Healthcare Industry Highlight: Revenue Cycle Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Advancing Standards for Precision Medicine
Advancing Standards for Precision Medicine FINAL REPORT Prepared by: Audacious Inquiry on behalf of the Office of the National Coordinator for Health Information Technology under Contract No. HHSM-500-2017-000101 Task Order No. HHSP23320100013U January 2021 ONC Advancing Standards for Precision Medicine Table of Contents Executive Summary ...................................................................................................................................... 5 Standards Development and Demonstration Projects ............................................................................ 5 Mobile Health, Sensors, and Wearables ........................................................................................... 5 Social Determinants of Health (SDOH) ............................................................................................. 5 Findings and Lessons Learned .......................................................................................................... 6 Recommendations ........................................................................................................................................ 6 Introduction ................................................................................................................................................... 7 Background ................................................................................................................................................... 7 Project Purpose, Goals, and Objectives .................................................................................................. -
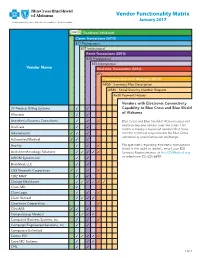
Vendor Functionality Matrix January 2017 an Independent Licensee of the Blue Cross and Blue Shield Association
Vendor Functionality Matrix January 2017 An Independent Licensee of the Blue Cross and Blue Shield Association Readiness Validated Claims Transactions (5010) 837 Professional 837 Institutional Remit Transactions (5010) 835 Professional 835 Institutional Vendor Name Real-time Transactions (5010) 27x Proprietary Real-time Messages (5010) AB50 - Summary Plan Description AB80 - Social Security Number Request Ax20 Payment History Vendors with Electronic Connectivity 2K Medical Billing Systems 3 3 Capability to Blue Cross and Blue Shield of Alabama Allscripts 3 3 Anesthesia Business Consultants 3 3 3 Blue Cross and Blue Shield of Alabama does not endorse any one vendor over the other. This AnviCare 3 3 matrix is merely a record of vendors that have Athenahealth 3 3 3 met the technical requirements for Blue Cross connectivity and information exchange. Automated Medical 3 3 3 Availity 3 3 3 For questions regarding electronic transactions listed in the table to the left, email your EDI Avid Anesthesiology Solutions 3 3 3 3 3 Services Representative at [email protected] AXIOM Systems Inc. 3 3 or telephone 205-220-6899. BrickMed, LLC 3 3 C&S Research Corporation 3 3 3 3 CBIZ MMP 3 3 Change Healthcare 3 3 3 3 3 3 Claim.MD 3 ClaimLogic 3 3 3 Claim Remedi 3 3 3 3 Clearwave Corporation 3 ClinixMIS 3 3 3 CompuGroup Medical 3 3 3 3 Compulink Business Systems, Inc. 3 3 3 Computer Engineered Solutions, Inc. 3 3 Computers Unlimited Cortex EDI 3 3 3 3 3 Cove MD Systems 3 3 3 CPU 3 3 1 of 4 Readiness Validated Claims Transactions (5010) 837 Professional 837 Institutional Remit Transactions (5010) 835 Professional 835 Institutional Vendor Name Real-time Transactions (5010) 27x Proprietary Real-time Messages (5010) AB50 - Summary Plan Description AB80 - Social Security Number Request Ax20 Payment History Creative Concepts in Communications 3 3 Custom Software Systems, Inc. -

Top 20 Ehr Software
TOP 20 EHR SOFTWARE C M CONVERTED MEDIA TOP 20 EHR SOFTWARE 1 AdvancedMD AdvancedEHR 11 Allscripts Allscripts Professional EHR 2 Cerner Cerner Ambulatory EHR 12 CareCloud CareCloud Charts 3 athenahealth athenahealth EHR 13 CureMD All in One EHR 4 Epic Epic EHR 14 Practice Velocity VelociDoc EHR Azalea Health 5 Practice Fusion Practice Fusion EHR 15 Azalea EHR Innovations 6 Kareo Kareo Clinical 16 ReLi Med Solutions ReLiMed EMR 7 Henry Schein MicroMD EMR 17 MedEZ MedEZ 8 drchrono drchrono EHR 18 iSALUS Healthcare OfficeEMR 9 NextGen Healthcare NextGen Healthcare EHR 19 ChartLogic ChartLogic EMR Modernizing 10 EMA 20 ICANotes ICANotes EHR Medicine C M CONVERTED MEDIA EHR IN PRACTICE HOW THESE RANKINGS WERE GENERATED This ranking was determined using a number of factors including industry standing, public opinion of software, social media presence, and available software features relevant to the needs of a small business. This ranking should serve as a rough estimate of software suitability, and more in-depth analysis can be taken below or by using our EHR software comparison. C M CONVERTED MEDIA SHORTLISTING EHR VENDORS CHECKLIST Research EHR employed by similar sized practices in 1 6 Produce an RFI document and send to vendor shortlist the same specialty Identify market leading solutions which offer some 2 7 Narrow shortlist based on RFI responses support in your specialty Leverage professional network for recommendations Compile requirements and business processes in an 3 8 based on their experience RFP document Narrow shortlist based -

