Intravenous Techniques in Ambulatory Anesthesia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Federal Register/Vol. 85, No. 36/Monday, February 24, 2020
10466 Federal Register / Vol. 85, No. 36 / Monday, February 24, 2020 / Notices Controlled substance Drug code Schedule Alphamethadol ................................................................................................................................................................. 9605 I Benzethidine .................................................................................................................................................................... 9606 I Betacetylmethadol ........................................................................................................................................................... 9607 I Clonitazene ...................................................................................................................................................................... 9612 I Diampromide ................................................................................................................................................................... 9615 I Diethylthiambutene .......................................................................................................................................................... 9616 I Dimethylthiambutene ....................................................................................................................................................... 9619 I Ketobemidone ................................................................................................................................................................. -

ESTIMATED WORLD REQUIREMENTS of NARCOTIC DRUGS in GRAMS for 2019 (As of 10 January 2019 )
ESTIMATED WORLD REQUIREMENTS OF NARCOTIC DRUGS IN GRAMS FOR 2019 (as of 10 January 2019 ) Afghanistan Cannabis 50 Codeine 50 000 Cannabis resin 1 Dextropropoxyphene 10 000 Coca leaf 1 Diphenoxylate 5 000 Cocaine 15 Fentanyl 1 Codeine 650 000 Methadone 20 000 Codeine -N-oxide 1 Morphine 8 000 Dextromoramide 1 Pethidine 90 000 Dextropropoxyphene 200 000 Pholcodine 40 000 Difenoxin 1 Albania Dihydrocodeine 1 Cocaine 1 Diphenoxylate 1 Codeine 1 189 000 Dipipanone 1 Fentanyl 300 Ecgonine 2 Heroin 1 Ethylmorphine 1 Methadone 7 000 Etorphine 1 Morphine 7 800 Fentanyl 17 000 Oxycodone 2 000 Heroin 1 Pethidine 2 700 Hydrocodone 10 000 Pholcodine 1 500 Hydromorphone 4 000 Remifentanil 9 Ketobemidone 1 Sufentanil 2 Levorphanol 1 Algeria Methadone 100 000 Alfentanil 350 Morphine 1 550 000 Codeine 2 500 000 Morphine -N-oxide 1 Etorphine 1 Nicomorphine 1 Fentanyl 500 Norcodeine 1 Methadone 4 000 Normethadone 1 Morphine 9 000 Normorphine 1 Oxycodone 4 000 Opium 10 Pethidine 3 000 Oripavine 1 Pholcodine 1 500 000 Oxycodone 60 000 Remifentanil 1 Oxymorphone 1 Sufentanil 30 Pethidine 50 000 Andorra Phenoperidine 1 Cannabis 2 000 Pholcodine 1 Fentanyl 100 Piritramide 1 Methadone 1 000 Remifentanil 20 000 Morphine 500 Sufentanil 10 Oxycodone 2 000 Thebacon 1 Pethidine 500 Thebaine 70 000 Remifentanil 4 Tilidine 1 Angola Armenia Alfentanil 20 Codeine 3 000 Codeine 21 600 Fentanyl 40 Dextromoramide 188 Methadone 13 500 Dextropropoxyphene 200 Morphine 7 500 Dihydrocodeine 500 Thebaine 15 Diphenoxylate 300 Trimeperidine 1 500 Fentanyl 63 Aruba* Methadone 2 000 -
Data Driven Investigation of Bispectral Index Algorithm
www.nature.com/scientificreports OPEN Data Driven Investigation of Bispectral Index Algorithm Hyung-Chul Lee, Ho-Geol Ryu, Yoonsang Park , Soo Bin Yoon, Seong Mi Yang, Hye-Won Oh & Chul-Woo Jung Received: 7 January 2019 Bispectral index (BIS), a useful marker of anaesthetic depth, is calculated by a statistical multivariate Accepted: 9 September 2019 model using nonlinear functions of electroencephalography-based subparameters. However, only Published: xx xx xxxx a portion of the proprietary algorithm has been identifed. We investigated the BIS algorithm using clinical big data and machine learning techniques. Retrospective data from 5,427 patients who underwent BIS monitoring during general anaesthesia were used, of which 80% and 20% were used as training datasets and test datasets, respectively. A histogram of data points was plotted to defne fve BIS ranges representing the depth of anaesthesia. Decision tree analysis was performed to determine the electroencephalography subparameters and their thresholds for classifying fve BIS ranges. Random sample consensus regression analyses were performed using the subparameters to derive multiple linear regression models of BIS calculation in fve BIS ranges. The performance of the decision tree and regression models was externally validated with positive predictive value and median absolute error, respectively. A four-level depth decision tree was built with four subparameters such as burst suppression ratio, power of electromyogram, 95% spectral edge frequency, and relative beta ratio. Positive predictive values were 100%, 80%, 80%, 85% and 89% in the order of increasing BIS in the fve BIS ranges. The average of median absolute errors of regression models was 4.1 as BIS value. -

