Bacteriology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Food Poisoning Toxins of Bacillus Cereus
toxins Review The Food Poisoning Toxins of Bacillus cereus Richard Dietrich 1,†, Nadja Jessberger 1,*,†, Monika Ehling-Schulz 2 , Erwin Märtlbauer 1 and Per Einar Granum 3 1 Department of Veterinary Sciences, Faculty of Veterinary Medicine, Ludwig Maximilian University of Munich, Schönleutnerstr. 8, 85764 Oberschleißheim, Germany; [email protected] (R.D.); [email protected] (E.M.) 2 Department of Pathobiology, Functional Microbiology, Institute of Microbiology, University of Veterinary Medicine Vienna, 1210 Vienna, Austria; [email protected] 3 Department of Food Safety and Infection Biology, Faculty of Veterinary Medicine, Norwegian University of Life Sciences, P.O. Box 5003 NMBU, 1432 Ås, Norway; [email protected] * Correspondence: [email protected] † These authors have contributed equally to this work. Abstract: Bacillus cereus is a ubiquitous soil bacterium responsible for two types of food-associated gastrointestinal diseases. While the emetic type, a food intoxication, manifests in nausea and vomiting, food infections with enteropathogenic strains cause diarrhea and abdominal pain. Causative toxins are the cyclic dodecadepsipeptide cereulide, and the proteinaceous enterotoxins hemolysin BL (Hbl), nonhemolytic enterotoxin (Nhe) and cytotoxin K (CytK), respectively. This review covers the current knowledge on distribution and genetic organization of the toxin genes, as well as mechanisms of enterotoxin gene regulation and toxin secretion. In this context, the exceptionally high variability of toxin production between single strains is highlighted. In addition, the mode of action of the pore-forming enterotoxins and their effect on target cells is described in detail. The main focus of this review are the two tripartite enterotoxin complexes Hbl and Nhe, but the latest findings on cereulide and CytK are also presented, as well as methods for toxin detection, and the contribution of further putative virulence factors to the diarrheal disease. -

Group a Streptococcus Produce Pilus-Like Structures Containing Protective Antigens and Lancefield T Antigens
Group A Streptococcus produce pilus-like structures containing protective antigens and Lancefield T antigens Marirosa Mora*†, Giuliano Bensi*†, Sabrina Capo*, Fabiana Falugi*, Chiara Zingaretti*, Andrea G. O. Manetti*, Tiziana Maggi*, Anna Rita Taddei‡, Guido Grandi*, and John L. Telford*§ *Chiron Vaccines, Via Fiorentina 1, 53100 Siena, Italy; and ‡Centro Interdipartimentale di Microscopia Elettronica, University of Tuscia, 01100 Viterbo, Italy Communicated by Rino Rappuoli, Chiron Corporation, Siena, Italy, September 8, 2005 (received for review July 29, 2005) Although pili have long been recognized in Gram-negative patho- extensively characterized and despite five decades of study, there gens as important virulence factors involved in adhesion and is still very little known about the structure and variability of T invasion, very little is known about extended surface organelles in antigens, although a gene of unknown function has been shown Gram-positive pathogens. Here we report that Group A Strepto- to code for the antigen recognized by T6 sera (9). Here we show coccus (GAS), a Gram-positive human-specific pathogen that that four of the 20 T antigens correspond to trypsin-resistant pili causes pharyngitis, impetigo, invasive disease, necrotizing fasciitis, composed of putative adhesion proteins and that recombinant and autoimmune sequelae has long, surface-exposed, pilus-like pilus proteins confer protection against lethal GAS challenge in structures composed of members of a family of extracellular a mouse model of infection and invasive disease. matrix-binding proteins. We describe four variant pili and show that each is recognized by a specific serum of the Lancefield Materials and Methods T-typing system, which has been used for over five decades to Bacterial Strains, Media, and Growth Conditions. -