CONFERENCE PROGRAM November 15–17, 2016, Boston, MA
CONFERENCE PROGRAM November 15–17, 2016, Boston, MA CONFERENCE PROGRAM | MESSAGE President and Chair’s Message Dear Colleague: “What we need is a national conversation of experts,” Mark Levin, Partner, Third Rock Ventures, once told the audience at the Annual Personalized Medicine Conference. “Across the industry, across government, the best people in this country to come together to tell us how to maximize value for patients. That is the big challenge in our future.” The 12th Annual Personalized Medicine Conference responds to Levin’s call to action with a concentrated focus on generating solutions to the field’s challenges. It will showcase what is new, offer insights into the issues, and provide partnership and networking opportunities for attendees. But most importantly, it will examine the unique contributions that researchers, investors, industry representatives, policy experts, payers, health care providers and patients can make at each stage in the development of personalized medicine products and services to forge a path through the field’s barriers. The conference program, which is organized around those stages, will go beyond defining personalized medicine’s challenges by, for example: ¢ Exploring the latest trends in research and development ¢ Analyzing the issues facing the diagnostic industry ¢ Finding commonalities in multiple definitions of “value” in health care ¢ Providing examples of the kinds of evidence appropriate for coverage and payment ¢ Examining the best practices for integrating personalized medicine into clinical settings ¢ Debating the circumstances that warrant the sharing of data for research We are pleased to present the entire conference program here, which covers these and many other topics. Sincerely yours, Edward Abrahams, Ph.D. -

Cerner, Athenahealth and Veeva Chase Cloudbased
9/18/2015 Cerner, Athenahealth And Veeva Chase Cloud-Based EHR - NASDAQ.com Cerner, Athenahealth And Veeva Chase CloudBased EHR By Investor's Business Daily, January 23, 2015, 04:55:00 PM EDT A new wrinkle in federal rules this year aims to urge more hospitals and other medical providers into the 21st century. Those expectations have helped lift a handful of companies in IBD's Computer SoftwareMedical group, a group at the intersection of health care and Internet technology and key suppliers to the health industry's conversion from paper to digital electronic records.Cerner ( CERN ),Athenahealth ( ATHN ) andVeeva Systems ( VEEV ) are at the head of that list. All three have seen benefits from the American Recovery and Reinvestment Act of 2009, also known as the stimulus bill. All have also seen their share of recent ups and downs. The initial bill set aside $19 billion to help health care providers convert their patient records systems from paper to digital, or electronic health records. As of Dec. 1, the Centers for Medicare and Medicaid Services Pinterest reported the program had paid more than $25.7 billion to participants, including hospitals, doctors and insurance companies, meeting "meaningful use" requirements. Tumblr Email Print Beginning this year, the government will ratchet up the pressure by trimming reimbursements to medical Gmail providers not yet converted to EHR systems, or converts that are falling short of the meaningfuluse Favorites benchmarks set out by the stimulus bill. More... (293) Nearly 80% of physicians and hospitals are already using EHRs or plan to start soon, according to data from AddThis the federal government and industry research groups. -

