Initial Agreement October 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Item 7: NHS Highland Assurance Report
Agenda 7. Item Report CLH No 17/19 HIGHLAND COUNCIL Committee: Care, Learning and Housing Date: 14 March 2019 Report Title: NHS Highland Assurance Report Report By: Interim Director of Care and Learning 1. Purpose/Executive Summary 1.1 The purpose of this report is to provide assurance to NHS Highland in relation to services commissioned and delivered through Highland Council. The content of each assurance report is informed by discussion with the Child Health Commissioner. 2. Recommendations 2.1 Members are asked to scrutinise the data and issues raised in this report. Comments will be incorporated into a report to NHS Highland as part of the agreed governance arrangements. 3. Performance Data 3.1 NHS Highland continue to advise of technical issues for the Child Health Surveillance data and would like to reassure you that they are continuing to look for this to be resolved as part of the work progressing nationally around the ‘Child Public Health and Wellbeing Transformational Change System’. 4. Health Visitor update 4.1 Health visitor numbers continue to increase with a further 5 health visitor trainees qualifying at the beginning of February 2019. This brings the total of successful trainees since the start of the Scottish Government programme to 20, with a further 5 due to qualify in January 2020. This will still leave a gap in vacancies against our establishment of health visitor posts when taking into account planned retirals. This indicates that there is a need for an ongoing and sustained training and recruitment programme for health visitors within Highland Council. 4.2 A further development in Scottish health visiting is the recent agreement of a national job description which has been produced to reflect the changed health visiting role as a result of the introduction of the Universal Health Visitor Pathway (UHVP) and the introduction of the Named Person. -

Accident and Emergency: Performance Update
Accident and Emergency Performance update Prepared by Audit Scotland May 2014 Auditor General for Scotland The Auditor General’s role is to: • appoint auditors to Scotland’s central government and NHS bodies • examine how public bodies spend public money • help them to manage their finances to the highest standards • check whether they achieve value for money. The Auditor General is independent and reports to the Scottish Parliament on the performance of: • directorates of the Scottish Government • government agencies, eg the Scottish Prison Service, Historic Scotland • NHS bodies • further education colleges • Scottish Water • NDPBs and others, eg Scottish Police Authority, Scottish Fire and Rescue Service. You can find out more about the work of the Auditor General on our website: www.audit-scotland.gov.uk/about/ags Audit Scotland is a statutory body set up in April 2000 under the Public Finance and Accountability (Scotland) Act 2000. We help the Auditor General for Scotland and the Accounts Commission check that organisations spending public money use it properly, efficiently and effectively. Accident and Emergency | 3 Contents Summary 4 Key messages 7 Part 1. A&E waiting times 9 Part 2. Reasons for delays in A&E 20 Part 3. Action by the Scottish Government 37 Endnotes 41 Appendix 1. NHS Scotland A&E departments and minor injury units 43 Appendix 2. National context for A&E and unscheduled care, 2004 to 2014 45 Exhibit data When viewing this report online, you can access background data by clicking on the graph icon. The data file will -

Emergency Departments
ED Site List 220711 v2.xls NHS Scotland - Emergency Departments Table 1: NHS Scotland - list of sites providing emergency care File NHS Board Site Type Location Name Location Address Comments Type Ayrshire & Arran ED Ayr Hospital DALMELLINGTON ROAD, AYR, KA6 6DX E Crosshouse Hospital KILMARNOCK ROAD, KILMARNOCK, AYRSHIRE, KA2 0BE E MIU/Other Arran War Memorial Hospital LAMLASH, ISLE OF ARRAN, KA27 8LF A Davidson Cottage Hospital THE AVENUE, GIRVAN, KA26 9DS A Closed from May-10 Girvan Community Hospital BRIDGEMILL, GIRVAN, AYRSHIRE, KA26 9HQ A Opened from May-10 Lady Margaret Hospital COLLEGE ST, MILLPORT, ISLE OF CUMBRAE, KA28 0HF A Opened from Oct-07 Borders ED Borders General Hospital MELROSE, TD6 9BS E MIU/Other Hawick Cottage Hospital VICTORIA ROAD, HAWICK, TD9 7AH A Hay Lodge Hospital NEIDPATH ROAD, PEEBLES, EH45 8JG A Kelso Hospital INCH ROAD, KELSO, TD5 7JP A Knoll Hospital STATION ROAD, DUNS, TD11 3EL A Dumfries & Galloway ED Dumfries & Galloway Royal Infirmary BANKEND ROAD, DUMFRIES, DG1 4AP E Galloway Community Hospital DALRYMPLE STREET, STRANRAER, DG9 7DQ E MIU/Other Castle Douglas Hospital ACADEMY STREET, CASTLE DOUGLAS, DG7 1EE A Kirkcudbright Hospital TOWNEND, KIRKCUDBRIGHT, DG6 4BE A Moffat Hospital HOLMEND, MOFFAT, DG10 9JY A Newton Stewart Hospital NEWTON STEWART, DG8 6LZ A Fife ED Victoria Hospital HAYFIELD ROAD, KIRKCALDY, KY2 5AH E MIU/Other Adamson Hospital BANK STREET, CUPAR, KY15 4JG A Queen Margaret Hospital WHITEFIELD ROAD, DUNFERMLINE, KY12 0SU E St Andrews Memorial Hospital ABBEY WALK, ST ANDREWS, KY16 9LG -

