2016-Arch.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reticulate Hyperpigmentation of the Skin After Topical Application Of
Letters to the Editor 301 Reticulate Hyperpigmentation of the Skin After Topical Application of Benzoyl Peroxide Sir, Our two patients appeared to develop an irritant response on Benzoyl peroxide (BP) is an e¡ective and frequently used topical thetrunk afterapplication of 5% benzoyl peroxide. One medication for the treatment of acne vulgaris. It is a strong, patient applied BP to his face withnoirritation,consistentwith broad spectrum bactericidal agent that signi¢cantly decreases the ¢ndings of Hausteinetal.(3). Both patients then developed the number of Propionibacterium acnes in both the follicle and apattern of reticulate hyperpigmentation after their initial der- on surface skin (1). A common side e¡ect after usage is irritation matitis subsided. Biopsy in both cases was consistent with of the skin, usually manifested as a stinging or burning, and postin£ammatory hyperpigmentation. sometimes accompanied by erythema and scaling. Benzoyl per- Postin£ammatory hyperpigmentation develops after acute oxide is a strong irritant, but a weak allergen, rarely causing a or chronic in£ammation and trauma to the skin. The intensity contact dermatitis (2, 3). Tolerance can be achieved by gradually of the hypermelanosistendstobe more pronounced in darker- increasing the frequency of application over time. We describe skinnedindividuals. Other conditions that produce a pattern of two cases in which topical application of benzoyl peroxide reticulate hyperpigmentation include Riehl's melanosis, resulted in an unusual pattern of reticulate hyperpigmentation which is characterized by reticulate brown-black pigmenta- of the skin, most likely as a sequela of an irritant contact derma- tion of the face and neck. This is thought to be a result of a titis. -
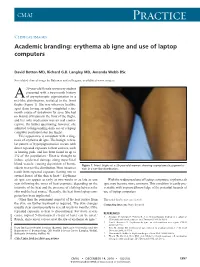
Erythema Ab Igne and Use of Laptop Computers
CMAJ Practice Clinical images Academic branding: erythema ab igne and use of laptop computers David Botten MD, Richard G.B. Langley MD, Amanda Webb BSc See related clinical image by Beleznay and colleagues, available at www.cmaj.ca 20-year-old female university student presented with a two-month history A of asymptomatic pigmentation in a net-like distribution, isolated to the front thighs (Figure 1). She was otherwise healthy, apart from having recently completed a six- month course of isotretinoin for acne. She had no history of trauma to the front of the thighs, and her only medication was an oral contra- ceptive. On further questioning, however, she admitted to longstanding daily use of a laptop computer positioned atop her thighs. This appearance is consistent with a diag- nosis of erythema ab igne. The benign, reticu- lar pattern of hyperpigmentation occurs with direct repeated exposure to heat sources, such as heating pads, and has been found in up to 3% of the population.1 Heat is thought to induce epidermal damage along superficial blood vessels, causing deposition of hemo- Figure 1: Front thighs of a 20-year-old woman showing asymptomatic pigmenta- siderin in a net-like distribution. Most instances tion in a net-like distribution. result from repeated exposure (lasting one to several hours) of the skin to heat.2,3 Erythema ab igne can appear as early as two weeks or as late as one With the widespread use of laptop computers, erythema ab year following the onset of heat exposure, depending on the igne may become more common. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -

Pharmaceuticals and Endocrine Active Chemicals in Minnesota Lakes
Pharmaceuticals and Endocrine Active Chemicals in Minnesota Lakes May 2013 Authors Mark Ferrey Contributors/acknowledgements The MPCA is reducing printing and mailing costs This report contains the results of a study that by using the Internet to distribute reports and characterizes the presence of unregulated information to wider audience. Visit our website contaminants in Minnesota’s lakes. The study for more information. was made possible through funding by the MPCA reports are printed on 100 percent post- Minnesota Clean Water Fund and by funding by consumer recycled content paper manufactured the U.S. Environmental Protection Agency without chlorine or chlorine derivatives. (EPA), which facilitated the sampling of lakes for this study. The Minnesota Pollution Control Agency (MPCA) thanks the following for assistance and advice in designing and carrying out this study: Steve Heiskary, Pam Anderson, Dereck Richter, Lee Engel, Amy Garcia, Will Long, Jesse Anderson, Ben Larson, and Kelly O’Hara for the long hours of sampling for this study. Cynthia Tomey, Kirsten Anderson, and Richard Grace of Axys Analytical Labs for the expert help in developing the list of analytes for this study and logistics to make it a success. Minnesota Pollution Control Agency 520 Lafayette Road North | Saint Paul, MN 55155-4194 | www.pca.state.mn.us | 651-296-6300 Toll free 800-657-3864 | TTY 651-282-5332 This report is available in alternative formats upon request, and online at www.pca.state.mn.us. Document number: tdr-g1-16 Contents Contents ........................................................................................................................................... -

HACEK Endocarditis: State-Of-The-Art Matthieu Revest, Gérald Egmann, Vincent Cattoir, Pierre Tattevin
HACEK endocarditis: state-of-the-art Matthieu Revest, Gérald Egmann, Vincent Cattoir, Pierre Tattevin To cite this version: Matthieu Revest, Gérald Egmann, Vincent Cattoir, Pierre Tattevin. HACEK endocarditis: state- of-the-art. Expert Review of Anti-infective Therapy, Expert Reviews, 2016, 14 (5), pp.523-530. 10.1586/14787210.2016.1164032. hal-01296779 HAL Id: hal-01296779 https://hal-univ-rennes1.archives-ouvertes.fr/hal-01296779 Submitted on 10 Jun 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. HACEK endocarditis: state-of-the-art Matthieu Revest1, Gérald Egmann2, Vincent Cattoir3, and Pierre Tattevin†1 ¹Infectious Diseases and Intensive Care Unit, Pontchaillou University Hospital, Rennes; ²Department of Emergency Medicine, SAMU 97.3, Centre Hospitalier Andrée Rosemon, Cayenne; 3Bacteriology, Pontchaillou University Hospital, Rennes, France †Author for correspondence: Prof. Pierre Tattevin, Infectious Diseases and Intensive Care Unit, Pontchaillou University Hospital, 2, rue Henri Le Guilloux, 35033 Rennes Cedex 9, France Tel.: +33 299289564 Fax.: + 33 299282452 [email protected] Abstract The HACEK group of bacteria – Haemophilus parainfluenzae, Aggregatibacter spp. (A. actinomycetemcomitans, A. aphrophilus, A. paraphrophilus, and A. segnis), Cardiobacterium spp. (C. hominis, C. valvarum), Eikenella corrodens, and Kingella spp. -

A. Fastidious Organisms MCQ 1 Explanation: the Most Common
MCQ Answer 1: A. Fastidious organisms MCQ 1 Explanation: The most common cause of culture-negative infective endocarditis in patients who have not been treated previously with antibiotics is fastidious organisms (1). In our patient, serology for Bartonella, Pasteurella and Coxiella was negative, but the Brucella antibody titer was 1:160 (reference range <1:20). Brucella titers higher than 1:160 in conjunction with a compatible clinical presentation are considered highly suggestive of infection especially in a non-endemic area (2), (3). Brucellosis can affect any organ system and cardiac involvement is rare, but endocarditis is the main cause of death due to brucellosis. Ideally, the diagnosis should be made by culture, however this test has a low sensitivity, is time-consuming, and poses a health risk for laboratory staff (4). HACEK organisms used to be considered the most common agent of culture-negative endocarditis, but with the current blood culture techniques, they can be easily isolated when incubated for at least five days. In our patient, the HACEK organism culture was negative at 5 days (5). Antibacterial therapy prior to blood culture sampling is a common cause of culture negative endocarditis. Our patient received empiric antibiotic therapy after the blood cultures were drawn. Valvular vegetations can be caused by noninfectious conditions and should be considered in the differential diagnoses of any patient with endocarditis. Nonbacterial thrombotic endocarditis (NBTE), such as marantic or Libman-Sachs endocarditis, happens in the setting of systemic lupus erythematosus, malignancy, or hypercoagulable state. The vegetations of NBTE are composed of fibrin thrombi that usually deposit on normal or minimally degenerated valves. -

