A Review of Unique Opioids and Their Conversions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Perioperative Opioid-Sparing Analgesia Strategies for Enhanced Recovery After Surgery
Perioperative Opioid-Sparing Analgesia Strategies for Enhanced Recovery After Surgery T. Anthony Anderson, MD PhD Associate Professor Department of Anesthesiology, Perioperative and Pain Medicine Lucile Packard Children's Hospital Stanford Stanford University School of Medicine International Society for Anaesthetic Pharmacology 2018 Annual Meeting Disclosures • I have no relevant relationships to disclose Learning Objectives After this lecture, the listener should be able to: • Identify risks associated with the perioperative use of opioids • Determine opioid-sparing systemic pharmacologic analgesics options • Organize a perioperative analgesic plan to decrease postoperative pain, reduce opioid use, hasten recovery, and improve patient safety Paradigm Shift Surgical Considerations Optimize Co-Morbidities Baseline Pain & Opioid Use Regional techniques Non-pharmacologic Non-opioid Opioids Reasons to Reduce Peri-operative Opioid Use • Relapse risk in patients with a history of opioid use disorder • Improved post-operative recovery • Acute risks • Chronic risks Opioid Use Disorder Relapse • In 2016, 1.8 million people had prescription pain medication use disorder, 5.5% of population • High risk group • Poor evidence for pain management options • Perioperative exposure to relapse triggers: – Stress – Agent of abuse Ward EN, Quaye AN, Wilens TE. Opioid Use Disorders: Perioperative Management of a Special Population. Anesth Analg. 2018 Aug;127(2):539-547. Briand LA, Blendy JA. Molecular and genetic substrates linking stress and addiction. Brain Res. 2010 Feb 16;1314:219-34. ERAS Colorectal Surgery • 13 major perioperative categories • 3 rely heavily on opioid reduction – Multimodal, opioid-sparing pain management – PONV prevention – Ileus reduction • ERAS protocols reduce – Length of hospital stay – Costs – Minor complications Carmichael JC, Keller DS, Baldini G, Bordeianou L, Weiss E, Lee L, Boutros M, McClane J, Feldman LS, Steele SR. -

RELISTOR, INN: Methylnaltrexone Bromide
The European Medicines Agency Evaluation of Medicines for Human Use EMEA/CHMP/10906/2008 ASSESSMENT REPORT FOR RELISTOR International Nonproprietary Name: METHYLNALTREXONE BROMIDE Procedure No. EMEA/H/C/870 Assessment Report as adopted by the CHMP with all information of a commercially confidential nature deleted. 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) 74 18 8613 E-mail: [email protected] http://www.emea.eu.int TABLE OF CONTENTS Page 1 BACKGROUND INFORMATION ON THE PROCEDURE......................................... 3 1.1 Submission of the dossier ...................................................................................................... 3 1.2 Steps taken for the assessment of the product ....................................................................... 3 2 SCIENTIFIC DISCUSSION............................................................................................... 4 2.1 Introduction............................................................................................................................ 4 2.2 Quality aspects....................................................................................................................... 5 2.3 Non-clinical aspects............................................................................................................... 7 2.4 Clinical aspects .................................................................................................................... 13 2.5 Pharmacovigilance...............................................................................................................41 -

Albany-Molecular-Research-Regulatory
PRODUCT CATALOGUE API COMMERCIAL US EU Japan US EU Japan API Name Site CEP India API Name Site CEP India DMF DMF DMF DMF DMF DMF A Abiraterone Malta • Benztropine Mesylate Cedarburg • Adenosine Rozzano - Quinto de' Stampi • • * Betaine Citrate Anhydrous Bon Encontre • Betametasone-17,21- Alcaftadine Spain Spain • • Dipropionate Sterile • Alclometasone-17, 21- Spain Betamethasone Acetate Spain Dipropionate • • Altrenogest Spain • • Betamethasone Base Spain Amphetamine Aspartate Rensselaer Betamethasone Benzoate Spain * Monohydrate Milled • Betamethasone Valerate Amphetamine Sulfate Rensselaer Spain * • Acetate Betamethasone-17,21- Argatroban Rozzano - Quinto de' Stampi Spain • • Dipropionate • • • Atenolol India • • Betamethasone-17-Valerate Spain • • Betamethasone-21- Atracurium Besylate Rozzano - Quinto de' Stampi Spain • Phosphate Disodium Salt • • Bromfenac Monosodium Atropine Sulfate Cedarburg Lodi * • Salt Sesquihydrate • • Azanidazole Lodi Bromocriptine Mesylate Rozzano - Quinto de' Stampi • • • • • Azelastine HCl Rozzano - Quinto de' Stampi • • Budesonide Spain • • Aztreonam Rozzano - Valle Ambrosia • • Budesonide Sterile Spain • • B Bamifylline HCl Bon Encontre • Butorphanol Tartrate Cedarburg • Beclomethasone-17, 21- Spain Capecitabine Lodi Dipropionate • C • 2 *Please contact our Accounts Managers in case you are interested in this API. 3 PRODUCT CATALOGUE API COMMERCIAL US EU Japan US EU Japan API Name Site CEP India API Name Site CEP India DMF DMF DMF DMF DMF DMF Dexamethasone-17,21- Carbimazole Bon Encontre Spain • Dipropionate -

