Racial and Ethnic Disparities in Health Care, Updated 2010
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Local Health Department Internships
Local Public Health Organizations The following links go to pages for employment, volunteering and internships for local public health departments, public health districts and local health units in Texas. A ● Abilene Taylor-County Public Health District ● Addison (City of) Developmental Services Department ● Alamo Heights (City of) ● Alice (City of) Community Development Department ● Allen (City of) Environmental Services ● Amarillo Area Public Health District ● Andrews City-CO Health Department ● Angelina County and Cities Health District ● Aransas County Environmental Health ● Arlington (City of) Environmental Health Division ● Austin Public Health B ● Balcones Heights (City of) Public Health ● Bastrop County Environmental & Sanitation Services ● Baytown Health Department ● Beaumont Public Health Department ● Bee County Health Department ● Beeville (City of) Development Services Department ● Bell County Health Department 1 Texas Health and Human Services ● hhs.texas.gov ● Bellaire (City of) ● Big Lake (City of) ● Blanco County Environmental Services ● Bosque County Courthouse ● Brady (City of) Health Inspector Office ● Brazoria County Health Department ● Brazos County Health Department ● Brown County-City of Brownwood Health Department ● Brownsville (City of) Health Department ● Burleson (City of) Environmental: volunteering, employment ● Burleson County Environmental ● Burnet County Environmental Services C ● Caldwell County Sanitation ● Cameron County Public Health ● Carrollton (City of) Environmental Svcs: volunteering, employment -

Human Service Workers Any People Experience Hardship and Need Help
Helping those in need: Human service workers any people experience hardship and need help. This help is provided by M a network of agencies and organi- zations, both public and private. Staffed by human service workers, this network, and the kinds of help it offers, is as varied as the clients it serves. “Human services tend to be as broad as the needs and problems of the cli- ent base,” says Robert Olding, president of the National Organization for Human Services in Woodstock, Georgia. Human service workers help clients become more self-sufficient. They may do this by helping them learn new skills or by recom- mending resources that allow them to care for themselves or work to overcome setbacks. These workers also help clients who are unable to care for themselves, such as children and the elderly, by coordinating the provision of their basic needs. The first section of this article explains the duties of human service workers and the types of assistance they provide. The next action. Throughout the process, they provide several sections detail the populations served clients with emotional support. by, and the occupations commonly found in, human services. Another section describes Evaluate and plan some benefits and drawbacks to the work, and Working closely with the client, human the section that follows discusses the educa- service workers identify problems and cre- Colleen tion and skills needed to enter human service ate a plan for services to help the client solve Teixeira these problems. This process—which includes occupations. The final section lists sources of Moffat additional information. -
Disparities in Health and Health Care: Five Key Questions and Answers
March 2020 | Issue Brief Disparities in Health and Health Care: Five Key Questions and Answers Samantha Artiga, Kendal Orgera, and Olivia Pham Executive Summary 1. What are health and health care disparities? Health and health care disparities refer to differences in health and health care between groups that are closely linked with social, economic, and/or environmental disadvantage. Disparities occur across many dimensions, including race/ethnicity, socioeconomic status, age, location, gender, disability status, and sexual orientation. 2. Why do health and health care disparities matter? Disparities in health and health care not only affect the groups facing disparities, but also limit overall gains in quality of care and health for the broader population and result in unnecessary costs. Addressing health disparities is increasingly important as the population becomes more diverse. It is projected that people of color will account for over half (52%) of the population in 2050. 3. What is the current status of disparities? Although the Affordable Care Act (ACA) lead to large coverage gains, some groups remain at higher risk of being uninsured, lacking access to care, and experiencing worse health outcomes. For example, as of 2018, Hispanics are two and a half times more likely to be uninsured than Whites (19.0% vs. 7.5%) and individuals with incomes below poverty are four times as likely to lack coverage as those with incomes at 400% of the federal poverty level or above (17.3% vs. 4.3%). 4. What are key initiatives to address disparities? The ACA’s coverage expansions and funding for community health centers increased access to coverage and care for many groups facing disparities, and other provisions explicitly focused on reducing disparities. -