USP Reference Standards Catalog
Last Updated On: January 6, 2016 USP Reference Standards Catalog Catalog # Description Current Lot Previous Lot CAS # NDC # Unit Price Special Restriction 1000408 Abacavir Sulfate R028L0 F1L487 (12/16) 188062-50-2 $222.00 (200 mg) 1000419 Abacavir Sulfate F0G248 188062-50-2 $692.00 Racemic (20 mg) (4-[2-amino-6-(cyclo propylamino)-9H-pur in-9yl]-2-cyclopenten e-1-methanol sulfate (2:1)) 1000420 Abacavir Related F1L311 F0H284 (10/13) 124752-25-6 $692.00 Compound A (20 mg) ([4-(2,6-diamino-9H- purin-9-yl)cyclopent- 2-enyl]methanol) 1000437 Abacavir Related F0M143 N/A $692.00 Compound D (20 mg) (N6-Cyclopropyl-9-{( 1R,4S)-4-[(2,5-diami no-6-chlorpyrimidin- 4-yloxy)methyl] cyclopent-2-enyl}-9H -purine-2,6-diamine) 1000441 Abacavir Related F1L318 F0H283 (10/13) N/A $692.00 Compound B (20 mg) ([4-(2,5-diamino-6-c Page 1 Last Updated On: January 6, 2016 USP Reference Standards Catalog Catalog # Description Current Lot Previous Lot CAS # NDC # Unit Price Special Restriction hloropyrimidin-4-yla mino)cyclopent-2-en yl]methanol) 1000452 Abacavir Related F1L322 F0H285 (09/13) 172015-79-1 $692.00 Compound C (20 mg) ([(1S,4R)-4-(2-amino -6-chloro-9H-purin-9 -yl)cyclopent-2-enyl] methanol hydrochloride) 1000485 Abacavir Related R039P0 F0J094 (11/16) N/A $692.00 Compounds Mixture (15 mg) 1000496 Abacavir F0J102 N/A $692.00 Stereoisomers Mixture (15 mg) 1000500 Abacavir System F0J097 N/A $692.00 Suitability Mixture (15 mg) 1000521 Acarbose (200 mg) F0M160 56180-94-0 $222.00 (COLD SHIPMENT REQUIRED) 1000532 Acarbose System F0L204 N/A $692.00 Suitability -

Blood Culture Bottles Incubation Period, 5 Days Or More?
February 2015 02/2015 NEWSLETTER Best Practices in Blood Culture Collection Blood culture bottles incubation period, 5 days or more? Introduction Blood is one of the most important specimens re- ceived by the microbiology laboratory for culture, and culture of blood is the most sensitive method for de- tection of bacteremia or fungemia. As we all know that the blood stream infection is one of the most se- rious problems in all infectious diseases. In general, adult patients with bacteremia are likely to have low quantities of bacteria in the blood, even in the setting of severe clinical symptoms. In addition, bacteremia in adults is generally intermittent. For this reason, multiple blood cultures, each containing large volumes of blood, are required to detect bacteraemia. Prior to initiation of antimicrobial therapy, at least two sets of blood cultures taken from separate venipuncture sites should be obtained. The technique, number of cultures, and volume of blood are more important factors for detection of bacteremia than timing of culture collection. Length of Incubation of Blood Cultures In routine circumstances, using automated continuous monitoring systems such as Becton Dickinson BACTEC System, blood cultures need not be incubated for longer than 5 days (1, 2, 3, 4, 5). For laborato- ries using manual blood culture systems, 7 days should suffice in most circumstances (6). Patient suspected Infectious Endocarditis (IE) A recent study at the Mayo Clinic, in which one of the widely used continuous monitoring blood culture systems was used, demonstrated that 99.5% of non-endocarditis BSIs and 100% of endocarditis epi- sodes were detected within 5 days of incubation (1). -

