Bartonella Infection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Distribution of Tick-Borne Diseases in China Xian-Bo Wu1, Ren-Hua Na2, Shan-Shan Wei2, Jin-Song Zhu3 and Hong-Juan Peng2*
Wu et al. Parasites & Vectors 2013, 6:119 http://www.parasitesandvectors.com/content/6/1/119 REVIEW Open Access Distribution of tick-borne diseases in China Xian-Bo Wu1, Ren-Hua Na2, Shan-Shan Wei2, Jin-Song Zhu3 and Hong-Juan Peng2* Abstract As an important contributor to vector-borne diseases in China, in recent years, tick-borne diseases have attracted much attention because of their increasing incidence and consequent significant harm to livestock and human health. The most commonly observed human tick-borne diseases in China include Lyme borreliosis (known as Lyme disease in China), tick-borne encephalitis (known as Forest encephalitis in China), Crimean-Congo hemorrhagic fever (known as Xinjiang hemorrhagic fever in China), Q-fever, tularemia and North-Asia tick-borne spotted fever. In recent years, some emerging tick-borne diseases, such as human monocytic ehrlichiosis, human granulocytic anaplasmosis, and a novel bunyavirus infection, have been reported frequently in China. Other tick-borne diseases that are not as frequently reported in China include Colorado fever, oriental spotted fever and piroplasmosis. Detailed information regarding the history, characteristics, and current epidemic status of these human tick-borne diseases in China will be reviewed in this paper. It is clear that greater efforts in government management and research are required for the prevention, control, diagnosis, and treatment of tick-borne diseases, as well as for the control of ticks, in order to decrease the tick-borne disease burden in China. Keywords: Ticks, Tick-borne diseases, Epidemic, China Review (Table 1) [2,4]. Continuous reports of emerging tick-borne Ticks can carry and transmit viruses, bacteria, rickettsia, disease cases in Shandong, Henan, Hebei, Anhui, and spirochetes, protozoans, Chlamydia, Mycoplasma,Bartonia other provinces demonstrate the rise of these diseases bodies, and nematodes [1,2]. -
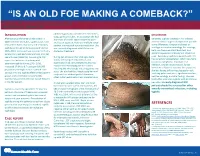
If Needed You Can Use Two Lines
“IS AN OLD FOE MAKING A COMEBACK?” •Eyob Tadesse MD1; Samie Meskele MD1; Ankoor Biswas MD1 •Aurora Health Care, Milwaukee WI. NTRODUCTION abdomen gradually spread to her extremities, DISCUSSION I scalp, palms and soles. In association she had After being on the verge of elimination in shortness of breath, vague abdominal pain Generally, syphilis presents in HIV infected 2000 in the United States, syphilis cases have and loss of appetite, history of multiple sexual patients similar to general population yet with rebounded. Rates of primary and secondary partner, unprotected sex and prostitution. She some differences. Diagnosis is based on syphilis continued to increase overall during was recently diagnosed with HIV but not serologic test and microbiology. For serology, 2005–2013. Increases have occurred primarily started on treatment. both non treponemal antibody test, and among men, and particularly among men has specific treponemal antibody test should be used. Secondary syphilis in patients with HIV sex with men (MSM)(1). According to CDC During her admission her vital signs were has varied skin presentation, which can mimic report the incidence of primary and stable, she had pale conjunctivae, skin cutaneous lymphoma, mycobacterial secondary syphilis during 2015–2016, examination had demonstrated widespread macular and maculopapular skin lesions infection, bacillary angiomatosis, fungal increased 17.6% to 8.7 cases per 100,000 infections or Kaposi’s sarcoma. In our patient, population, the highest rate reported since involving the whole body including palms and soles. She also had thin, fragile scalp hair and she was having diffuse maculopapular rash, 1993(2). HIV and syphilis affect similar patient scalp hair loss without genital ulceration; involving palms and soles, significant hair loss, groups and co-infection is common(3). -