The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio In
microorganisms Review The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio in the Treatment of Obesity and Inflammatory Bowel disease Spase Stojanov 1,2, Aleš Berlec 1,2 and Borut Štrukelj 1,2,* 1 Faculty of Pharmacy, University of Ljubljana, SI-1000 Ljubljana, Slovenia; [email protected] (S.S.); [email protected] (A.B.) 2 Department of Biotechnology, Jožef Stefan Institute, SI-1000 Ljubljana, Slovenia * Correspondence: borut.strukelj@ffa.uni-lj.si Received: 16 September 2020; Accepted: 31 October 2020; Published: 1 November 2020 Abstract: The two most important bacterial phyla in the gastrointestinal tract, Firmicutes and Bacteroidetes, have gained much attention in recent years. The Firmicutes/Bacteroidetes (F/B) ratio is widely accepted to have an important influence in maintaining normal intestinal homeostasis. Increased or decreased F/B ratio is regarded as dysbiosis, whereby the former is usually observed with obesity, and the latter with inflammatory bowel disease (IBD). Probiotics as live microorganisms can confer health benefits to the host when administered in adequate amounts. There is considerable evidence of their nutritional and immunosuppressive properties including reports that elucidate the association of probiotics with the F/B ratio, obesity, and IBD. Orally administered probiotics can contribute to the restoration of dysbiotic microbiota and to the prevention of obesity or IBD. However, as the effects of different probiotics on the F/B ratio differ, selecting the appropriate species or mixture is crucial. The most commonly tested probiotics for modifying the F/B ratio and treating obesity and IBD are from the genus Lactobacillus. In this paper, we review the effects of probiotics on the F/B ratio that lead to weight loss or immunosuppression. -
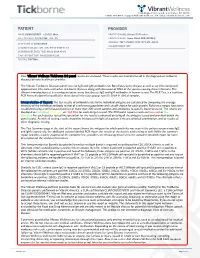
View Tickborne Diseases Sample Report
1360 Bayport Ave, Ste B. San Carlos, CA 94070 1(866) 364-0963 | [email protected] | www. vibrant-wellness.com PATIENT PROVIDER NAME: DEMO REPORT GENDER: Male PRACTICE NAME: Vibrant IT4 Practice DATE OF BIRTH: 04/14/1998 AGE: 22 PROVIDER NAME: Demo Client, DDD (999994) ADDRESS: TEST STREET, TEST CITY, KY- 42437. ACCESSION ID: 2009220006 PHLEBOTOMIST: 607 SPECIMEN COLLECTION TIME: 09-21-2020 11:14 SPECIMEN RECEIVED TIME: 09-22-2020 05:14 FINAL REPORT TIME: 09-25-2020 15:56 FASTING: FASTING Your Vibrant Wellness TickBorne 2.0 panel results are enclosed. These results are intended to aid in the diagnosis of tickborne diseases by your healthcare provider. The Vibrant Tickborne Diseases panel tests for IgG and IgM antibodies for Borreliosis/Lyme disease as well as co-infection(s) and opportunistic infections with other tick-borne illnesses along with detection of DNA of the species causing these infections. The Vibrant Immunochip test is a semiquantitative assay that detects IgG and IgM antibodies in human serum. The PCR Test is a real-time PCR Assay designed for qualitative detection of infectious group- specific DNA in clinical samples. Interpretation of Report: The test results of antibody levels to the individual antigens are calculated by comparing the average intensity of the individual antibody to that of a reference population and cut-off chosen for each protein. Reference ranges have been established using a well characterized set of more than 300 serum samples and antibodies to specific bacteria tested. The results are displayed as In Control, Moderate, or High Risk.for each antigen tested. -

Appendix III: OTU's Found to Be Differentially Abundant Between CD and Control Patients Via Metagenomeseq Analysis
Appendix III: OTU's found to be differentially abundant between CD and control patients via metagenomeSeq analysis OTU Log2 (FC CD / FDR Adjusted Phylum Class Order Family Genus Species Number Control) p value 518372 Firmicutes Clostridia Clostridiales Ruminococcaceae Faecalibacterium prausnitzii 2.16 5.69E-08 194497 Firmicutes Clostridia Clostridiales Ruminococcaceae NA NA 2.15 8.93E-06 175761 Firmicutes Clostridia Clostridiales Ruminococcaceae NA NA 5.74 1.99E-05 193709 Firmicutes Clostridia Clostridiales Ruminococcaceae NA NA 2.40 2.14E-05 4464079 Bacteroidetes Bacteroidia Bacteroidales Bacteroidaceae Bacteroides NA 7.79 0.000123188 20421 Firmicutes Clostridia Clostridiales Lachnospiraceae Coprococcus NA 1.19 0.00013719 3044876 Firmicutes Clostridia Clostridiales Lachnospiraceae [Ruminococcus] gnavus -4.32 0.000194983 184000 Firmicutes Clostridia Clostridiales Ruminococcaceae Faecalibacterium prausnitzii 2.81 0.000306032 4392484 Bacteroidetes Bacteroidia Bacteroidales Bacteroidaceae Bacteroides NA 5.53 0.000339948 528715 Firmicutes Clostridia Clostridiales Ruminococcaceae Faecalibacterium prausnitzii 2.17 0.000722263 186707 Firmicutes Clostridia Clostridiales NA NA NA 2.28 0.001028539 193101 Firmicutes Clostridia Clostridiales Ruminococcaceae NA NA 1.90 0.001230738 339685 Firmicutes Clostridia Clostridiales Peptococcaceae Peptococcus NA 3.52 0.001382447 101237 Firmicutes Clostridia Clostridiales NA NA NA 2.64 0.001415109 347690 Firmicutes Clostridia Clostridiales Ruminococcaceae Oscillospira NA 3.18 0.00152075 2110315 Firmicutes Clostridia -