Original Article Anesthetic Effect of Propofol Combined with Remifentanil and Propofol Combined with Ketamine in Ophthalmic Surgery
Int J Clin Exp Med 2019;12(7):9387-9392 www.ijcem.com /ISSN:1940-5901/IJCEM0079428 Original Article Anesthetic effect of propofol combined with remifentanil and propofol combined with ketamine in ophthalmic surgery Xiaofeng Yi1*, Yanbing Zhang1*, Limin Jin1, Xinjing Yang2 Departments of 1Anesthesia Surgery, 2Emergency ICU, First Affiliated Hospital of Soochow University, Suzhou 215000, Jiangsu, China. *Equal contributors. Received May 10, 2018; Accepted December 7, 2018; Epub July 15, 2019; Published July 30, 2019 Abstract: Propofol combined with ketamine has been used for anesthesia in the past. Remifentanil presented a good analgesic effect, rapid onset, short half-life, and a high clearance rate. Propofol combined with remifentanil also shows good effects in the clinic. This study compared the effect and safety of propofol combined remifentanil and propofol combined ketamine in pediatric eye surgery. Pediatric patients that received eye surgery in our hospital were selected and randomly divided into two groups, the experimental group (n=30), in which patients received pro- pofol combined with remifentanil anesthesia and control group (n=30), and the group receiving propofol combined with ketamine anesthesia. The curative effect, FCO2, SPO2, MAP, HR, anesthesia complications, operation time, recovery time, and leaving PACU time were compared. The rate of good anesthesia was 93.33% in the experimental group, which was significantly higher than control (P < 0.05). FCO2 at 2 and 5 minutes after anesthesia, preopera- tive, intraoperative, and postoperative elevated, while SPO2, MAP, and HR decreased (P < 0.05). The experimen- tal group showed smaller fluctuation range than the control. The rate of Nausea (6.67%), vomiting (3.33%), and somnolence (10%) in the experimental group was significantly lower than control (P < 0.05). -

Federal Register/Vol. 85, No. 36/Monday, February 24, 2020
10466 Federal Register / Vol. 85, No. 36 / Monday, February 24, 2020 / Notices Controlled substance Drug code Schedule Alphamethadol ................................................................................................................................................................. 9605 I Benzethidine .................................................................................................................................................................... 9606 I Betacetylmethadol ........................................................................................................................................................... 9607 I Clonitazene ...................................................................................................................................................................... 9612 I Diampromide ................................................................................................................................................................... 9615 I Diethylthiambutene .......................................................................................................................................................... 9616 I Dimethylthiambutene ....................................................................................................................................................... 9619 I Ketobemidone ................................................................................................................................................................. -