Small Practice Ambulatory Emr/Pm (10 Or Fewer Physicians) 2019
SMALL PRACTICE AMBULATORY EMR/PM (10 OR FEWER PHYSICIANS) 2019 BUILDING STRONG FOUNDATIONS FOR CUSTOMER SUCCESS ® %/ Performance Report | January 2019 DRILL DEEPER TABLE OF CONTENTS 2 Executive Insights 6 Expanded Insights 29 Vendor Insights 31 AdvancedMD 45 eClinicalWorks 33 Allscripts 47 eMDs 35 Aprima 49 Greenway Health 37 athenahealth 51 Kareo 39 CareCloud 53 NextGen Healthcare 41 Cerner 55 Virence Health (GE Healthcare) 43 CureMD 57 Data Index 68 Vendor Executive Interview Details 1 EXECUTIVE INSIGHTS SMALL PRACTICE AMBULATORY EMR/PM (10 OR FEWER PHYSICIANS) 2019 BUILDING STRONG FOUNDATIONS FOR CUSTOMER SUCCESS As healthcare has moved beyond meaningful use, small practices have begun to expect more from their vendors and to look for EMRs that do more than meet basic regulatory requirements. As a result, EMR/PM satisfaction among small practices (10 or fewer physicians) has varied greatly over the past year—scores for a number of vendors have swung more than 10 percentage points (some positively, some negatively). To explore what the future holds for this market, KLAS spoke to hundreds of small practice customers about their EMR/PM experiences and needs and also interviewed executives and representatives from AdvancedMD, Allscripts, Aprima, athenahealth, Azalea Health, CareCloud, Cerner, CureMD, eMDs, Greenway Health, Kareo, NextGen, Quest Diagnostics, and Virence Health (GE Healthcare) to find out how these vendors plan to increase customer satisfaction going forward. What Are the Most Important Vendor/ NextGen Healthcare, CureMD, and Aprima Product Attributes for Small Practices? Most Aligned to Deliver Customer Success (n=57) The green bars represent the total tallies after New 7 Technology each need was weighted When asked to name the top things EMR/PM vendors should focus based on whether the respondent ranked it first, on, small practices overwhelmingly say that before addressing more Advanced Needs second, or third. -

Top Integrated Electronic Health Records Physician Practice Management & Billing Vendors
BLACK BOOK RANKINGS 2014 USER SURVEY Top Integrated Electronic Health Records Physician Practice Management & Billing Vendors Publication Date: May 2014 Electronic Health Records Ambulatory Practice Management Software Solutions Outsourced Revenue Cycle Management Services BLACK BOOK™ TOP INTEGRATED PRACTICE MANAGEMENT & REVENUE CYCLE MANAGEMENT EHR SOFTWARE VENDORS May 2014 ©2014 Black Book Rankings LLC. This report is a licensed product. Do not duplicate or distribute without permission. Page 1 2014 Black Book Integrated Practice Management – Revenue Cycle Management EHR Software Top Vendors Report Black Book™ annually evaluates leading health care/medical software and service providers across 18 operational excellence key performance indicators completely from the perspective of the client experience. Independent and unbiased from vendor influence, more than 380,000 healthcare IT users are invited to contribute to various annual customer satisfaction polls. Suppliers also encourage their clients to participate to produce current and objective customer service data for buyers, analysts, investors, consultants, competitive suppliers and the media. For more information or to order customized research results, please contact the Client Resource Center at +1 727.953.3355 or [email protected] © 2014, 2013 Black Book Rankings LLC All Rights Reserved. Reproduction of this publication in any form without prior written permission is forbidden. The information contained herein has been obtained from sources believed to be reliable. Brown-Wilson Group, Inc. the parent corporation of Black Book™, Black Book Rankings LLC, Black Book Market Research LLC, and The Black Book of Outsourcing®, disclaims all warranties as to the accuracy, completeness or adequacy of such information. Brown-Wilson Group shall have no liability for errors, omissions or inadequacies in the information contained herein or for interpretations thereof. -