Robust Taxonomic Classification of Uncharted Microbial Sequences and Bins with CAT and BAT
bioRxiv preprint doi: https://doi.org/10.1101/530188; this version posted January 24, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Robust taxonomic classification of uncharted microbial sequences and bins with CAT and BAT F.A. Bastiaan von Meijenfeldt1,†, Ksenia Arkhipova1,†, Diego D. Cambuy1, Felipe H. Coutinho2,3, Bas E. Dutilh1,2,* 1 Theoretical Biology and Bioinformatics, Science for Life, Utrecht University, The Netherlands. 2 Centre for Molecular and Biomolecular Informatics, Radboud University Medical Centre, Nijmegen, The Netherlands. 3 Instituto de Biologia, Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil. * To whom correspondence should be addressed. Tel: +31 30 253 4212; Email: [email protected]. † These authors contributed equally to this work. Present Address: [Felipe H. Couthinho], Evolutionary Genomics Group, Departamento de Produccíon y Microbiología, Universidad Miguel Hernández, Campus San Juan, San Juan, Alicante 03550, Spain. ABSTRACT Current-day metagenomics increasingly requires taxonomic classification of long DNA sequences and metagenome-assembled genomes (MAGs) of unknown microorganisms. We show that the standard best-hit approach often leads to classifications that are too specific. We present tools to classify high- quality metagenomic contigs (Contig Annotation Tool, CAT) and MAGs (Bin Annotation Tool, BAT) and thoroughly benchmark them with simulated metagenomic sequences that are classified against a reference database where related sequences are increasingly removed, thereby simulating increasingly unknown queries. We find that the query sequences are correctly classified at low taxonomic ranks if closely related organisms are present in the reference database, while classifications are made higher in the taxonomy when closely related organisms are absent, thus avoiding spurious classification specificity. -

Introduction to Bacteriology and Bacterial Structure/Function
INTRODUCTION TO BACTERIOLOGY AND BACTERIAL STRUCTURE/FUNCTION LEARNING OBJECTIVES To describe historical landmarks of medical microbiology To describe Koch’s Postulates To describe the characteristic structures and chemical nature of cellular constituents that distinguish eukaryotic and prokaryotic cells To describe chemical, structural, and functional components of the bacterial cytoplasmic and outer membranes, cell wall and surface appendages To name the general structures, and polymers that make up bacterial cell walls To explain the differences between gram negative and gram positive cells To describe the chemical composition, function and serological classification as H antigen of bacterial flagella and how they differ from flagella of eucaryotic cells To describe the chemical composition and function of pili To explain the unique chemical composition of bacterial spores To list medically relevant bacteria that form spores To explain the function of spores in terms of chemical and heat resistance To describe characteristics of different types of membrane transport To describe the exact cellular location and serological classification as O antigen of Lipopolysaccharide (LPS) To explain how the structure of LPS confers antigenic specificity and toxicity To describe the exact cellular location of Lipid A To explain the term endotoxin in terms of its chemical composition and location in bacterial cells INTRODUCTION TO BACTERIOLOGY 1. Two main threads in the history of bacteriology: 1) the natural history of bacteria and 2) the contagious nature of infectious diseases, were united in the latter half of the 19th century. During that period many of the bacteria that cause human disease were identified and characterized. 2. Individual bacteria were first observed microscopically by Antony van Leeuwenhoek at the end of the 17th century. -