Parliamentary Questions on Covid-19 and Answers by the Scottish Government
PARLIAMENTARY QUESTIONS ON COVID-19 AND ANSWERS BY THE SCOTTISH GOVERNMENT Thursday 2 July 2020 Written questions lodged on 2 July can be found on page 12 of this document. ANSWERS TO PARLIAMENTARY QUESTIONS (Received on 2 July) Government Initiated Question George Adam (Paisley) (Scottish National Party): To ask the Scottish Government when it will publish an update on Scotland’s approach to physical distancing. S5W-30404 John Swinney: The Scottish Government has today published COVID-19: Scotland’s route map through and out of the crisis – Update on approach to physical distancing in light of advice from the Scottish Government COVID-19 Advisory Group which provides an update on the approach to physical distancing in Scotland as we move through Phase 2 and Phase 3 of the Route Map. This approach continues to be informed by evidence and has been updated in light of advice from the Scottish Government COVID-19 Advisory Group which has also been published today. The publication also updates on the final stage of Phase 2 of Scotland’s Route Map. Continued progress in suppressing the virus, as measured by the latest data, means that we are able to confirm the indicative dates for the remainder of Phase 2, concerning relaxation of the 5-mile guidance on travel for leisure purposes, the re- opening of self-contained, self-catering accommodation and the re-opening of outdoor hospitality. Changes to allow children and young-people more opportunity to meet up are also set out. Ministerial portfolio: Economy, Fair Work and Culture Iain Gray (East Lothian) (Scottish Labour): To ask the Scottish Government whether restrictions have been placed on the Individual Training Account scheme for 2020-21 because of the COVID-19 pandemic and, if so, in what sectors. -

Highland Council Transport Programme Consultation Feedback Report
Highland Council Transport Programme Consultation Feedback Report Contents Page number Introduction 3 Inverness and Nairn 8 Easter Ross and Black Isle 31 Badenoch and Strathspey 51 Eilean a’ Cheo 64 Wester Ross and Lochalsh 81 Lochaber 94 Caithness 109 Section 1 Introduction Introduction The Council currently spends £15.003m on providing mainstream home to school, public and dial a bus transport across Highland. At a time of reducing budgets, the Council has agreed a target to reduce the budget spent on the provision of transport by 15%. The Transport Programme aims to consider the needs of communities across Highland in the preparation for re-tendering the current services offered. It is important to understand the needs and views of communities to ensure that the services provided in the future best meet the needs of communities within the budget available. The public engagement for the transport programme commenced Monday 26th October 2015 and over a 14-week period sought to obtain feedback from groups, individuals and transport providers. This consultation included local Member engagement, a series of 15 public meetings and a survey (paper and online). The feedback from this consultation will contribute to the process of developing a range of services/routes. The consultation survey document asked questions on: • How suitable the current bus services are – what works, what should change and the gaps • Is there anything that prevents or discourages the use of bus services • What type of bus service will be important in the future • What opportunities are there for saving by altering the current network Fifteen public meetings where held throughout Highland. -