Spring 2019 Medical Practice Management
SPRING 20CUSTOMER SUCCESS 19REPORT MEDICAL PRACTICE MANAGEMENT SOFTWARE CATEGORY MEDICAL PRACTICE MANAGEMENT SOFTWARE OVERVIEW Medical practice management software (PMS) is designed to assist medical offices of all sizes operate more efficiently. Mostly, small and medium-size practices utilize a PMS to manage daily administrative and financial functions, and integrate it with electronic medical records The capabilities of PMS include: entering and monitoring patients, storing patient demographics, scheduling patient appointments, handling charge capture, executing billing procedures, presenting insurance claims, processing payments from third parties, insurance providers, and patients, and producing reports for employees. Medical PMS can be used to store and maintain patient records as well as manage large data sets, including details of physicians and other health care providers, medical facilities, insurance companies, procedures, and ICD codes. 2 CUSTOMER SUCCESS Company Score is affected by the following: SCORING METHODOLOGY 1. Number of employees (based on social media and public resources) The FeaturedCustomers.com Customer 2. Vendor momentum based on web traffic and Success score is based on data from our search trends customer success content platform, social 3. Employee satisfaction and engagement presence, as well as additional data aggregated (based on social network ratings) from online sources and social media properties. 4. % traffic increase to your Customer Our ranking engine applies an algorithm to all of References the data collected to calculate the overall 5. Lower Funnel SEO Key Term Rankings Customer Success score. The overall Customer Success score is a weighted average based on 3 CUSTOMER SUCCESS AWARDS parts: Market Leader (90 - 100) Content Score is affected by the following: Vendor on FeaturedCustomers.com 1. -

EHR to EHR Conversions When, Why &
EHR to EHR Conversions When, Why & How Navigating EHR Mergers, Acquisitions and Dissatisfactions Presented by: Jeffery Daigrepont, Senior Vice President | Coker Group [email protected] | 770-597-0590 Agenda . Current State of the Market . Navigating EHR Mergers & Acquisitions – Merging practices/hospitals of different EHRs . Navigating EHR Dissatisfaction . Future Proofing HCIT Investments . Summary 2 Current State of the Market 3 EMR Market for Hospitals- Top Companies . Athena Health (Aquired RazorInsights and Harvards WebOMR) . Allscripts (Eclipsys, end of life) . Cerner . CPSI . Epic Systems . eClinicalWorks (Ambulatory Only, but popular bolt-on) . GE Healthcare . HCS EMR . Healthcare Management Systems . Healthland (Now CPIS) . McKesson . Meditech . NextGen (Discontinued inpatient) . Quadramed . Prognosis . RazorInsights (Now Athena) . Siemens Medical (Now Cerner) Source: http://www.healthcareitnews.com/news/black-book-names-best-best-ehrs 4 The Market Size (Buyers) Hospitals 11% CAHs 49% Community IDNs 41% Approximately 5000 hospitals 5 CDC EHR Adoption Stats… . In 2015, 78% of office-based physicians used any type of electronic health record (EHR) system, up from 18% in 2001. In 2015, 48% of office-based physicians reported having a system that met the criteria for a basic system, up from 11% in 2006. In 2015, 69% of office-based physicians reported that they intended to participate (i.e., they planned to apply or already had applied) in "meaningful use" incentives. From 2010 (the earliest year that trend data are available) -