Microbiology Course Specification 1St, 2Nd Year of M.B.B.Ch
Faculty of Medicine Aswan University Microbiology Course Specification 1st, 2nd year of M.B.B.Ch. Program (Integrated system) 2019-2020 No. ILOs Practical Topic wks. hrs 1. B.1, C.1 Lab safety -Microscope 1st 2hrs D.1, D2 2. A6, B3 Sterilization, disinfection and 1st 2hrs D1, D2 antisepsis 3. A2, B.1 Laboratory diagnosis of bacterial 2nd 2 hrs C1, C2 infection (Simple and Gram’s stain) D1, D2 4. A6, B3 Ziehl Neelsen stain 2nd 2hrs 5. A3, B.1, Laboratory diagnosis of bacterial 3rd 2hrs C3 infection (Culture media I) D1, D2 6. A3, B1, Laboratory diagnosis of bacterial 3rd 2hrs C3, infection (Culture media II) D1, D2 7. A3, B2, , Laboratory diagnosis of bacterial 4th 2hrs C3, D1, infection (Biochemical reactions D2 Molecular diagnostic techniques) 8. A7, B.4 Antimicrobial susceptibility testing 4th 2hrs 9. A8, B5, Laboratory diagnosis of viral 5th 2hrs C5, D1, infections D2 A8, C2, Laboratory diagnosis of fungal 01. B.6, D1, 5th infections D2 A10, 10. B.7, C4, Serology I 6th D1, D2 A10, 12. B.7, C4 Serology II 6th D.1, D2 A10, 13. B.7, C4 Serology III 7th D.1, D2 A20, 04. B12, C8- Basics of infection control 7th 9 A2- Memorize the microorganism morphology A3- Recall bacterial growth requirements and replication. A6- Describe different methods of sterilization A7- Recognize proper selection of antimicrobials. A8- Recall general knowledge in the field of viral and fungal diseases. A10- Identify the role of the immune system against microbial infection. A20- State the basics of infection control B1- Differentiate the microorganism morphology B2- Explain genotypic variations and recombinant DNA technology B3- Compare between the different sterilization methods. -

Toxicity Assessment of the Antimicrobial Triclocarban Using Sub-Lethal Behaviour and Reproduction Endpoints Melanie Raby Ryerson University
Ryerson University Digital Commons @ Ryerson Theses and dissertations 1-1-2013 Toxicity Assessment Of The Antimicrobial Triclocarban Using Sub-Lethal Behaviour And Reproduction Endpoints Melanie Raby Ryerson University Follow this and additional works at: http://digitalcommons.ryerson.ca/dissertations Part of the Environmental Sciences Commons Recommended Citation Raby, Melanie, "Toxicity Assessment Of The Antimicrobial Triclocarban Using Sub-Lethal Behaviour And Reproduction Endpoints" (2013). Theses and dissertations. Paper 2017. This Thesis is brought to you for free and open access by Digital Commons @ Ryerson. It has been accepted for inclusion in Theses and dissertations by an authorized administrator of Digital Commons @ Ryerson. For more information, please contact [email protected]. TOXICITY ASSESSMENT OF THE ANTIMICROBIAL TRICLOCARBAN USING SUB-LETHAL BEHAVIOUR AND REPRODUCTION ENDPOINTS by Melanie Raby Bachelor of Science (Honours) University of Waterloo, 2011 A thesis presented to Ryerson University in partial fulfillment of the requirement for the degree of Master of Applied Science in the Program of Environmental Applied Science and Management Toronto, Ontario, Canada, 2013 © MELANIE RABY, 2013 Author’s Declaration I hereby declare that I am the sole author of this thesis. This is a true copy of the thesis, including any required final revisions, and accepted by my examiners. I authorize Ryerson University to lend this thesis to other institutions or individuals for the purpose of scholarly research. I further authorize Ryerson University to reproduce this thesis by photocopying or by other means, in total or in part, at the request of other institutions or individuals for the purpose of scholarly research. I understand that my thesis may be made electronically available to the public. -