A Review of Unique Opioids and Their Conversions
A Review of Unique Opioids and Their Conversions Jacqueline Cleary, PharmD, BCACP Assistant Professor Albany College of Pharmacy and Health Sciences Adjunct Professor SAGE College of Nursing DISCLOSURES • Kaleo • Remitigate, LLC OBJECTIVES • Compare and contrast unique pharmacotherapy options for the treatment of chronic pain including: methadone, buprenoprhine, tapentadol, and tramadol • Select methadone, buprenorphine, tapentadol, or tramadol based on patient specific factors • Apply appropriate opioid conversion strategies to unique opioids • Understand opioid overdose risk surrounding opioid conversions and the use of unique opioids UNIQUE OPIOIDS METHADONE, BUPRENORPHINE, TRAMADOL, TAPENTADOL METHADONE My favorite drug because….? METHADONE- INDICATIONS • FDA labeled indications – (1) chronic pain (2) detoxification Oral soluble tablets for suspension NOT indicated for chronic pain treatment • Initial inpatient detoxification of opioids by a licensed trained provider with methadone and supportive care is appropriate • Methadone maintenance provider must have special credentialing and training as required by state Outpatient prescription must be for pain ONLY and say “for pain” on RX • Continuation of methadone maintenance from outside provider while patient is inpatient for another condition is appropriate http://cdn.atforum.com/wp-content/uploads/SAMHSA-2015-Guidelines-for-OTPs.pdf MECHANISM OF ACTION • Potent µ-opioid agonist • NMDA receptor antagonist • Norepinephrine reuptake inhibitor • Serotonin reuptake inhibitor ADVERSE EVENTS -

Nerve Blocks for Surgery on the Shoulder, Arm Or Hand
Nerve blocks for surgery on the shoulder, arm or hand Information for patients and families First Edition 2015 www.rcoa.ac.uk/patientinfo Nerve blocks for surgery on the shoulder, arm or hand This leaflet is for anyone who is thinking about having a nerve block for an operation on the shoulder, arm or hand. It will be of particular interest to people who would prefer not to have a general anaesthetic. The leaflet has been written with the help of patients who have had a nerve block for their operation. Throughout this leaflet we have used the above symbol to highlight key facts. Brachial plexus block? The brachial plexus is the group of nerves that lies between your neck and your armpit. It contains all the nerves that supply movement and feeling to your arm – from your shoulder to your fingertips. A brachial plexus block is an injection of local anaesthetic around the brachial plexus. It ‘blocks’ information travelling along these nerves. It is a type of nerve block. Your arm becomes numb and immobile. You can then have your operation without feeling anything. The block can also provide excellent pain relief for between three and 24 hours, depending on what kind of local anaesthetic is used. A brachial plexus block rarely affects the rest of the body so it is particularly advantageous for patients who have medical conditions which put them at a higher risk for a general anaesthetic. A brachial plexus block may be combined with a general anaesthetic or with sedation. This means you have the advantage of the pain relief provided by a brachial plexus block, but you are also unconscious or sedated during the operation. -

Determination of Barbiturates and 11-Nor-9-Carboxy-Δ9-THC in Urine
Determination of Barbiturates and 11-Nor-9-carboxy- 9-THC in Urine using Automated Disposable Pipette Extraction (DPX) and LC/MS/MS Fred D. Foster, Oscar G. Cabrices, John R. Stuff, Edward A. Pfannkoch GERSTEL, Inc., 701 Digital Dr. Suite J, Linthicum, MD 21090, USA William E. Brewer Department of Chemistry and Biochemistry, University of South Carolina, 631 Sumter St. Columbia, SC 29208, USA KEYWORDS DPX, LC/MS/MS, Sample Preparation, High Throughput Lab Automation ABSTRACT This work demonstrates the use of disposable pipette extraction (DPX) as a fast and automated sample preparation technique for the determination of barbiturates and 11-nor-9- carboxy- 9-THC (COOH-THC) in urine. Using a GERSTEL MultiPurpose Sampler (MPS) with DPX option coupled to an Agilent 6460 LC-MS/MS instrument, 8 barbiturates and COOH-THC were extracted and their concentrations determined. The resulting average cycle time of 7 min/ sample, including just-in-time sample preparation, enabled high throughput screening. Validation results show that the automated DPX-LC/ AppNote 1/2013 MS/MS screening method provides adequate sensitivity for all analytes and corresponding internal standards that were monitored. Lower limits of quantitation (LLOQ) were found to be 100 ng/mL for the barbiturates and 10 ng/mL for COOH-THC and % CVs were below 10 % in most cases. INTRODUCTION The continuously growing quantity of pain management sample extract for injection [1-2]. The extraction of the drugs used has increased the demand from toxicology Barbiturates and COOH-THC is based on the DPX-RP- laboratories for more reliable solutions to monitor S extraction method described in an earlier Application compliance in connection with substance abuse and/or Note detailing monitoring of 49 Pain Management diversion. -