Epic Interoperability
INTEROPERABILITY WHITE PAPER Epic Interoperability Interoperability—the ability of different information technology systems and software applications to communicate, exchange data, and use the information that has been exchanged1—helps to provide comprehensive patient information in an electronic health record. Epic enables the secure flow of patient data between Epic sites and between Epic and other vendors’ systems. We accomplish this in three ways: 1) Care Everywhere, Epic’s patient record exchange platform 2) interfaces, and 3) application programming interfaces (APIs). Source: “EMR Interoperability 2014”, KLAS Enterprises, September 2014 Patient record exchange between healthcare organizations Care Everywhere is Epic’s standards-based patient record exchange platform and uses the Consolidated Clinical Document Architecture (C-CDA) as required for Meaningful Use Stage 2 certification.2 Epic installed Care Everywhere in all versions of its EpicCare EHR software in use so that 100% of customers who are live with EpicCare also have the ability to exchange patient records. Care Everywhere is available to 436,726 providers at over 1,183 hospitals and 33,989 clinics. These organizations cover a patient population of approximately 183 million—over 56.5% of the U.S. population. 1 HIMSS Dictionary of Healthcare Information Technology Terms, Acronyms and Organizations, 2nd Edition, 2010 2 Full Meaningful Use Stage 2 certification details are available at http://www.epic.com/software-certification.php © Epic. All Rights Reserved. October 2016 INTEROPERABILITY WHITE PAPER Organizations using Care Everywhere make up the largest EHR-based exchange group in the United States3, exchanging 1.25 million patient records a day with each other and with over 10,000 other organizations.4 This includes healthcare providers using other EHR systems, Health Information Service Providers, Health Information Exchanges, and entities connected to the eHealth Exchange like the VA, the Social Security Administration and the DoD. -
Clinical Integration Through Electronic Data Interchange
VENDOR LIST Clinical Integration Through Electronic Data Interchange As of February 2021 As of February 2021 Vendor Name Vendor Name Vendor Name 4Medica CareHere-Champ IT Solutions DaVinci Technology Accumedic Computer Systems CareSpan USA Inc DaVita ACE Health Solutions, LLC Cascades Clinical Systems, Inc. DavLong Business Solutions, LLC Acumen Physician Solutions Centura Health Corporate DigiDMS Acurus Solutions Cerner Corp Digital MD Systems ADL Data Systems Cerner PowerChart DocComply Advanced Data Systems Corp Change Healthcare Doctor On Demand Advanced Technologies Group ChartLogic Doc-tor.com AdvancedMD Software ChartPerfect, Inc DoctorWellington Agastha ChenMed DocuTrac Ageology, Inc. ChiroTouch Dr J Exceptional Medicine AllegianceMD Software Inc ClaimPower, Inc. DrChrono AllMeds, Inc ClinicTracker JAG Drscribe Allscripts Clinlab DrugPak LLC American Medical Software Clovi Echo Group American Medical Solutions CoCENTRIX eClinicalWorks Anagen Systems CodoniX eData Platform Angel Systems, Inc. Community Computer Service, Inc. EHealthLine.com, Inc. Ankhos Oncology Software, LLC Complete Healthcare Solutions, Inc eHealthObjects, Inc AntWorks Complete Medical Solutions, Inc. EHR Your Way AP Easy Software Solutions CompuGroup Medical Elation Health Apex Energetics CompuLink Business Systems ELEKTA IMPAC Medical Systems Apex Healthware Computalogic Ellkay Aprima Comtron eMD Office.com Aragon Development Conceptual Mindworks eMDs Arise Lab, LLC Confluence Health Systems LLC eMedical Fusion Artisan Medical Solutions Connexin Software, Inc eMedicalNotes ASP.MD Core Solutions Emedpractice Aspyra Inc. CorEMR Empower Health Services, LLC Athena Health Cority Enable Healthcare Inc. AtlasMD CorrecTek EnableDoc Axion Health Credible Behavioral Health Software Encite Azalea Health Innovations, Inc. Criterions Ensoftek, Inc. AZZLY Crowell Systems Epic Systems Corporation BestNotes CureMD Essential Health Solutions BIZMATICS, Inc Custom Computing Corp Evident Brilogy CyberMed, LLC. -

Clinical Integration Through Electronic Data Interchange
VENDOR LIST Clinical Integration Through Electronic Data Interchange As of July 2021 As of July 2021 Vendor Name Vendor Name Vendor Name 4Medica CareCloud DataLink LLC Accumedic Computer Systems CareHere-Champ IT Solutions DataTel Solutions ACE Health Solutions, LLC CareSpan USA Inc DaVinci Technology Acumen Physician Solutions Cascades Clinical Systems, Inc. DaVita Acurus Solutions Centura Health Corporate DavLong Business Solutions, LLC ADL Data Systems Cerner Corp DigiDMS Advanced Data Systems Corp Change Healthcare Digital MD Systems Advanced Technologies Group ChartLogic DocComply AdvancedMD Software ChartPerfect, Inc Doctor On Demand Agastha ChenMed DoctorWellington Ageology, Inc. ChiroTouch DocuTrac AllegianceMD Software Inc ClaimPower, Inc. Dr J Exceptional Medicine AllMeds, Inc ClinicTracker JAG DrChrono Allscripts Clinlab Drscribe American Medical Software Clovi DrugPak LLC American Medical Solutions CoCENTRIX Echo Group Anagen Systems CodoniX eClinicalWorks Angel Systems, Inc. Community Computer Service, Inc. eData Platform Ankhos Oncology Software, LLC Complete Healthcare Solutions, Inc EHealthLine.com, Inc. AntWorks Complete Medical Solutions, Inc. eHealthObjects, Inc AP Easy Software Solutions CompuGroup Medical EHR Your Way Apex Energetics CompuLink Business Systems Elation Health Apex Healthware Computalogic ELEKTA IMPAC Medical Systems Aprima Computer Service & Support Ellkay Aragon Development Comtron eMD Office.com Arise Lab, LLC Conceptual Mindworks eMDs Artisan Medical Solutions Confluence Health Systems LLC eMedical