HIV and the SKIN • Sudden Acute Exacerbations • Treatment Failure DR
2018/08/13 KEY FEATURES • Atypical presentation of common disorders • Severe or exaggerated presentations HIV AND THE SKIN • Sudden acute exacerbations • Treatment failure DR. FREDAH MALEKA DERMATOLOGY UNIVERSITY OF PRETORIA:KALAFONG VIRAL INFECTIONS EXANTHEM OF PRIMARY HIV INFECTION • Exanthem of primary HIV infection • Acute retroviral syndrome • Herpes simplex virus (HSV) • Morbilliform rash (exanthem) : 2-4 weeks after HIV exposure • Varicella Zoster virus (VZV) • Typically generalised • Molluscum contagiosum (Poxvirus) • Pronounced on face and trunk, sparing distal extremities • Human papillomavirus (HPV) • Associated : fever, lymphadenopathy, pharyngitis • Epstein Barr virus (EBV) • DDX: drug reaction • Cytomegalovirus (CMV) • other viral infections – EBV, Enteroviruses, Hepatitis B virus 1 2018/08/13 HERPES SIMPLEX VIRUS(HSV) • Vesicular eruption due to HSV 1&2 • Primary lesion: painful, grouped vesicles on an erythematous base • HIV: attacks are more frequent and severe • : chronic, non-healing, deep ulcers, with scarring and tissue destruction • CLUE: severe pain and recurrences • DDX: syphilis, chancroid, lymphogranuloma venereum • Tzanck smear, Histology, Viral culture HSV • Treatment: Acyclovir 400mg tds 7-10 days • Alternatives: Valacyclovir and Famciclovir • In setting of treatment failure, viral isolates tested for resistance against acyclovir • Alternative drugs: Foscarnet, Cidofovir • Chronic suppressive therapy ( >8 attacks per year) 2 2018/08/13 VARICELLA • Chickenpox • Presents with erythematous papules and umbilicated -

Coxiella Burnetii
SENTINEL LEVEL CLINICAL LABORATORY GUIDELINES FOR SUSPECTED AGENTS OF BIOTERRORISM AND EMERGING INFECTIOUS DISEASES Coxiella burnetii American Society for Microbiology (ASM) Revised March 2016 For latest revision, see web site below: https://www.asm.org/Articles/Policy/Laboratory-Response-Network-LRN-Sentinel-Level-C ASM Subject Matter Expert: David Welch, Ph.D. Medical Microbiology Consulting Dallas, TX [email protected] ASM Sentinel Laboratory Protocol Working Group APHL Advisory Committee Vickie Baselski, Ph.D. Barbara Robinson-Dunn, Ph.D. Patricia Blevins, MPH University of Tennessee at Department of Clinical San Antonio Metro Health Memphis Pathology District Laboratory Memphis, TN Beaumont Health System [email protected] [email protected] Royal Oak, MI BRobinson- Erin Bowles David Craft, Ph.D. [email protected] Wisconsin State Laboratory of Penn State Milton S. Hershey Hygiene Medical Center Michael A. Saubolle, Ph.D. [email protected] Hershey, PA Banner Health System [email protected] Phoenix, AZ Christopher Chadwick, MS [email protected] Association of Public Health Peter H. Gilligan, Ph.D. m Laboratories University of North Carolina [email protected] Hospitals/ Susan L. Shiflett Clinical Microbiology and Michigan Department of Mary DeMartino, BS, Immunology Labs Community Health MT(ASCP)SM Chapel Hill, NC Lansing, MI State Hygienic Laboratory at the [email protected] [email protected] University of Iowa [email protected] Larry Gray, Ph.D. Alice Weissfeld, Ph.D. TriHealth Laboratories and Microbiology Specialists Inc. Harvey Holmes, PhD University of Cincinnati College Houston, TX Centers for Disease Control and of Medicine [email protected] Prevention Cincinnati, OH om [email protected] [email protected] David Welch, Ph.D. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Rheumatic Manifestations of Bartonella Infection in 2 Children MOHAMMAD J