Different Perspectives for Assigning Weights to Determinants of Health
COUNTY HEALTH RANKINGS WORKING PAPER DIFFERENT PERSPECTIVES FOR ASSIGNING WEIGHTS TO DETERMINANTS OF HEALTH Bridget C. Booske Jessica K. Athens David A. Kindig Hyojun Park Patrick L. Remington FEBRUARY 2010 Table of Contents Summary .............................................................................................................................................................. 1 Historical Perspective ........................................................................................................................................ 2 Review of the Literature ................................................................................................................................... 4 Weighting Schemes Used by Other Rankings ............................................................................................... 5 Analytic Approach ............................................................................................................................................. 6 Pragmatic Approach .......................................................................................................................................... 8 References ........................................................................................................................................................... 9 Appendix 1: Weighting in Other Rankings .................................................................................................. 11 Appendix 2: Analysis of 2010 County Health Rankings Dataset ............................................................ -

Security, Disease, Commerce: Ideologies of Postcolonial Global Health Nicholas B
Special Issue: Postcolonial Technoscience ABSTRACT Public health in the United States and Western Europe has long been allied with national security and international commerce. During the 1990s, American virologists and public health experts capitalized on this historical association, arguing that ‘emerging diseases’ presented a threat to American political and economic interests. This paper investigates these arguments, which I call the ‘emerging diseases worldview’, and compares it to colonial-era ideologies of medicine and public health. Three points of comparison are emphasized: the mapping of space and relative importance of territoriality; the increasing emphasis on information and commodity exchange networks; and the transition from metaphors of conversion and a ‘civilizing mission’, to integration and international development. Although colonial and postcolonial ideologies of global health remain deeply intertwined, significant differences are becoming apparent. Keywords emerging diseases, exchange, information, networks, pharmaceuticals, public health Security, Disease, Commerce: Ideologies of Postcolonial Global Health Nicholas B. King In April 2000, the Clinton administration, citing domestic political pres- sure and awareness of an emergent international health threat, formally designated HIV/AIDS a threat to American national security. Earlier that year, a National Intelligence Council (NIC) estimate projected that the disease would reduce human life expectancy in Sub-Saharan Africa by as much as 30 years, and kill as much -
What the Public Thinks About Menatl Health and Mental Illness
What the Public Thinks about Mental Health and ~entaleI1lness A paper presented by Shirley A. Star, Senior Study Director National Opinion Research Center, University of Chicago to the Annual Meeting The National Association for Mental Health, Inc. November 19, 1952 For the past two and a half years, the National Opinion Research Center has been engaged upon a pioneering study of the-American public's thinking in the field of mental health, under the joint sponsorship of the National Association for Mental Health and the National Institute of Mental Health, It is a vast and ambitious project, and I'm afraid that the title which has been assigned to my remarks about .the study is going to prove to be misleading in at least two ways. In the first place, and this must be obvious, both the title given me and the scope of the study cover Ear more ground than I could possibly present in the course of one afternoon. About all I can do today is hit a few of the high spots in public thinking and emphasize beforehand that the study aims to be inclusive. You can pretty well assume that it contains some information on just about any question in the area you might raise, even though I don't refer to many of them. So, as they say in the more enterprising shops--"If you don't see what you want, ask for it," In the second place, and this is more serious, I am in the em- barrassing position of having to stand here this afternoon and honestly- -2- admit that I don1t -know what the public thinks as yet. -