Design and Synthesis of Cyclic Analogs of the Kappa Opioid Receptor Antagonist Arodyn
Design and synthesis of cyclic analogs of the kappa opioid receptor antagonist arodyn By © 2018 Solomon Aguta Gisemba Submitted to the graduate degree program in Medicinal Chemistry and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. Chair: Dr. Blake Peterson Co-Chair: Dr. Jane Aldrich Dr. Michael Rafferty Dr. Teruna Siahaan Dr. Thomas Tolbert Date Defended: 18 April 2018 The dissertation committee for Solomon Aguta Gisemba certifies that this is the approved version of the following dissertation: Design and synthesis of cyclic analogs of the kappa opioid receptor antagonist arodyn Chair: Dr. Blake Peterson Co-Chair: Dr. Jane Aldrich Date Approved: 10 June 2018 ii Abstract Opioid receptors are important therapeutic targets for mood disorders and pain. Kappa opioid receptor (KOR) antagonists have recently shown potential for treating drug addiction and 1,2,3 4 8 depression. Arodyn (Ac[Phe ,Arg ,D-Ala ]Dyn A(1-11)-NH2), an acetylated dynorphin A (Dyn A) analog, has demonstrated potent and selective KOR antagonism, but can be rapidly metabolized by proteases. Cyclization of arodyn could enhance metabolic stability and potentially stabilize the bioactive conformation to give potent and selective analogs. Accordingly, novel cyclization strategies utilizing ring closing metathesis (RCM) were pursued. However, side reactions involving olefin isomerization of O-allyl groups limited the scope of the RCM reactions, and their use to explore structure-activity relationships of aromatic residues. Here we developed synthetic methodology in a model dipeptide study to facilitate RCM involving Tyr(All) residues. Optimized conditions that included microwave heating and the use of isomerization suppressants were applied to the synthesis of cyclic arodyn analogs. -

The Opioid Epidemic: What Labs Have to Do with It?
The Opioid Epidemic: What labs have to do with it? Ewa King, Ph.D. Associate Director of Health RIDOH State Health Laboratories Analysis. Answers. Action. www.aphl.org Overview • Overdose trends • Opioids and their effects • Analytical testing approaches • Toxicology laboratories Analysis. Answers. Action. www.aphl.org Opioid overdose crisis 1 Analysis. Answers. Action. www.aphl.org Opioid overdose crisis 2 Analysis. Answers. Action. www.aphl.org Opiates and Opioids • Opiates vs. Opioids • Opiates: Naturally occurring, derived from the poppy plant • Opioids: “Opiate-like” drugs in effects, not chemical structure Includes opiates • Narcotic analgesics • CNS depressants • DEA Schedule I or II controlled substances • Additive effect with other CNS depressant drugs Analysis. Answers. Action. www.aphl.org Efficacy of Opioids • How do opioids work? • Bind with opioid receptors • Brain, spinal cord, GI tract, and throughout the body • Pain, emotion, breathing, movement, and digestion Opioid Receptor Analysis. Answers. Action. www.aphl.org Effects of Opioids Physiological Psychological • Pain relief • Drowsiness/ sedation • Cough suppression • Mental confusion • GI motility • Loss of memory • Respiratory depression • Lethargy/ apathy • Pupillary constriction • Euphoria/ tranquility • Itching • Mood swings • Constipation • Depression • Dependence • Withdrawal • Dependence Analysis. Answers. Action. www.aphl.org Opiates 1 Opiates • Naturally occurring alkaloids Opium • Latex from the opium poppy plant Codeine: • Mild to moderate pain • Antitussive Morphine: • Severe pain • Metabolite of codeine and heroin Analysis. Answers. Action. www.aphl.org Opiates 2 Semi-synthetic Opiates: • Synthesized from a natural opiate Heroin: • Schedule I narcotic Hydrocodone (Vicodin): • Mild to moderate pain • Metabolizes to hydromorphone (Dilaudid) Oxycodone (Oxycontin/Percocet): • Moderate to severe pain • Metabolizes to oxymorphone (Opana) Analysis. Answers. Action. -

