi Batasas - edul davar WZO WEBSITE 65 A Passion for Culinary Excellence - ardeshir marker 67 Mumbai’s non-profit Music Organisation - benita fernando www.w-z-o.org 1 Sponsored by The World Zarathushtrian Trust Fund M e m b e r s o f t h e M a n a g i n g C o m m i t t e e London, England The World Zoroastrian