Case Report Rheumatic Manifestations of Bartonella Infection in 2 Children MOHAMMAD J. AL-MATAR, ROSS E. PETTY, DAVID A. CABRAL, LORI B. TUCKER, BANAFSHI PEYVANDI, JULIE PRENDIVILLE, JACK FORBES, ROBYN CAIRNS, and RALPH ROTHSTEIN ABSTRACT. We describe 2 patients with very unusual rheumatological presentations presumably caused by Bartonella infection: one had myositis of proximal thigh muscles bilaterally, and the other had arthritis and skin nodules. Both patients had very high levels of antibody to Bartonella that decreased in asso- ciation with clinical improvement. Bartonella infection should be considered in the differential diag- nosis of unusual myositis or arthritis in children. (J Rheumatol 2002;29:184–6) Key Indexing Terms: MYOSITIS ARTHRITIS BARTONELLA Infection with Bartonella species has a wide range of mani- was slightly increased at 9.86 IU/l (normal 4.51–9.16), and IgA was 2.1 IU/l festations in children including cat scratch disease (regional (normal 0.2–1.0). C3 was 0.11 g/l (normal 0.77–1.43) and C4 was 0.28 (nor- mal 0.07–0.40). Antinuclear antibodies were present at a titer of 1:40, the anti- granulomatous lymphadenitis), bacillary angiomatosis, streptolysin O titer was 35 (normal < 200), and the anti-DNAase B titer was encephalitis, Parinaud’s oculoglandular syndrome, Trench 1:85 (normal). Urinalysis showed 50–100 erythrocytes and 5–10 leukocytes fever (Vincent’s angina), osteomyelitis, granulomatous per high power field. Routine cultures of urine, blood, and throat were nega- hepatitis, splenitis, pneumonitis, endocarditis, and fever of tive. Liver enzymes, electrolytes, HIV serology, cerebrospinal fluid analysis, unknown origin1-3. -

An Important One Health Opportunity
veterinary sciences Review Ehrlichioses: An Important One Health Opportunity Tais B. Saito * and David H. Walker Department of Pathology, University of Texas Medical Branch at Galveston, Galveston, TX 77555, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-1409-772-4813 Academic Editor: Ulrike Munderloh Received: 15 July 2016; Accepted: 25 August 2016; Published: 31 August 2016 Abstract: Ehrlichioses are caused by obligately intracellular bacteria that are maintained subclinically in a persistently infected vertebrate host and a tick vector. The most severe life-threatening illnesses, such as human monocytotropic ehrlichiosis and heartwater, occur in incidental hosts. Ehrlichia have a developmental cycle involving an infectious, nonreplicating, dense core cell and a noninfectious, replicating reticulate cell. Ehrlichiae secrete proteins that bind to host cytoplasmic proteins and nuclear chromatin, manipulating the host cell environment to their advantage. Severe disease in immunocompetent hosts is mediated in large part by immunologic and inflammatory mechanisms, including overproduction of tumor necrosis factor α (TNF-α), which is produced by CD8 T lymphocytes, and interleukin-10 (IL-10). Immune components that contribute to control of ehrlichial infection include CD4 and CD8 T cells, natural killer (NK) cells, interferon-γ (IFN-γ), IL-12, and antibodies. Some immune components, such as TNF-α, perforin, and CD8 T cells, play both pathogenic and protective roles. In contrast with the immunocompetent host, which may die with few detectable organisms owing to the overly strong immune response, immunodeficient hosts die with overwhelming infection and large quantities of organisms in the tissues. Vaccine development is challenging because of antigenic diversity of E. -

The Difference in Clinical Characteristics Between Acute Q Fever and Scrub Typhus in Southern Taiwan
International Journal of Infectious Diseases (2009) 13, 387—393 http://intl.elsevierhealth.com/journals/ijid The difference in clinical characteristics between acute Q fever and scrub typhus in southern Taiwan Chung-Hsu Lai a,b, Chun-Kai Huang a, Hui-Ching Weng c, Hsing-Chun Chung a, Shiou-Haur Liang a, Jiun-Nong Lin a,b, Chih-Wen Lin d, Chuan-Yuan Hsu d, Hsi-Hsun Lin a,* a Division of Infectious Diseases, Department of Internal Medicine, E-Da Hospital/I-Shou University, 1 E-Da Road, Jiau-Shu Tsuen, Yan-Chau Shiang, Kaohsiung County, 824 Taiwan, Republic of China b Graduate Institute of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung County, Taiwan, Republic of China c Department of Health Management, I-Shou University, Kaohsiung County, Taiwan, Republic of China d Section of Gastroenterology, Department of Internal Medicine, E-Da