ESTIMATED WORLD REQUIREMENTS of NARCOTIC DRUGS in GRAMS for 2019 (As of 10 January 2019 )
ESTIMATED WORLD REQUIREMENTS OF NARCOTIC DRUGS IN GRAMS FOR 2019 (as of 10 January 2019 ) Afghanistan Cannabis 50 Codeine 50 000 Cannabis resin 1 Dextropropoxyphene 10 000 Coca leaf 1 Diphenoxylate 5 000 Cocaine 15 Fentanyl 1 Codeine 650 000 Methadone 20 000 Codeine -N-oxide 1 Morphine 8 000 Dextromoramide 1 Pethidine 90 000 Dextropropoxyphene 200 000 Pholcodine 40 000 Difenoxin 1 Albania Dihydrocodeine 1 Cocaine 1 Diphenoxylate 1 Codeine 1 189 000 Dipipanone 1 Fentanyl 300 Ecgonine 2 Heroin 1 Ethylmorphine 1 Methadone 7 000 Etorphine 1 Morphine 7 800 Fentanyl 17 000 Oxycodone 2 000 Heroin 1 Pethidine 2 700 Hydrocodone 10 000 Pholcodine 1 500 Hydromorphone 4 000 Remifentanil 9 Ketobemidone 1 Sufentanil 2 Levorphanol 1 Algeria Methadone 100 000 Alfentanil 350 Morphine 1 550 000 Codeine 2 500 000 Morphine -N-oxide 1 Etorphine 1 Nicomorphine 1 Fentanyl 500 Norcodeine 1 Methadone 4 000 Normethadone 1 Morphine 9 000 Normorphine 1 Oxycodone 4 000 Opium 10 Pethidine 3 000 Oripavine 1 Pholcodine 1 500 000 Oxycodone 60 000 Remifentanil 1 Oxymorphone 1 Sufentanil 30 Pethidine 50 000 Andorra Phenoperidine 1 Cannabis 2 000 Pholcodine 1 Fentanyl 100 Piritramide 1 Methadone 1 000 Remifentanil 20 000 Morphine 500 Sufentanil 10 Oxycodone 2 000 Thebacon 1 Pethidine 500 Thebaine 70 000 Remifentanil 4 Tilidine 1 Angola Armenia Alfentanil 20 Codeine 3 000 Codeine 21 600 Fentanyl 40 Dextromoramide 188 Methadone 13 500 Dextropropoxyphene 200 Morphine 7 500 Dihydrocodeine 500 Thebaine 15 Diphenoxylate 300 Trimeperidine 1 500 Fentanyl 63 Aruba* Methadone 2 000 -

Dezocine Exhibits Antihypersensitivity Activities in Neuropathy Through
www.nature.com/scientificreports OPEN Dezocine exhibits antihypersensitivity activities in neuropathy through spinal Received: 09 November 2016 Accepted: 19 January 2017 μ-opioid receptor activation and Published: 23 February 2017 norepinephrine reuptake inhibition Yong-Xiang Wang1, Xiao-Fang Mao1, Teng-Fei Li1, Nian Gong1 & Ma-Zhong Zhang2 Dezocine is the number one opioid painkiller prescribed and sold in China, occupying 44% of the nation’s opioid analgesics market today and far ahead of the gold-standard morphine. We discovered the mechanisms underlying dezocine antihypersensitivity activity and assessed their implications to antihypersensitivity tolerance. Dezocine, given subcutaneously in spinal nerve-ligated neuropathic rats, time- and dose-dependently produced mechanical antiallodynia and thermal antihyperalgesia, significantly increased ipsilateral spinal norepinephrine and serotonin levels, and induced less antiallodynic tolerance than morphine. Its mechanical antiallodynia was partially (40% or 60%) and completely (100%) attenuated by spinal μ-opioid receptor (MOR) antagonism or norepinephrine depletion/α2-adrenoceptor antagonism and combined antagonism of MORs and α2-adenoceptors, respectively. In contrast, antagonism of spinal κ-opioid receptors (KORs) and δ-opioid receptors (DORs) or depletion of spinal serotonin did not significantly alter dezocine antiallodynia. In addition, dezocine- delayed antiallodynic tolerance was accelerated by spinal norepinephrine depletion/α2-adenoceptor antagonism. Thus dezocine produces antihypersensitivity activity through spinal MOR activation and norepinephrine reuptake inhibition (NRI), but apparently not through spinal KOR and DOR activation, serotonin reuptake inhibition or other mechanisms. Our findings reclassify dezocine as the first analgesic of the recently proposed MOR-NRI, and reveal its potential as an alternative to as well as concurrent use with morphine in treating pain. -