Fundamentals of Public Health Nutrition (3 Credit Hours) Fall: 2018 Delivery Format: E-Learning in Canvas
University of Florida College of Public Health & Health Professions Syllabus PHC 6521: Fundamentals of Public Health Nutrition (3 credit hours) Fall: 2018 Delivery Format: E-Learning in Canvas Instructor Name: Dr. von Castel Room Number: FSHN 227 Phone Number: 352 Email Address: [email protected] *****PLEASE USE THIS NOT CANVAS Office Hours: by appointment via phone,conferences (in canvas) or Lync(Microsoft) Preferred Course Communications: email through ufl.edu Prerequisites None PURPOSE AND OUTCOME Public health nutrition involves the promotion of health through nutrition and the prevention of nutrition related disease in a population. It focuses on improving the food choices, dietary intake, and nutritional status at the community, regional, or national level. The public health nutrition professional works to assess nutritional problems and needs by considering environmental causes, identifying intervention points, developing policies and programs to intervene at those points, implementing the policies or programs, and evaluating the effectiveness of the intervention. Course Overview This course will provide an introduction to Public Health Nutrition and the role of the Public Health Nutrition professional. Emphasis will be on definition, identification and prevention of nutrition related disease, as well as improving health of a population by improving nutrition. Malnutrition will be discussed on a societal, economic, and environmental level. It will include the basics of nutritional biochemistry as it relates to malnutrition of a community and targeted intervention. Finally, it will review existing programs and policies, including strengths, weaknesses and areas for modification or new interventions. Relation to Program Outcomes MPH Competencies covered 1. Monitor health status to identify and solve community health problems 2. -
Core Principles to Reframe Mental and Behavioral Health Policy 2
Getty Images / Maskot Core Principles to Reframe Mental and Behavioral Health Policy January 2021 Historic and modern-day policies rooted in discrimination and oppression have created and widened harmful inequities impacting many communities of color. Effectively and equitably addressing mental health requires intervening at systemic and policy levels to dismantle the structures that produce negative outcomes like generational poverty, intergenerational and cultural trauma, racism, sexism, and ableism. Changing social, economic, and physical environments alongside key mental and behavioral health supports through immediate relief and longer-term fixes impact individual and community mental health and wellbeing. An individual’s mental health is impacted by and informs nearly every aspect of their life, identity, and community. CLASP looks at how one’s social, economic, and physical environment impact individual and community views of mental health and wellbeing. To improve mental health outcomes, we must think about an individual and family’s economic security, family support, and their community’s built environment. CLASP recognizes the influence of intergenerational and cultural trauma on communities and believes that all mental and behavioral health practices should be trauma-informed and healing- centered. Policymakers must significantly reform and reimagine systems that support the wellbeing of people with low incomes. This includes, but is not exclusive to: • Universal health coverage, as noted in our health care principles; • Recognizing -
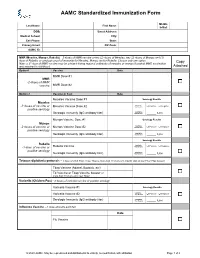
AAMC Standardized Immunization Form
AAMC Standardized Immunization Form Middle Last Name: First Name: Initial: DOB: Street Address: Medical School: City: Cell Phone: State: Primary Email: ZIP Code: AAMC ID: MMR (Measles, Mumps, Rubella) – 2 doses of MMR vaccine or two (2) doses of Measles, two (2) doses of Mumps and (1) dose of Rubella; or serologic proof of immunity for Measles, Mumps and/or Rubella. Choose only one option. Copy Note: a 3rd dose of MMR vaccine may be advised during regional outbreaks of measles or mumps if original MMR vaccination was received in childhood. Attached Option1 Vaccine Date MMR Dose #1 MMR -2 doses of MMR vaccine MMR Dose #2 Option 2 Vaccine or Test Date Measles Vaccine Dose #1 Serology Results Measles Qualitative -2 doses of vaccine or Measles Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Mumps Vaccine Dose #1 Serology Results Mumps Qualitative -2 doses of vaccine or Mumps Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Serology Results Rubella Qualitative Positive Negative -1 dose of vaccine or Rubella Vaccine Titer Results: positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Tetanus-diphtheria-pertussis – 1 dose of adult Tdap; if last Tdap is more than 10 years old, provide date of last Td or Tdap booster Tdap Vaccine (Adacel, Boostrix, etc) Td Vaccine or Tdap Vaccine booster (if more than 10 years since last Tdap) Varicella (Chicken Pox) - 2 doses of varicella vaccine or positive serology Varicella Vaccine #1 Serology Results Qualitative Varicella Vaccine #2 Titer Results: Positive Negative Serologic Immunity (IgG antibody titer) Quantitative Titer Results: _____ IU/ml Influenza Vaccine --1 dose annually each fall Date Flu Vaccine © 2020 AAMC. -

Health Officer Order
NICK MACCHIONE, FACHE HEALTH AND HUMAN SERVICES AGENCY WILMA J. WOOTEN, M.D. AGENCY DIRECTOR PUBLIC HEALTH OFFICER PUBLIC HEALTH SERVICES 3851 ROSECRANS STREET, MAIL STOP P-578 SAN DIEGO, CA 92110-3134 (619) 531-5800 • FAX (619) 542-4186 ORDER OF THE HEALTH OFFICER (Quarantine of Persons Exposed to COVID-19) The spread of coronavirus disease 2019 (COVID-19) is a substantial threat to the public’s health. San Diego County is currently subject to a declared local health emergency and a proclaimed local emergency due to the COVID-19 pandemic, and the Governor of the State of California proclaimed a state of emergency. Everyone is at risk for becoming ill with COVID-19, but some people are more vulnerable to serious illness due to age or underlying health conditions. In order to slow the spread of COVID-19, and prevent the healthcare system in San Diego County from being overwhelmed, it is necessary for the Health Officer of the County of San Diego (Health Officer) to require the quarantine of persons exposed to COVID-19. Household contacts, intimate partners, caregivers, and any other person who have been in close contact with a person either diagnosed with COVID-19, or likely to have COVID-19 (COVID-19 Patient), must quarantine themselves. A “close contact” is a contact with a COVID-19 Patient that occurs anywhere between 48 hours before the COVID-19 Patient’s symptoms began (or, for asymptomatic patients, 2 days prior to test specimen collection), and until the COVID-19 Patient is no longer required to be isolated, and where they: 1. -