Hospital/I-Shou University, Kaohsiung County, Taiwan, Republic of China Received 14 April 2008; received in revised form 17 July 2008; accepted 29 July 2008 Corresponding Editor: Craig Lee, Ottawa, Canada KEYWORDS Summary Acute Q fever; Objective: To identify the differences in clinical characteristics between acute Q fever and scrub Coxiella burnetii; typhus in southern Taiwan. Scrub typhus; Methods: A prospective observational study was conducted in which serological tests for acute Q Orientia tsutsugamushi; fever and scrub typhus were performed simultaneously regardless of which disease was suspected Clinical characteristics; clinically. From April 2004 to December 2007, 80 and 40 cases of serologically confirmed acute Q Taiwan fever and scrub typhus, respectively, were identified and included in the study for comparison. -

Assessment of Coxiella Burnetii Presence After Tick Bite in North‑Eastern Poland
Infection (2020) 48:85–90 https://doi.org/10.1007/s15010-019-01355-w ORIGINAL PAPER Assessment of Coxiella burnetii presence after tick bite in north‑eastern Poland Karol Borawski1 · Justyna Dunaj1 · Piotr Czupryna1 · Sławomir Pancewicz1 · Renata Świerzbińska1 · Agnieszka Żebrowska2 · Anna Moniuszko‑Malinowska1 Received: 12 June 2019 / Accepted: 4 September 2019 / Published online: 14 September 2019 © The Author(s) 2019 Abstract Purpose The aim of the study is to assess anti-Coxiella burnetii antibodies presence in inhabitants of north-eastern Poland, to assess the risk of Q fever after tick bite and to assess the percentage of co-infection with other pathogens. Methods The serological study included 164 foresters and farmers with a history of tick bite. The molecular study included 540 patients, hospitalized because of various symptoms after tick bite. The control group consisted of 20 honorary blood donors. Anti-Coxiella burnetii antibodies titers were determined by Coxiella burnetii (Q fever) Phase 1 IgG ELISA (DRG International Inc. USA). PCR was performed to detect DNA of C. burnetii, Borrelia burgdorferi and Anaplasma phagocytophilum. Results Anti-C. burnetii IgG was detected in six foresters (7.3%). All foresters with the anti-C. burnetii IgG presence were positive toward anti-B. burgdorferi IgG and anti-TBE (tick-borne encephalitis). Anti-C. burnetii IgG was detected in fve farmers (6%). Four farmers with anti-C. burnetii IgG presence were positive toward anti-B. burgdorferi IgG and two with anti-TBE. Among them one was co-infected with B. burgdorferi and TBEV. Correlations between anti-C. burnetii IgG and anti-B. burgdorferi IgG presence and between anti-C. -
Non-Coding Rnas of the Q Fever Agent, Coxiella Burnetii
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 2015 Non-coding RNAs of the Q fever agent, Coxiella burnetii Indu Ramesh Warrier The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Warrier, Indu Ramesh, "Non-coding RNAs of the Q fever agent, Coxiella burnetii" (2015). Graduate Student Theses, Dissertations, & Professional Papers. 4620. https://scholarworks.umt.edu/etd/4620 This Dissertation is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. NON-CODING RNAS OF THE Q FEVER AGENT, COXIELLA BURNETII By INDU RAMESH WARRIER M.Sc (Med), Kasturba Medical College, Manipal, India, 2010 Dissertation presented in partial fulfillment of the requirements for the degree of Doctor of Philosophy Cellular, Molecular and Microbial Biology The University of Montana Missoula, MT August, 2015 Approved by: Sandy Ross, Dean of The Graduate School Graduate School Michael F. Minnick, Chair Division of Biological Sciences Stephen J. Lodmell Division of Biological Sciences Scott D. Samuels Division of Biological Sciences Scott Miller Division of Biological Sciences Keith Parker Department of Biomedical and Pharmaceutical Sciences Warrier, Indu, PhD, Summer 2015 Cellular, Molecular and Microbial Biology Non-coding RNAs of the Q fever agent, Coxiella burnetii Chairperson: Michael F. Minnick Coxiella burnetii is an obligate intracellular bacterial pathogen that undergoes a biphasic developmental cycle, alternating between a small cell variant (SCV) and a large cell variant (LCV). -