Recommended Methods for the Identification and Analysis of Fentanyl and Its Analogues in Biological Specimens
Recommended methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Recommended Methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES UNITED NATIONS Vienna, 2017 Note Operating and experimental conditions are reproduced from the original reference materials, including unpublished methods, validated and used in selected national laboratories as per the list of references. A number of alternative conditions and substitution of named commercial products may provide comparable results in many cases. However, any modification has to be validated before it is integrated into laboratory routines. ST/NAR/53 Original language: English © United Nations, November 2017. All rights reserved. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. Mention of names of firms and commercial products does not imply the endorse- ment of the United Nations. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. Acknowledgements The Laboratory and Scientific Section of the UNODC (LSS, headed by Dr. Justice Tettey) wishes to express its appreciation and thanks to Dr. Barry Logan, Center for Forensic Science Research and Education, at the Fredric Rieders Family Founda- tion and NMS Labs, United States; Amanda L.A. -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group. -

Nerve Injury After Peripheral Nerve Block: Allbest Rights Practices Reserved
PRINTER-FRIENDLY VERSION AVAILABLE AT ANESTHESIOLOGYNEWS.COM Nerve Injury After Peripheral Nerve Block: AllBest rights Practices reserved. Reproduction and Medical-Legal in whole or in part without Protection permission isStrategies prohibited. Copyright © 2015 McMahon Publishing Group unless otherwise noted. DAVID HARDMAN, MD, MBA Professor of Anesthesiology Vice Chair for Professional Affairs Department of Anesthesiology University of North Carolina at Chapel Hill Chapel Hill, North Carolina Dr. Hardman reports no relevant financial conflicts of interest. he risk for permanent or severe nerve injury after peripheral nerve blocks (PNBs) is Textremely low, irrespective of its etiology (ie, related to anesthesia, surgery or the patient). The risk inherent in a procedure should always be explicitly discussed with the patient (sidebar, page 4). In fact, it may be better to define this phenomenon ultrasound-guided axillary blocks were used, demon- as postoperative neurologic symptoms (PONS) or peri- strated a very low nerve injury rate of 0.0037% at hos- operative nerve injuries (PNI) in order to help stan- pital discharge.1-7 dardize terminology. Permanent injury rates, as defined A 2009 prospective case series involving more than by a neurologic abnormality present at or beyond 12 7,000 PNBs, conducted in Australia and New Zealand, months after the procedure, have consistently ranged demonstrated that when a postoperative neurologic from 0.029% to 0.2%, although the results of a recent symptom was diagnosed, it was 9 times more likely to multicenter Web-based survey in France, in which be due to a non–anesthesia-related cause than a nerve ANESTHESIOLOGY NEWS • JULY 2015 1 block–related cause.6 On the other hand, it is well doc- PNI rate of 1.7% in patients who received a single-injec- umented in the orthopedic and anesthesia literature tion interscalene block (ISB). -
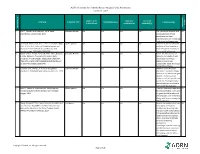
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table SAMPLE SIZE/ CONTROL/ OUTCOME CITATION EVIDENCE TYPE INTERVENTION(S) CONCLUSION(S) POPULATION COMPARISON MEASURE(S) SCORE CONSENSUS REFERENCE # REFERENCE 1 Lirk P., Picardi S. and Hollmann, M. W. Local Literature Review n/a n/a n/a n/a The mechanism of action and VA anaesthetics: 10 essentials. 2014 access pathways of local anesthetics and their pharmokinetics are increasingly understood and appreciated. 2 Calatayud, Jesús, M.D.,D.D.S., Ph.D., González, Õngel, Expert Opinion n/a n/a n/a n/a A review of the discovery and VA M.D., D.D.S., Ph.D. History of the development and evolution of local anesthesia evolution of local anesthesia since the coca leaf. from the Spanish discovery of Anesthesiology. 2003;98(6):1503-1508. the coca leaf in America. 3 Gordh T, M.D., Gordh, Torsten E.,M.D., Ph.D., Lindqvist Literature Review n/a n/a n/a n/a Before the introduction of VA K, M.Sc. Lidocaine: The origin of a modern local lidocaine, the choice of local anesthetic. Anesthesiology. 2010;113(6):1433-1437. anesthetics was limited. https://doi.org/10.1097/ALN.0b013e3181fcef48. doi: Lidocaine's onset was 10.1097/ALN.0b013e3181fcef48. substantially faster and longer lasting than procaine. 4 Volcheck G.W., Mertes, P. M. Local and general Literature Review n/a n/a n/a n/a Whether to test the local VA anesthetics immediate hypersensitivity reactions. 2014 anesthetic causing the allergic reaction or an alternative agent depends on the expected future need of the specific local anesthetic. -

