Gonadotropin-Releasing Hormone Stimulation Test and Diagnostic Cutoff in Precocious Puberty: a Mini Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Study Protocol and Documented in the Subject Dispensing Log
Protocol Title of trial: A Multicenter, Double-Blind, Randomized, Placebo-Controlled Study Evaluating Three Doses of Subcutaneous Pulsatile GnRH Administered via OmniPod Pump for Ovulation Induction in Female Subjects with Primary Amenorrhea with Hypogonadotropic Hypogonadism NCT number: NCT01976728 Sponsor trial code: 000070 Date: 06 Dec 2017 Gonadorelin Acetate, FE Trial Code: 000070 Date: 06 Dec 2017 999037, FE 999903 E-Protocol Amendment-21975;1.0 No Specified Dosage Form and Strength Supersedes: None Clinical Trial Protocol - Amendment 7 Page 1 of 82 CLINICAL TRIAL PROTOCOL A Multicenter, Double-Blind, Randomized, Placebo-Controlled Study Evaluating Three Doses of Subcutaneous Pulsatile GnRH Administered via OmniPod Pump for Ovulation Induction in Female Subjects with Primary Amenorrhea with Hypogonadotropic Hypogonadism Trial Code 000070 Consolidated Protocol Incorporating Amendments 1-7 IND Number: 22,278 Investigational Medicinal Product: LutrePulse OmniPod Indication: Primary Hypothalamic Amenorrhea Phase: III Name and Address of Sponsor: Ferring International Pharmascience Center U.S., Inc. 100 Interpace Parkway Parsippany, NJ 07054 P: 973-796-1600 F: 973-796-1660 GCP Statement: This trial will be performed in compliance with GCP. The information in this document is confidential and is proprietary to Ferring International Pharmascience Center U.S. or another company within the Ferring Group. It is understood that information in this document shall not be disclosed to any third party, in any form, without prior written consent -
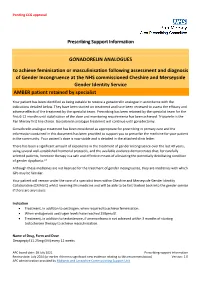
Prescribing Support Information GONADORELIN ANALOGUES To
Pending CCG approval Prescribing Support Information GONADORELIN ANALOGUES to achieve feminisation or masculinisation following assessment and diagnosis of Gender Incongruence at the NHS commissioned Cheshire and Merseyside Gender Identity Service AMBER patient retained by specialist Your patient has been identified as being suitable to receive a gonadorelin analogue in accordance with the indications detailed below. They have been started on treatment and have been reviewed to assess the efficacy and adverse effects of the treatment by the specialist team. Prescribing has been retained by the specialist team for the first 6-12 months until stabilisation of the dose and monitoring requirements has been achieved. Triptorelin is the Pan Mersey first line choice. Gonadorelin analogue treatment will continue until gonadectomy. Gonadorelin analogue treatment has been considered as appropriate for prescribing in primary care and the information contained in this document has been provided to support you to prescribe the medicine for your patient in the community. Your patient’s dose is now stable and is detailed in the attached clinic letter. There has been a significant amount of experience in the treatment of gender incongruence over the last 40 years, using several well-established hormonal protocols, and the available evidence demonstrates that, for carefully selected patients, hormone therapy is a safe and effective means of alleviating the potentially debilitating condition of gender dysphoria.1.2 Although these medicines are not licensed for the treatment of gender incongruence, they are medicines with which GPs may be familiar. Your patient will remain under the care of a specialist team within Cheshire and Merseyside Gender Identity Collaborative (CMAGIC) whilst receiving this medicine and will be able to be fast tracked back into the gender service if there are any issues. -

Hertfordshire Medicines Management Committee (Hmmc) Nafarelin for Endometriosis Amber Initiation – Recommended for Restricted Use
HERTFORDSHIRE MEDICINES MANAGEMENT COMMITTEE (HMMC) NAFARELIN FOR ENDOMETRIOSIS AMBER INITIATION – RECOMMENDED FOR RESTRICTED USE Name: What it is Indication Date Decision NICE / SMC generic decision status Guidance (trade) last revised Nafarelin A potent agonistic The hormonal December Final NICE NG73 2mg/ml analogue of management of 2020 Nasal Spray gonadotrophin endometriosis, (Synarel®) releasing hormone including pain relief and (GnRH) reduction of endometriotic lesions HMMC recommendation: Amber initiation across Hertfordshire (i.e. suitable for primary care prescribing after specialist initiation) as an option in endometriosis Background Information: Gonadorelin analogues (or gonadotrophin-releasing hormone agonists [GnRHas]) include buserelin, goserelin, leuprorelin, nafarelin and triptorelin. The current HMMC decision recommends triptorelin as Decapeptyl SR® injection as the gonadorelin analogue of choice within licensed indications (which include endometriosis) link to decision. A request was made by ENHT to use nafarelin nasal spray as an alternative to triptorelin intramuscular injection during the COVID-19 pandemic. The hospital would provide initial 1 month supply, then GPs would continue for further 5 months as an alternative to the patient attending for further clinic appointments for administration of triptorelin. Previously at ENHT, triptorelin was the only gonadorelin analogue on formulary for gynaecological indications. At WHHT buserelin nasal spray 150mcg/dose is RED (hospital only) for infertility & endometriosis indications. Nafarelin nasal spray 2mg/ml is licensed for: . The hormonal management of endometriosis, including pain relief and reduction of endometriotic lesions. Use in controlled ovarian stimulation programmes prior to in-vitro fertilisation, under the supervision of an infertility specialist. Use of nafarelin in endometriosis aims to induce chronic pituitary desensitisation, which gives a menopause-like state maintained over many months. -