Circulatory and Lymphatic System Infections 1105
Chapter 25 | Circulatory and Lymphatic System Infections 1105 Chapter 25 Circulatory and Lymphatic System Infections Figure 25.1 Yellow fever is a viral hemorrhagic disease that can cause liver damage, resulting in jaundice (left) as well as serious and sometimes fatal complications. The virus that causes yellow fever is transmitted through the bite of a biological vector, the Aedes aegypti mosquito (right). (credit left: modification of work by Centers for Disease Control and Prevention; credit right: modification of work by James Gathany, Centers for Disease Control and Prevention) Chapter Outline 25.1 Anatomy of the Circulatory and Lymphatic Systems 25.2 Bacterial Infections of the Circulatory and Lymphatic Systems 25.3 Viral Infections of the Circulatory and Lymphatic Systems 25.4 Parasitic Infections of the Circulatory and Lymphatic Systems Introduction Yellow fever was once common in the southeastern US, with annual outbreaks of more than 25,000 infections in New Orleans in the mid-1800s.[1] In the early 20th century, efforts to eradicate the virus that causes yellow fever were successful thanks to vaccination programs and effective control (mainly through the insecticide dichlorodiphenyltrichloroethane [DDT]) of Aedes aegypti, the mosquito that serves as a vector. Today, the virus has been largely eradicated in North America. Elsewhere, efforts to contain yellow fever have been less successful. Despite mass vaccination campaigns in some regions, the risk for yellow fever epidemics is rising in dense urban cities in Africa and South America.[2] In an increasingly globalized society, yellow fever could easily make a comeback in North America, where A. aegypti is still present. -

Are Mycobacterium Drugs Effective for Treatment Resistant Lyme Disease, Tick-Borne Co-Infections, and Autoimmune Disease?
Central JSM Arthritis Bringing Excellence in Open Access Case Report *Corresponding author Richard I. Horowitz, Hudson Valley Healing Arts Center, 4232 Albany Post Road, Hyde Park, New York 12538, Are Mycobacterium Drugs USA, Tel: 845-229-8977; Fax: 845-229-8930; Email: Submitted: 15 June 2016 Effective for Treatment Accepted: 14 July 2016 Published: 16 July 2016 Resistant Lyme Disease, Tick- Copyright © 2016 Horowitz et al. Borne Co-Infections, and OPEN ACCESS Keywords Autoimmune Disease? • Lyme disease • Bartonella Richard I. Horowitz* and Phyllis R. Freeman • Tularemia Hudson Valley Healing Arts Center, USA • Behçet’s Disease/Syndrome • Rheumatoid arthritis • Dapsone Abstract • Pyrazinamide Introduction: PTLDS/chronic Lyme disease may cause disabling symptoms with • Persister bacteria associated overlapping autoimmune manifestations, with few clinically effective published treatment options. We recently reported on the successful use of a mycobacterium drug, Dapsone, for those with PTLDS. We now report on the novel use of another mycobacterium drug, pyrazinamide, (PZA), in relieving resistant symptomatology secondary to Lyme disease and associated co-infections, while decreasing autoimmune manifestations with Behçet’s syndrome. Method: Disabling multi-systemic/arthritic symptoms persisted in a Lyme patient with co-infections (Bartonella, tularemia) and overlapping rheumatoid arthritis/ Behçet’s disease, despite several rotations of classic antibiotic and DMARD regimens. Dapsone, a published treatment protocol used for Behçet’s syndrome, recently has been demonstrated to be effective in the treatment of PTLDS/chronic Lyme disease and co-infections. It was superior to prior treatment regimens in relieving some resistant chronic tick-borne/autoimmune manifestations; however, it did not effectively treat the skin lesions and ulcers secondary to Behçet’s disease, nor significantly affect the granuloma formation, joint swelling, and pain associated with Lyme, Bartonella, and RA.