The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures
Volume 2- Issue 1 : 2018 DOI: 10.26717/BJSTR.2018.02.000695 Eduardo de Oliveira Duque-Estrada. Biomed J Sci & Tech Res ISSN: 2574-1241 Mini Review Open Access The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures Eduardo de Oliveira Duque-Estrada MD* Received: January 17, 2018; Published: January 25, 2018 *Corresponding author: Eduardo de Oliveira Duque-Estrada, Ex-Professor of Pediatrics and Pediatric Surgery, Teresópolis Schoolof Medicine, Rio de Janeiro, Rua Jose da Silva Ribeiro 119 apt 11 São Paulo, SP Brazil CEP: 05726-130, Email: Abstract The local anesthetics are widely u sed in minor pediatric surgical procedures. The major problem with their use is the resulted pain experienced by the patients at the time of injection. To discuss those situations in the light of the medical literature we present this mini-review. Key words: Local Injection; Pain; Buffer; pH; Lidocaine; Pediatric Surgery Procedure Introduction Table 1: Techniques for injection pain control*. a eutectic mixture of lidocaine and prilocaine (EMLA) cream [17] S.No Techniques for injection pain control before infiltration, and local external cooling (cryoanalgesia) have 1. Warming the anesthetic solution [18,19] (Table 1). also been used to reduce the pain of infiltration of local anesthetic 2. Buffering the anesthetic Buffering the Anesthetic 3. Injection technique 4. Distraction Local anesthesia is extremely useful either as the sole method the best results on the minor surgery in general [3,6]. Blocking 5. Combination anesthetic technique the pain pathway with local anesthetic solution will also reduce 6. Cooling of skin the family stress response to the surgical procedure. -

Nerve Blocks for Surgery on the Shoulder, Arm Or Hand
The Association of Regional The Royal College of Anaesthetists of Great Anaesthesia – Anaesthetists Britain and Ireland United Kingdom Nerve blocks for surgery on the shoulder, arm or hand Information for patients and families www.rcoa.ac.uk/patientinfo First edition 2015 This leaflet is for anyone who is thinking about having a nerve block for an operation on the shoulder, arm or hand. It will be of particular interest to people who would prefer not to have a general anaesthetic. The leaflet has been written with the help of patients who have had a nerve block for their operation. You can find more information leaflets on the website www.rcoa.ac.uk/patientinfo. The leaflets may also be available from the anaesthetic department or pre-assessment clinic in your hospital. The website includes the following: ■ Anaesthesia explained (a more detailed booklet). ■ You and your anaesthetic (a shorter summary). ■ Your spinal anaesthetic. ■ Anaesthetic choices for hip or knee replacement. ■ Epidural pain relief after surgery. ■ Local anaesthesia for your eye operation. ■ Your child’s general anaesthetic. ■ Your anaesthetic for major surgery with planned high dependency care afterwards. ■ Your anaesthetic for a broken hip. Risks associated with your anaesthetic This is a collection of 14 articles about specific risks associated with having an anaesthetic or an anaesthetic procedure. It supplements the patient information leaflets listed above and is available on the website: www.rcoa.ac.uk/patients-and-relatives/risks. Throughout this leaflet and others in the series, we have used this symbol to highlight key facts. 2 NERVE BLOCKS FOR SURGERY ON THE SHOULDER, ARM OR HAND Brachial plexus block? The brachial plexus is the group of nerves that lies between your neck and your armpit.