The 5 Stupidest Chemicals That Shouldn't Be in Your House (PDF)
MARCH 2013 NRDC faCT SHEET FS:13-03-A The 5 Stupidest Chemicals That Shouldn’t be in Your House As you begin the annual spring cleaning purge, make sure that you aren’t leaving behind a house filled with toxic chemicals that can harm you, your family, and your pets. Get rid of the chemicals that harm more than they help. 1. ANTIBACTERIAL PRODUCTS 2. TOXIC FLAME RETARDANTS Soaps, cosmetics, cleansers, lotions, toothpaste and other Furniture foam is saturated with flame retardant chemicals products may carry an “antibacterial” label, but you are really that not only don’t stop furniture fires, but also make fires paying extra for unnecessary additives like triclosan and its more toxic by forming deadly gases and soot, the real killers chemical cousin triclocarban—which may be doing more in most fires. What’s worse, flame retardant chemicals are harm than good. Triclosan is found in over 80 percent of linked to real and measurable health impacts, including Americans’ bodies and exposure has been linked to allergies, lower IQs and decreased attention spans for children exposed impaired reproduction, hormone disruption, and weakened in the womb, male infertility, male birth defects, and early muscles. The U.S. Food and Drug Administration (FDA) puberty in girls. A recent study in animals linked flame admitted that triclosan is no more effective at preventing retardants to autism and obesity. illness than regular soap. Widespread use—in everything Americans carry much higher levels of flame retardants from cutting boards, yoga mats, bedding, soaps and gels— in their bodies than anyone else in the world, due in large could also be promoting drug-resistant bacteria. -

CSI Dermatology
Meagen M. McCusker, MD [email protected] Integrated Dermatology, Enfield, CT AbbVie - Speaker Case-based scenarios, using look-alike photos, comparing the dermatologic manifestations of systemic disease to dermatologic disease. Select the clinical photo that best matches the clinical vignette. Review the skin findings that help differentiate the two cases. Review etiology/pathogenesis when understood and discuss treatments. Case 1: Scaly Serpiginous Eruption This patient was evaluated for a progressively worsening pruritic rash associated with dyspnea on exertion and 5-kg weight loss. Despite its dramatic appearance, the patient reported no itch. KOH examination is negative (But, who’s good at those anyway?) A. B. Case 1: Scaly Serpiginous Eruption This patient was evaluated for a progressively worsening pruritic rash associated with dyspnea on exertion and 5-kg weight loss. Despite its dramatic appearance, the patient reported no itch. KOH examination is negative (But, who’s good at those anyway?) A. Correct. B. Tinea Corporis Erythema Gyratum Repens Erythema Gyratum Repens Tinea corporis Rare paraneoplastic T. rubrum > T. mentagrophytes phenomenon typically > M. canis associated with lung Risk factors cancer>esophageal and breast Close contact, previous cancers. infection, Less commonly associated with occupational/recreational connective tissue disorders such exposure, contaminated as Lupus or Rheumatoid furniture or clothing, Arthritis gymnasium, locker rooms “Figurate erythema” migrates up 1-3 week incubation → to 1 cm a day centrifugal spread from point of Resolves with treatment of the invasion with central clearing malignancy This patient was diagnosed with squamous cell carcinoma of the lung. Case 2: Purpuric Eruption on the Legs & Buttocks A 12-year old boy presents with a recent history of upper respiratory tract infection, fever and malaise.