Sporulation Evolution and Specialization in Bacillus
bioRxiv preprint doi: https://doi.org/10.1101/473793; this version posted March 11, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Research article From root to tips: sporulation evolution and specialization in Bacillus subtilis and the intestinal pathogen Clostridioides difficile Paula Ramos-Silva1*, Mónica Serrano2, Adriano O. Henriques2 1Instituto Gulbenkian de Ciência, Oeiras, Portugal 2Instituto de Tecnologia Química e Biológica, Universidade Nova de Lisboa, Oeiras, Portugal *Corresponding author: Present address: Naturalis Biodiversity Center, Marine Biodiversity, Leiden, The Netherlands Phone: 0031 717519283 Email: [email protected] (Paula Ramos-Silva) Running title: Sporulation from root to tips Keywords: sporulation, bacterial genome evolution, horizontal gene transfer, taxon- specific genes, Bacillus subtilis, Clostridioides difficile 1 bioRxiv preprint doi: https://doi.org/10.1101/473793; this version posted March 11, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Abstract Bacteria of the Firmicutes phylum are able to enter a developmental pathway that culminates with the formation of a highly resistant, dormant spore. Spores allow environmental persistence, dissemination and for pathogens, are infection vehicles. In both the model Bacillus subtilis, an aerobic species, and in the intestinal pathogen Clostridioides difficile, an obligate anaerobe, sporulation mobilizes hundreds of genes. -

Structural Changes in the Oral Microbiome of the Adolescent
www.nature.com/scientificreports OPEN Structural changes in the oral microbiome of the adolescent patients with moderate or severe dental fuorosis Qian Wang1,2, Xuelan Chen1,4, Huan Hu2, Xiaoyuan Wei3, Xiaofan Wang3, Zehui Peng4, Rui Ma4, Qian Zhao4, Jiangchao Zhao3*, Jianguo Liu1* & Feilong Deng1,2,3* Dental fuorosis is a very prevalent endemic disease. Although oral microbiome has been reported to correlate with diferent oral diseases, there appears to be an absence of research recognizing any relationship between the severity of dental fuorosis and the oral microbiome. To this end, we investigated the changes in oral microbial community structure and identifed bacterial species associated with moderate and severe dental fuorosis. Salivary samples of 42 individuals, assigned into Healthy (N = 9), Mild (N = 14) and Moderate/Severe (M&S, N = 19), were investigated using the V4 region of 16S rRNA gene. The oral microbial community structure based on Bray Curtis and Weighted Unifrac were signifcantly changed in the M&S group compared with both of Healthy and Mild. As the predominant phyla, Firmicutes and Bacteroidetes showed variation in the relative abundance among groups. The Firmicutes/Bacteroidetes (F/B) ratio was signifcantly higher in the M&S group. LEfSe analysis was used to identify diferentially represented taxa at the species level. Several genera such as Streptococcus mitis, Gemella parahaemolysans, Lactococcus lactis, and Fusobacterium nucleatum, were signifcantly more abundant in patients with moderate/severe dental fuorosis, while Prevotella melaninogenica and Schaalia odontolytica were enriched in the Healthy group. In conclusion, our study indicates oral microbiome shift in patients with moderate/severe dental fuorosis. -

Distribution and Characteristics of Bacillus Bacteria Associated with Hydrobionts and the Waters of the Peter the Great Bay, Sea of Japan I
ISSN 0026-2617, Microbiology, 2008, Vol. 77, No. 4, pp. 497–503. © Pleiades Publishing, Ltd., 2008. Original Russian Text © I.A. Beleneva, 2008, published in Mikrobiologiya, 2008, Vol. 77, No. 4, pp. 558–565. EXPERIMENTAL ARTICLES Distribution and Characteristics of Bacillus Bacteria Associated with Hydrobionts and the Waters of the Peter the Great Bay, Sea of Japan I. A. Beleneva1 Zhirmunskii Institute of Marine Biology, Far East Division, Russian Academy of Sciences, ul. Pal’chevskogo, 17, Vladivostok 690041, Russia Received May 28, 2007 Abstract—Bacilli of the species Bacillus subtilis, B. pumilus, B. mycoides, B. marinus and B. licheniformis (a total of 53 strains) were isolated from 15 invertebrate species and the water of the Vostok Bay, Peter the Great Bay, Sea of Japan. Bacilli were most often isolated from bivalves (22.7%) and sea cucumbers (18.9%); they occurred less frequently in sea urchins and starfish (13.2 and 7.5%, respectively). Most of bacilli strains were isolated from invertebrates inhabiting silted sediments. No Bacillus spp. strains were isolated from invertebrates inhabiting stony and sandy environments. The species diversity of bacilli isolated from marine objects under study was low. Almost all bacterial isolates were resistant to lincomycin. Unlike B. pumilus, B. subtilis isolates were mostly resistant to benzylpenicillin and ampicillin. Antibiotic sensitivity of B. licheniformis strains was variable (two strains were resistant to benzylpenicillin and oxacillin, while one was sensitive). A significant fraction of isolated bacilli contained pigments. Pigmented strains were more often isolated from seawater sam- ples, while colorless ones predominated within hydrobionts. B. subtilis colonies had the broadest range of co- lors. -