COVID-19 Vaccination Requirement (Proclamation 21-14.1) for Health Care Providers, Workers and Settings
Updated September 2021 DOH 505-160 COVID-19 Vaccination Requirement (Proclamation 21-14.1) for health care providers, workers and settings Link to proclamation: 21-14.1 - COVID-19 Vax Washington General Proclamation Questions What does Proclamation 21-14.1 do? Proclamation 21-14.1, issued by Governor Inslee on August 20, 2021, made numerous changes to Proclamation 21-14, issued by Governor Inslee on August 9, 2021, but left the same core requirements in place. As before, the proclamation requires health care providers, defined broadly to include not only licensed health care providers but also all employees, contractors, and volunteers who work in a health care setting, to be fully vaccinated against COVID-19 by October 18, 2021. It also requires operators of health care settings to verify the vaccination status of: a) Every employee, volunteer, and contractor who works in the health care setting, whether or not they are licensed or providing health care services, and b) Every employee, volunteer, and contractor who provides health care services for the health care setting operator. On what legal grounds can this be imposed? In response to the emerging COVID-19 threat, Governor Inslee declared a state of emergency on February 29, 2020, using his broad emergency authority under chapter 43.06 RCW. More specifically, under RCW 43.06.220, after a state of emergency has been declared, the governor may prohibit any activity that they believe should be prohibited to help preserve and maintain life, health, property or the public peace. Under an emergency such as this, the governor’s paramount duty is to protect the health and safety of our communities. -

2021-22 School Year New York State Immunization Requirements for School Entrance/Attendance1
2021-22 School Year New York State Immunization Requirements for School Entrance/Attendance1 NOTES: Children in a prekindergarten setting should be age-appropriately immunized. The number of doses depends on the schedule recommended by the Advisory Committee on Immunization Practices (ACIP). Intervals between doses of vaccine should be in accordance with the ACIP-recommended immunization schedule for persons 0 through 18 years of age. Doses received before the minimum age or intervals are not valid and do not count toward the number of doses listed below. See footnotes for specific information foreach vaccine. Children who are enrolling in grade-less classes should meet the immunization requirements of the grades for which they are age equivalent. Dose requirements MUST be read with the footnotes of this schedule Prekindergarten Kindergarten and Grades Grades Grade Vaccines (Day Care, 1, 2, 3, 4 and 5 6, 7, 8, 9, 10 12 Head Start, and 11 Nursery or Pre-k) Diphtheria and Tetanus 5 doses toxoid-containing vaccine or 4 doses and Pertussis vaccine 4 doses if the 4th dose was received 3 doses (DTaP/DTP/Tdap/Td)2 at 4 years or older or 3 doses if 7 years or older and the series was started at 1 year or older Tetanus and Diphtheria toxoid-containing vaccine Not applicable 1 dose and Pertussis vaccine adolescent booster (Tdap)3 Polio vaccine (IPV/OPV)4 4 doses 3 doses or 3 doses if the 3rd dose was received at 4 years or older Measles, Mumps and 1 dose 2 doses Rubella vaccine (MMR)5 Hepatitis B vaccine6 3 doses 3 doses or 2 doses of adult hepatitis B vaccine (Recombivax) for children who received the doses at least 4 months apart between the ages of 11 through 15 years Varicella (Chickenpox) 1 dose 2 doses vaccine7 Meningococcal conjugate Grades 2 doses vaccine (MenACWY)8 7, 8, 9, 10 or 1 dose Not applicable and 11: if the dose 1 dose was received at 16 years or older Haemophilus influenzae type b conjugate vaccine 1 to 4 doses Not applicable (Hib)9 Pneumococcal Conjugate 1 to 4 doses Not applicable vaccine (PCV)10 Department of Health 1.