Recommendations for Prescribing Analgesia on Discharge Following Surgery Or Acute Injury Information for Health Practitioners Preparing the Patient for Discharge
Recommendations for prescribing analgesia on discharge following surgery or acute injury Information for health practitioners preparing the patient for discharge better health * better care * better value This booklet ‘Recommendations for prescribing analgesia on discharge following surgery or acute injury: Information for health practitioners preparing the patient for discharge’ is designed to be used in conjunction with the patient booklet titled ‘Pain relief medications following surgery and injury: Information for patients preparing for discharge’. Developed by the Analgesia Management Working Group (AMWG) and made available by the Western Australian Medication Safety Group (WAMSG). For more information on the WAMSG or this booklet go to website www.watag.org.au/wamsg Disclaimer: The information contained in this brochure has been produced as a guide only. It is not intended to be comprehensive and does not take the place of professional medical advice from your doctor, nurse or pharmacist. Contents Background 2 Recommendations for prescribing post-operative analgesia for pain following an acute injury or surgery 4 Precautions when prescribing opioids with other medications 6 Recommendations for prescribing discharge analgesia for pain following an acute injury or surgery 8 Paracetamol 8 Non-Steroidal Anti-inflammatory Drugs (NSAIDs) 8 Opioids 8 Communication to the primary care provider 10 Communication with the patient 10 Appendix 1 – Post-operative and post-intervention analgesia discharge checklist 11 Appendix 2 – Discharge analgesic plan 13 References 14 Recommendations for prescribing analgesia on discharge following surgery or acute injury | 1 Background The WA Medication Safety Group (WAMSG) has identified analgesia management post- surgery or acute injury (specifically managing and ceasing opioids), in the transition period from hospital to home, as a priority safety issue for patients and the community. -

Recommended Methods for the Identification and Analysis of Fentanyl and Its Analogues in Biological Specimens
Recommended methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Recommended Methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES UNITED NATIONS Vienna, 2017 Note Operating and experimental conditions are reproduced from the original reference materials, including unpublished methods, validated and used in selected national laboratories as per the list of references. A number of alternative conditions and substitution of named commercial products may provide comparable results in many cases. However, any modification has to be validated before it is integrated into laboratory routines. ST/NAR/53 Original language: English © United Nations, November 2017. All rights reserved. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. Mention of names of firms and commercial products does not imply the endorse- ment of the United Nations. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. Acknowledgements The Laboratory and Scientific Section of the UNODC (LSS, headed by Dr. Justice Tettey) wishes to express its appreciation and thanks to Dr. Barry Logan, Center for Forensic Science Research and Education, at the Fredric Rieders Family Founda- tion and NMS Labs, United States; Amanda L.A. -
Methylnaltrexone Nonf
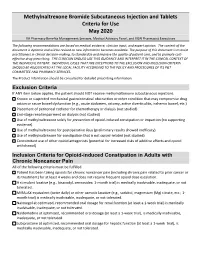
Methylnaltrexone Bromide Subcutaneous Injection and Tablets Criteria for Use May 2020 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The following recommendations are based on medical evidence, clinician input, and expert opinion. The content of the document is dynamic and will be revised as new information becomes available. The purpose of this document is to assist practitioners in clinical decision-making, to standardize and improve the quality of patient care, and to promote cost- effective drug prescribing. THE CLINICIAN SHOULD USE THIS GUIDANCE AND INTERPRET IT IN THE CLINICAL CONTEXT OF THE INDIVIDUAL PATIENT. INDIVIDUAL CASES THAT ARE EXCEPTIONS TO THE EXCLUSION AND INCLUSION CRITERIA SHOULD BE ADJUDICATED AT THE LOCAL FACILITY ACCORDING TO THE POLICY AND PROCEDURES OF ITS P&T COMMITTEE AND PHARMACY SERVICES. The Product Information should be consulted for detailed prescribing information. Exclusion Criteria If ANY item below applies, the patient should NOT receive methylnaltrexone subcutaneous injections. Known or suspected mechanical gastrointestinal obstruction or other condition that may compromise drug action or cause bowel dysfunction (e.g., acute abdomen, ostomy, active diverticulitis, ischemic bowel, etc.) Placement of peritoneal catheter for chemotherapy or dialysis (not studied) End-stage renal impairment on dialysis (not studied) Use of methylnaltrexone solely for prevention of opioid-induced constipation or impaction (no supporting evidence). Use of methylnaltrexone for postoperative ileus (preliminary results showed inefficacy). Use of methylnaltrexone for constipation that is not opioid-related (not studied) Concomitant use of other opioid antagonists (potential for increased risks of additive effects and opioid withdrawal) Inclusion Criteria for Opioid-induced Constipation in Adults with Chronic Noncancer Pain All of the following criteria must be fulfilled.