Human Chorionic Gonadotropin (HCG), a Polypeptide Hormone Produced by the Human
45792G/Revised: April 2011 CHORIONIC GONADOTROPIN FOR INJECTION, USP DESCRIPTION: Human chorionic gonadotropin (HCG), a polypeptide hormone produced by the human placenta, is composed of an alpha and a beta sub-unit. The alpha sub-unit is essentially identical to the alpha sub-units of the human pituitary gonadotropins, luteinizing hormone (LH) and follicle-stimulating hormone (FSH), as well as to the alpha sub-unit of human thyroid-stimulating hormone (TSH). The beta sub-units of these hormones differ in amino acid sequence. Chorionic gonadotropin is obtained from the human pregnancy urine. It is standardized by a biological assay procedure. Chorionic Gonadotropin for Injection, USP is available in multiple dose vials containing 10,000 USP Units with accompanying Bacteriostatic Water for Injection for reconstitution. When reconstituted with 10 mL of the accompanying diluent each vial contains: Chorionic gonadotropin 10,000 Units Mannitol 100 mg Benzyl alcohol 0.9% Water for Injection q.s. Buffered with dibasic sodium phosphate and monobasic sodium phosphate. Hydrochloric acid and/or sodium hydroxide may have been used for pH adjustment (6.0 Reference ID: 2933198 8.0). Nitrogen gas is used in the freeze drying process. CLINICAL PHARMACOLOGY: The action of HCG is virtually identical to that of pituitary LH, although HCG appears to have a small degree of FSH activity as well. It stimulates production of gonadal steroid hormones by stimulating the interstitial cells (Leydig cells) of the testis to produce androgens and the corpus luteum of the ovary to produce progesterone. Androgen stimulation in the male leads to the development of secondary sex characteristics and may stimulate testicular descent when no anatomical impediment to descent is present. -

Gonadotropin and Testosterone Measurements After
Pediat. Res. 10: 46-51 (1976) Estradiol puberty estrogen sexual differentiation gonadotropins testosterone maturation Gonadotropin and Testosterone Measurements after Estrogen Administration to Adult Men, Prepubertal and Pubertal Boys, and Men with Hypogonadotropism: Evidence for Maturation of Positive Feedback in the Male HOWARD E. KULIN"" AND EDWARD 0. REITER Reproduction Research Branch, National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland, USA Extract MATERIALS AND METHODS Nineteen male subjects were given five daily injections of SUBJECTS 17~-estradiol and circulating levels of estradiol (E 2 ), testosterone (T), and gonadotropins were determined by radioimmunoassay Seven normal, adult men (ages 20-22) and one male (age 21) before, during, and after the steroid course. Peak levels of E 2 with the syndrome of vanishing testes (I) were hospitalized for attained during the 5 days of treatment ranged from 173-577 pg/ml. study at the Clinical Center of the National Institutes of Health. Four of seven normal adult men and one castrate man demonstrated Each patient was given five daily intramuscular injections of IO or suppression of follicle-stimulating hormone ( FSH) and luteinizing 15 ,ug/kg body weight of 17~-estradiol (E2 ) (20) and blood samples hormone ( LH) with a subsequent rise in LH ( positive feedback) were obtained every 12-24 hr before, during, and after the estrogen while E 2 levels remained elevated. A rise in T was associated with course (see Table I). the LH increment in the four normal men. Nine pre-, early, or Nine endocrinologically normal boys between the ages of 7 and midpubertal boys and two men with hypogonadotropic hypogo 18 were studied in the course of evaluation for short stature, nadism displayed only gonadotropin suppression after E 2 adminis precocious puberty, or delayed adolescence. -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -

Sgnrha-Ovarh-Study-Protocol.Pdf
STUDY PROTOCOL FOR A COMPASSIONATE AQUACULTURE INVESTIGATIONAL NEW ANIMAL DRUG (INAD) EXEMPTION FOR SALMON GONADOTROPIN-RELEASING HORMONE ® ANALOGUE (sGnRHa - OvaRH ) (INAD 012-186) Sponsor: U.S. Fish and Wildlife Service, Division of Fish Hatcheries ______________________ ___________________ Sponsor Signature Date Approved Manufacturer: Western Chemical Inc. 1269 Lattimore Road Ferndale, WA Facility for Coordination of sGnRHa (OvaRH®) INAD: Aquatic Animal Drug Approval Partnership Program 4050 Bridger Canyon Road Bozeman, Mt 59715 Proposed Starting Date September 1, 2012 Proposed Ending Date August 31, 2017 Study Director Mr. Jim Bowker _________________________ ________________ Study Director Signature Date Clinical Field Trial Location and Trial Number: __________________________________________ _________________ Type or Print Facility Name Trial Number Investigator______________________________________________________ Type or Print Name __________________________________________ _________________ Investigator Signature Date I. STUDY ID AND TITLE .................................................................................................................................. 1 II. SPONSOR..................................................................................................................................................... 1 III. INVESTIGATORS/FACILITIES .................................................................................................................... 2 IV. PROPOSED STARTING AND COMPLETION DATES: ........................................................................ -

Chorionic Gonadotropin Human (C0684)
Chorionic gonadotropin human Product Number C 0684 Storage Temperature -0 °C Product Description When hCG was used in combination with recombinant CAS Number: 9002-61-3 interferon-γ, there was a significant cooperative pI = 2.951 induction of nitric oxide synthesis (iNOS) in a dose- Extinction Coefficient: E1% = 3.88 (278nm)2 dependent manner in mouse peritoneal macrophages Synonym: Choriogonin, hCG suggesting that hCG may provide a second signal for synergistic induction of NO synthesis.9 The molecular weight is approximately 37.9 kDa (with approximately 31% carbohydrate by weight). The Precautions and Disclaimer theoretical molecular weight is 37.9 kDa based on the For Laboratory Use Only. Not for drug, household or native form, which contains 2 subunits. The α subunit other uses. has a molecular weight of 14.9 kDa of which approximately 10.2 kDa is for the polypeptide and Preparation Instructions approximately 4.7 kDa for the carbohydrate. The hCG is soluble in water and aqueous buffers such β subunit has a molecular weight of 23 kDa of which phosphate buffer. hCG is also soluble in aqueous approximately 16.0 kDa is for the polypeptide and glycerol and glycols and is insoluble in ethanol.1 approximately 7.0 kDa is for the carbohydrate.3,4,5 Solutions should be sterile filtered and not autoclaved. Product Number C 0684 is sterile filtered and contains Storage/Stability approximately 1,000 I.U. per vial. Dilute aqueous solutions undergo rapid loss of activity when stored frozen, or heated, or if excess acid or hCG is a glycoprotein hormone produced by the base is added. -

Advanced Prostate Cancer: Developing Gonadotropin- Releasing Hormone Analogues Guidance for Industry
Advanced Prostate Cancer: Developing Gonadotropin- Releasing Hormone Analogues Guidance for Industry DRAFT GUIDANCE This guidance document is being distributed for comment purposes only. Comments and suggestions regarding this draft document should be submitted within 90 days of publication in the Federal Register of the notice announcing the availability of the draft guidance. Submit electronic comments to https://www.regulations.gov. Submit written comments to the Dockets Management Staff (HFA-305), Food and Drug Administration, 5630 Fishers Lane, Rm. 1061, Rockville, MD 20852. All comments should be identified with the docket number listed in the notice of availability that publishes in the Federal Register. For questions regarding this draft document, contact Elaine Chang at 240-402-2628. U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) July 2019 Clinical/Medical Advanced Prostate Cancer: Developing Gonadotropin- Releasing Hormone Analogues Guidance for Industry Additional copies are available from: Office of Communications, Division of Drug Information Center for Drug Evaluation and Research Food and Drug Administration 10001 New Hampshire Ave., Hillandale Bldg., 4th Floor Silver Spring, MD 20993-0002 Phone: 855-543-3784 or 301-796-3400; Fax: 301-431-6353; Email: [email protected] https://www.fda.gov/drugs/guidance-compliance-regulatory-information/guidances-drugs U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation -

WSAVA List of Essential Medicines for Cats and Dogs
The World Small Animal Veterinary Association (WSAVA) List of Essential Medicines for Cats and Dogs Version 1; January 20th, 2020 Members of the WSAVA Therapeutic Guidelines Group (TGG) Steagall PV, Pelligand L, Page SW, Bourgeois M, Weese S, Manigot G, Dublin D, Ferreira JP, Guardabassi L © 2020 WSAVA All Rights Reserved Contents Background ................................................................................................................................... 2 Definition ...................................................................................................................................... 2 Using the List of Essential Medicines ............................................................................................ 2 Criteria for selection of essential medicines ................................................................................. 3 Anaesthetic, analgesic, sedative and emergency drugs ............................................................... 4 Antimicrobial drugs ....................................................................................................................... 7 Antibacterial and antiprotozoal drugs ....................................................................................... 7 Systemic administration ........................................................................................................ 7 Topical administration ........................................................................................................... 9 Antifungal drugs ..................................................................................................................... -

The Effect of Gonadotropin Withdrawal and Stimulation with Human Chorionic Gonadotropin on Intratesticular Androstenedione and DHEA in Normal Men
ORIGINAL ARTICLE Endocrine Research The Effect of Gonadotropin Withdrawal and Stimulation with Human Chorionic Gonadotropin on Intratesticular Androstenedione and DHEA in Normal Men M. Y. Roth, S. T. Page, K. Lin, B. D. Anawalt, A. M. Matsumoto, B. Marck, W. J. Bremner, and J. K. Amory Downloaded from https://academic.oup.com/jcem/article/96/4/1175/2720870 by guest on 02 October 2021 Departments of Internal Medicine (M.Y.R., S.T.P., B.D.A., A.M.M., W.J.B., J.K.A.) and Obstetrics and Gynecology (K.L.) and Center for Research in Reproduction and Contraception (M.Y.R., S.T.P., B.D.A., A.M.M., W.J.B., J.K.A.), University of Washington, Seattle, Washington 91895; and Geriatric Research (B.M.), Education and Clinical Center, Veterans Affairs Puget Sound Health Care System, Seattle, Washington 98105 Introduction: Concentrations of intratesticular (IT) testosterone (T) are known to be 100–200 times those of serum T; however, the IT concentrations of T’s precursors, their testicular to serum gra- dients, gonadotropin dependence, and response to stimulation with human chorionic gonado- tropin (hCG) have not been studied in detail. We hypothesized that serum and IT androstenedione (ADD) and IT dehydroepiandrosterone (DHEA) would be significantly suppressed by the adminis- tration of a GnRH antagonist and increased when stimulated by hCG, without a similar suppression of serum DHEA. Methods: We suppressed gonadotropins in 23 normal men with the GnRH antagonist acyline and randomly assigned them to one of four doses of hCG, 0, 15, 60, or 125 IU sc every other day for 10 d. -

(12) United States Patent (10) Patent No.: US 6,235,712 B1 Stevenson Et Al
US006235.712B1 (12) United States Patent (10) Patent No.: US 6,235,712 B1 Stevenson et al. (45) Date of Patent: May 22, 2001 (54) NON-AQUEOUS POLARAPROTIC PEPTIDE Helm, et al., “Stability of Gonadorelin and Triptorelin in FORMULATIONS Aqueous Solution”, Pharm. Res., 7/12, pp. 1253-1256 (1990). (75) Inventors: Cynthia L. Stevenson; Steven J. Johnson, et al., “Degradation of the LH-RHAnalog Nafare Prestrelski, both of Mountain View, CA lin Acetate in Aqueous Solution”, Intl. J. Pharm., 31, pp. (US) 125-129 (1986). 73) Assignee:9. ALZA Corporation,p Mountain View, Lupron (leuprolide acetate for Subcutaneous injection), Phy CA (US) sician's Desk Ref, 50th Ed., pp. 2555-2556 (1996). Lupron Depot (leuprolide acetate for depot Suspension), * ) Notice: Subject to anyy disclaimer, the term of this Physician's Desk Ref, 50th Ed., pp. 2556-2562 (1996). patent is extended or adjusted under 35 Lutrepulse (gonadorelin acetate for IV injection), Physi U.S.C. 154(b) by 0 days. cian's Desk Ref, 50th Ed., pp.980–982 (1996). Okada, et al., “New Degradation Product of (21) Appl. No.: 09/514,951 Des-Gly'-NH-LH-RH-Ethylamide (Fertirelin) in Aque (22) Filed: Feb. 28, 2000 ous Solution”, J. Pharm. Sci., 80/2, pp. 167–170 (1991). Okada, et al., “Preparation of Three-Month Depot Injectable Related U.S. Application Data MicroSpheres of Leuprorelin Acetate Using Biodegradable Polymers”, Pharm. Res., 11/8, pp. 1143–1147 (1994). (62) Division of application No. 09/293,839, filed on Apr. 19, 1999, now Pat. No. 6,124,261, which is a continuation of Oyler, et al., “Characterization of the Solution Degradation application No.