Emergency Departments
ED-site-list NHS Scotland - Emergency Departments Table 1: NHS Scotland - list of sites providing emergency care NHS Board Site Type Location Name Location Address File Type Comments Ayrshire & Arran ED Ayr Hospital DALMELLINGTON ROAD, AYR, KA6 6DX E Crosshouse Hospital KILMARNOCK ROAD, KILMARNOCK, AYRSHIRE, KA2 0BE E MIU/Other Arran War Memorial Hospital LAMLASH, ISLE OF ARRAN, KA27 8LF A Davidson Cottage Hospital THE AVENUE, GIRVAN, KA26 9DS A Closed from May-10 Girvan Community Hospital BRIDGEMILL, GIRVAN, AYRSHIRE, KA26 9HQ A Opened from May-10 Lady Margaret Hospital COLLEGE ST, MILLPORT, ISLE OF CUMBRAE, KA28 0HF A Opened from Oct-07 Borders ED Borders General Hospital MELROSE, TD6 9BS E MIU/Other Hawick Cottage Hospital VICTORIA ROAD, HAWICK, TD9 7AH A Hay Lodge Hospital NEIDPATH ROAD, PEEBLES, EH45 8JG A Kelso Hospital INCH ROAD, KELSO, TD5 7JP A Knoll Hospital STATION ROAD, DUNS, TD11 3EL A Dumfries & Galloway ED Dumfries & Galloway Royal Infirmary BANKEND ROAD, DUMFRIES, DG1 4AP E Galloway Community Hospital DALRYMPLE STREET, STRANRAER, DG9 7DQ E MIU/Other Castle Douglas Hospital ACADEMY STREET, CASTLE DOUGLAS, DG7 1EE A Kirkcudbright Hospital TOWNEND, KIRKCUDBRIGHT, DG6 4BE A Moffat Hospital HOLMEND, MOFFAT, DG10 9JY A Newton Stewart Hospital NEWTON STEWART, DG8 6LZ A Fife ED Queen Margaret Hospital WHITEFIELD ROAD, DUNFERMLINE, KY12 0SU E Victoria Hospital HAYFIELD ROAD, KIRKCALDY, KY2 5AH E MIU/Other Adamson Hospital BANK STREET, CUPAR, KY15 4JG A St Andrews Memorial Hospital ABBEY WALK, ST ANDREWS, KY16 9LG A Forth Valley -