Probiotic Lactic Acid Bacteria Vs. Bacilli: Pros and Cons ARTHUR C
Probiotic lactic acid bacteria vs. bacilli: pros and cons ARTHUR C. OUWEHAND1*, SOFIA FORSSTEN1, MARKUS LEHTINEN1, ELIZABETH GALBRAITH2, ELLEN DAVIS2 *Corresponding author 1. Active Nutrition, DuPont Nutrition & Health, Sokeritehtaantie 20, 02460 Kantvik, Finland Arthur C. Ouwehand 2. Animal and Environmental Applications, DuPont Nutrition & Health, W227 N752 Westmound Drive, Waukesha, WI 53186, USA KEYWORDS: probiotic, lactic acid bacteria, Lactobacillus, Bifidobacterium, Bacillus, spores ABSTRACT: Both lactic acid bacteria (LAB) and bacilli are commercialised as probiotics; LAB are mainly utilised as live and active or dormant cells, while bacilli are utilised as spores. Belonging to very different genera, they have different technological properties. LAB have a longer history of use as probiotics and therefore have a broader base as far as health efficacy documentation is concerned. The question therefore sometimes arises; strains from which of these groups make better probiotics? Considering the fact that probiotics, by definition, have to be viable in sufficient numbers and have to have documented health benefits, this is not a relevant question. Any microbial strain has to fulfil these criteria in order to qualify as a probiotic. The current paper reviews and compares the available data for both groups of organisms. Pre - Probiotics INTRODUCTION In order to supply consumers with products that provide meaningful levels of probiotics, several requirements have There is no legal description of probiotics. However, the most to be fulfilled by probiotic strains selected for industrial commonly accepted definition is from a FAO/WHO working production. Quality-control must be vigilantly performed, group: “Live microorganisms which when administered in assuring identity, viability and absence of contaminants. -

HACEK Endocarditis: State-Of-The-Art Matthieu Revest, Gérald Egmann, Vincent Cattoir, Pierre Tattevin
HACEK endocarditis: state-of-the-art Matthieu Revest, Gérald Egmann, Vincent Cattoir, Pierre Tattevin To cite this version: Matthieu Revest, Gérald Egmann, Vincent Cattoir, Pierre Tattevin. HACEK endocarditis: state- of-the-art. Expert Review of Anti-infective Therapy, Expert Reviews, 2016, 14 (5), pp.523-530. 10.1586/14787210.2016.1164032. hal-01296779 HAL Id: hal-01296779 https://hal-univ-rennes1.archives-ouvertes.fr/hal-01296779 Submitted on 10 Jun 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. HACEK endocarditis: state-of-the-art Matthieu Revest1, Gérald Egmann2, Vincent Cattoir3, and Pierre Tattevin†1 ¹Infectious Diseases and Intensive Care Unit, Pontchaillou University Hospital, Rennes; ²Department of Emergency Medicine, SAMU 97.3, Centre Hospitalier Andrée Rosemon, Cayenne; 3Bacteriology, Pontchaillou University Hospital, Rennes, France †Author for correspondence: Prof. Pierre Tattevin, Infectious Diseases and Intensive Care Unit, Pontchaillou University Hospital, 2, rue Henri Le Guilloux, 35033 Rennes Cedex 9, France Tel.: +33 299289564 Fax.: + 33 299282452 [email protected] Abstract The HACEK group of bacteria – Haemophilus parainfluenzae, Aggregatibacter spp. (A. actinomycetemcomitans, A. aphrophilus, A. paraphrophilus, and A. segnis), Cardiobacterium spp. (C. hominis, C. valvarum), Eikenella corrodens, and Kingella spp.