Aviemore and Broadford Preferred for New Hospitals
Highlights MONTHLY March 2014 MEET THE BOARD: GRAHAM CRERAR A fund of experience AVIEMORE AND BROADFORD Dr Boyd Peters at Ian Charles PREFERRED FOR Hospital in Grantown-on-Spey NEW HOSPITALS St Vincents Hospital, Kingussie BROADFORD and Aviemore community hospital and resource have emerged as the pre- centre in Aviemore, starting a ferred locations for new hos- wider redesign of health and so- pitals in Highland. cial care services and closing Ian On 11th March, the steering Charles Hospital in Grantown-on- group looking into the redesign of Spey and St Vincent Hospital in health and adult social care ser- Kingussie. vices in Skye, Lochalsh and Work will now take place to South West Ross chose Broad- identify possible sites in ford as its preferred location for a Aviemore for the new hospital and resource centre, and this will new hospital in the area. Mackinnon Memorial Hospital, form part of the formal consulta- A week earlier, a special meet- Broadford ing of the NHS Highland board tion. decided to go to formal three- In Skye, Lochalsh and South month consultation in Badenoch West Ross, an extensive engage- & Strathspey, where there has ment exercise resulted in a pre- already been extensive commu- ferred option being chosen for the nity engagement on service re- future shape of service provision. design. The result of this is the This was to modernise local ser- emergence of a preferred option vices, including those provided by for change – developing a new Continued on page 2 Portree Hospital - - Preferred locations for new hospitals Continued from front page of the NHS Highland board to at pains to point out at its special pave the way for a formal, three- meeting this month that much the area’s two hospitals, Portree month consultation on the full had still to be done before any and Mackinnon Memorial in service model and possible site construction work starts. -
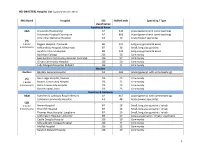
Report on Progress to Implement the Recommendations in the Independent External
Report on progress to implement the recommendations in the independent external view of Skye, Lochalsh and South West Ross Out of Hours Services by Sir Lewis Ritchie in May 2018 Introduction David Alston, chair of NHS Highland, requested a review of Out of Hours Services in Skye, Lochalsh and south west Ross from Sir Lewis Ritchie in November 2017. A report with recommendations was provided by Sir Lewis in May 2018, which has been accepted by all concerned. The work undertaken by Sir Lewis was particularly helpful in enabling all concerned to drawn a line under previous differences and move forward with greater clarity on next steps. Actions to Date This report provides the first update on the work being taken toward implementing 15 recommendations make by Sir Lewis Ritchie. The report follows a format that has been requested by Sir Lewis, and is in line with a format used to update on other reviews. The format is based on a self report using black, red, amber and green (BRAG) categories. There are different definitions of each colour in different versions of the BRAG tool, but the definitions used in this report are: Green - "active and on-track"; Amber - "active but some concerns and needs to be monitored closely"; Red - "Active but major concerns and needs corrective action;" Blue - "on-hold"; Black - “closed”1,2. A self assessment has been provided by staff from NHS Highland, NHS 24, and the Scottish Ambulance Service against each of the 15 recommendations made by Sir Lewis. An assessment of “risk and readiness” has also been provided by an Independent Facilitator in relation to each recommendation. -
MASTER) Hospital List (Updated October 2015
HEI (MASTER) Hospital List (updated October 2015) NHS Board Hospital ISD Staffed beds Speciality / Type classification Ayrshire & Arran A&A University Hospital Ayr A2 343 Acute (general with some teaching) University Hospital Crosshouse A2 666 Acute (general with some teaching) Arran War Memorial Hospital A3 19 Acute (mixed speciality) (9) 3 acute Biggart Hospital, Prestwick B6 121 Long stay geriatric & acute 6 community Kirklandside Hospital, Kilmarnock B7 36 Small, long stay geriatric Ayrshire Central Hospital B8 142 Long stay geriatric & acute Davidson Cottage J26 26 Community East Ayrshire Community Hospital, Cumnock J26 57 Community Girvan Community Hospital J26 20 Community Lady Margaret Hospital, Millport J26 9 Community Borders Borders Borders General Hospital A2 265 Acute (general, with some teaching) (5) Hay Lodge Hospital, Peebles J26 23 Community 1 acute Hawick Community Hospital J26 22 Community 4 community Kelso Community Hospital J26 23 Community Knoll Hospital, Duns J26 23 Community Dumfries & Galloway D&G Dumfries & Galloway Royal Infirmary A2 367 Acute (general, with some teaching) Galloway Community Hospital A3 48 Acute (mixed speciality) (10) 2 acute Annan Hospital B7 18 Small, long stay geriatric / rehab 8 community Thornhill Hospital B7 13 Small, long stay geriatric / rehab Thomas Hope Hospital, Langholm B7 10 Small, long stay geriatric / rehab Lochmaben Hospital, Lockerbie B9 17 Long stay geriatric / rehab / psychiatry Castle Douglas Hospital J26 19 Community Kirkcudbright Cottage Hospital J26 9 Community Moffat Hospital J26 12 Community Newton Stewart Hospital J26 19 Community 1 HEI (MASTER) Hospital List (updated October 2015) Fife Fife Victoria Hospital, Kirkcaldy A2 621 Acute (general with some teaching) (7) Queen Margaret Hospital, Dunfermline A3 196 Acute (mixed speciality) 2 acute 5 community Cameron Hospital, Leven B7 95 Small, long stay geriatric Adamson Hospital, Cupar J26 19 Community Glenrothes Hospital J26 74 Community Randolph Wemyss Memorial Hospital J26 16 Community St. -

Women, Pregnancy and Substance Misuse Revised Good Practice Guidelines
Revised Good Practice Guidelines Women, Pregnancy and Substance Misuse Protocol Reference: 009/250810 Date of Issue: September 2010 Prepared by: Lorna MacAskill, Midwifery Date of Review: September 2012 Development Of!cer, Sandra Harrington, Consultant Midwife Lead Reviewer: Sandra Harrington, Version: 2 Consultant Midwife Rati!ed by: Nursing, Midwifery & AHP Date: 25th August 2010 Policies, Procedures and Guidelines Group EQIA undertaken: 6th July 2010 EQIA Completed: 25th August 2010 Distribution: • Board Nurse Director • Youth Justice Strategy Group • Lead Midwives/Midwives • Highland Alcohol and Drug • University of Stirling Partnership (HADP) - Highland Campus Midwifery Dept • Argyll and Bute Alcohol and Drug • University of Paisley - Midwifery Dept Partnership (ABADP) • Lead Nurses/Health Visitors • Area Medical Committee • Osprey House • Councils on Alcohol • CPN(A)s including dual Diagnosis Workers • Women’s Aid • GPs & GP Sub Group • Action for Children • Obstetricians • APEX • Directorate Managers/Clinical Services Managers • Northern & Strathclyde Police • Assistant General Managers/Locality Managers • Local Authority: • Homeless Day Centre • Team Managers for children and • Connecting Young Carers families • Beechwood • Integrated Services Of!cers • Caley House • Integrated Services Co-ordinators • Direct Health Services Management Team • Fostering Service • Nursing, Midwifery & AHP Leadership Committee • Youth Action Teams • Clinical Governance Department • Argyll & Bute Head of Children’s • Child Protection Action Group Services - Highland and Argyll & Bute • STRADA, Highland Method CD Rom Email ü Paper Intranet ü Warning - Document uncontrolled when printed Version: 2 Date of Issue: September 2010 Page 1 Date of Review: September 2012 Contents Women, Pregnancy & Substance Misuse Revised Good Practice Guidelines Page no Foreword 4 Summary of Guidelines 6 1. Background 7 2. The Principles of Addressing Health Behaviour Change 8 3. -

NHS Education for Scotland
NHS Education for Scotland Rural Fellowships in General Practice – Local Job Information Information for NHS Highland, West: Skye, Lochalsh and Wester Ross Rural Fellowship A one-year fellowship based in stunning Skye, with the possiblity of supporting the unique and world-leading model of care in the Small Isles. This innovative fellowship will link both with GP practices and the established team of Advanced Nurse Practitioners (Broadford and Portree based) for a multi-disciplinary educational experience. Background One of the most breathtaking destinations in Europe, the area is centred around the famous Isle of Skye, dominated by the imposing Cuillin ridge. The Skye Lochalsh and Wester Ross area is part of the North and West Operational Unit within NHS Highland. Skye, Lochalsh and Wester Ross are a natural geographical grouping in the West Highlands which is centred on the Isle of Skye. This acts as the administrative and medical hub for a diverse group of remote and rural communities encompassing the communities of Glenelg, Kyle of Lochalsh, Broadford, Sleat, Carbost, Dunvegan, Portree on the Isle of Skye and Applecross, Torridon, Lochcarron, Ullapool and Gairloch in Wester Ross. The local cultural identity is enhanced by the mountains, islands and musical tradition of the area. It has access to the complete range of outdoor sports. Tourism, fish farming, forestry, crafting and fishing are the economic drivers in addition to good quality public services from the NHS, Education and NHS Highland and Highland Council. Mackinnon Memorial Hospital is based on the Isle of Skye and is run by Rural Practitioners who also provide OOH for the practices patients on the Island. -

Job Pack for This Post Can Be Accessed At
CONSULTANT IN GERIATRIC MEDICINE BELFORD HOSPITAL And Lochaber Community Information Pack MS12029625 APPOINTMENT OF CONSULTANT GERIATRIC MEDICINE, BELFORD HOSPITAL INFORMATION PACK Section 1 Welcome Section 2 Advert Section 3 Job Information Section 4 Job Plan Section 5 Person Specification Section 6 Terms and Conditions Section 1 – Welcome Introduction Thank you for your interest in joining NHS Highland. This information package contains details relating to the local area, this post and the Terms and Conditions of Service. NHS Highland is committed to becoming a learning organisation, recognising that staff require access to opportunities to learn, maintain and develop skills and knowledge, and we recognise the importance of valuing and supporting our staff throughout their time here. We offer: Policies to help balance commitments at work and home and flexible family friendly working arrangements Excellent training and development opportunities. On-site library services at the Centre for Health Sciences Access to NHS staff benefits/staff discounts Cycle to Work Scheme Excellent student support Access to NHS Pension scheme Recruitment Process Applicants are expected to make contact with the department before applying and we would strongly encourage those that are shortlisted to visit the department prior to interview. The cost of one preliminary visit will be met by NHS Highland. When organising a visit, candidates must agree appropriate travel and accommodation arrangements with the Medical Staffing Department prior to booking.