Hemophilia and Bleeding Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Skin Injuries – Can We Determine Timing and Mechanism?
Skin injuries – can we determine timing and mechanism? Jo Tully VFPMS Seminar 2016 What skin injuries do we need to consider? • Bruising • Commonest accidental and inflicted skin injury • Basic principles that can be applied when formulating opinion • Abrasions • Lacerations }we need to be able to tell the difference • Incisions • Stabs/chops • Bite marks – animal v human / inflicted v ‘accidental’ v self-inflicted Our role…. We are often/usually/always asked…………….. • “What type of injury is it?” • “When did this injury occur?” • “How did this injury occur?” • “Was this injury inflicted or accidental?” • IS THIS CHILD ABUSE? • To be able to answer these questions (if we can) we need knowledge of • Anatomy/physiology/healing - injury interpretation • Forces • Mechanisms in relation to development, plausibility • Current evidence Bruising – can we really tell which bruises are caused by abuse? Definitions – bruising • BLUNT FORCE TRAUMA • Bruise =bleeding beneath intact skin due to BFT • Contusion = bruise in deeper tissues • Haematoma - extravasated blood filling a cavity (or potential space). Usually associated with swelling • Petechiae =Pinpoint sized (0.1-2mm) hemorrhages into the skin due to acute rise in venous pressure • medical causes • direct forces • indirect forces Medical Direct Indirect causes mechanical mechanical forces forces Factors affecting development and appearance of a bruise • Properties of impacting object or surface • Force of impact • Duration of impact • Site - properties of body region impacted (blood supply, -
Immune Thrombocytopenia Purpura (ITP)
Immune Thrombocytopenia Purpura (ITP) Information for patients and carers from the Haematology Department What is ITP? Immune thrombocytopenic purpura (ITP) is a condition which causes the number of platelets in Spleen your blood to be reduced. Platelets are cells that help blood to clot and they help to prevent bleeding and bruising after an injury. If you do not have enough platelets in your blood, you are likely to bruise easily or may be unable to stop bleeding if you cut yourself. In ITP, your body’s immune system destroys your own platelets. White blood cells in your blood and your spleen (an organ in your abdomen) are part of your immune system. One of their actions is to produce antibodies which help your body to fight Diagram showing the position of infections. If you develop ITP, your immune system the spleen becomes overactive and produces antibodies that cause your platelets to be destroyed in the spleen; this results in a low platelet count. ITP is a type of autoimmune condition (which means your immune system is acting against your body rather than for it). ITP in adults is more common in women than men. It is very different from ITP in children, who usually get ITP after a viral infection but who recover without any treatment. ITP in adults normally needs treatment. Some people with ITP have other autoimmune conditions, such as rheumatoid arthritis, or infections such as hepatitis or HIV. If you have any of these medical issues, your ITP may be treated slightly differently. 1 of 8 ITP (August 2021) A normal platelet count is between 150 and 400 thousand million platelets per litre of blood. -

081999 Disseminated Intravascular Coagulation
The New England Journal of Medicine Current Concepts Systemic activation+ of coagulation DISSEMINATED INTRAVASCULAR COAGULATION Intravascular+ Depletion of platelets+ deposition of fibrin and coagulation factors MARCEL LEVI, M.D., AND HUGO TEN CATE, M.D. Thrombosis of small+ Bleeding and midsize vessels+ ISSEMINATED intravascular coagulation is and organ failure characterized by the widespread activation Dof coagulation, which results in the intravas- Figure 1. The Mechanism of Disseminated Intravascular Coag- cular formation of fibrin and ultimately thrombotic ulation. occlusion of small and midsize vessels.1-3 Intravascu- Systemic activation of coagulation leads to widespread intra- lar coagulation can also compromise the blood sup- vascular deposition of fibrin and depletion of platelets and co- agulation factors. As a result, thrombosis of small and midsize ply to organs and, in conjunction with hemodynam- vessels may occur, contributing to organ failure, and there may ic and metabolic derangements, may contribute to be severe bleeding. the failure of multiple organs. At the same time, the use and subsequent depletion of platelets and coag- ulation proteins resulting from the ongoing coagu- lation may induce severe bleeding (Fig. 1). Bleeding may be the presenting symptom in a patient with disseminated intravascular coagulation, a factor that can complicate decisions about treatment. TABLE 1. COMMON CLINICAL CONDITIONS ASSOCIATED WITH DISSEMINATED ASSOCIATED CLINICAL CONDITIONS INTRAVASCULAR COAGULATION. AND INCIDENCE Sepsis Infectious Disease Trauma Serious tissue injury Disseminated intravascular coagulation is an ac- Head injury Fat embolism quired disorder that occurs in a wide variety of clin- Cancer ical conditions, the most important of which are listed Myeloproliferative diseases in Table 1. -

Bleeds and Bruises in Children with Haemophilia
Bleeds and Bruises in CHildren WiTH HaeMOPHilia MusCle ANd/or JoiNt Bleeds Call the parent/guardian P.r.i.C.e. siGNs oF A serious HeAd Bleed P : Protection * Headache. Lower Limb: Take weight off the joint or muscle * drowsiness. Upper Limb: No carrying using affected arm * Nausea. r : rest * Vomiting. • Rest means rest! * unsteady Balance. • Try not to allow use of the joint or muscle where * irritability. possible. * Confusion. * seizures. i : ice * loss of consciousness. • Regular ice packs can help with pain & reduce swelling. • Put an ice pack over the affected area for 20 minutes. Repeat every two hours. DO NOT leave the ice pack on for more than 20 minutes siGNs oF A soFt tissue DO NOT place ice pack directly on skin (Use a tea Bleed towel/cold pack cover) * Bruising, discolouring of skin. C : Compression * Mild swelling. • Use an elasticated bandage to compress the affected area to reduce swelling. e : elevation • Elevate the affected limb to help reduce swelling. siGNs oF AN ABdoMiNAl • Keep the affected joint or muscle above the level of the Bleed heart. * Bloody, black or tar-like First Aid bowel motions. * red or brown urine. Mouth & Gum Bleeds * Pain. These can be hard to control because clots that form are * Vomiting of blood (blood washed away by saliva or knocked off by the tongue or food. Try giving the child an ice cube or ice pop to suck. may be red or black). These bleeds may need treatment by parents or the treatment centre. Nosebleeds siGNs oF BleediNG iNto tHe Tilt head forward and pinch the bridge of the nose below the bone for 10 - 20 minutes and / or put an ice-pack on JoiNts or MusCles the bridge of the nose for not more than 5 minutes. -

Isolated Plantar Vein Thrombosis Resembling a Corn with a Bruise
JE Hahm, et al pISSN 1013-9087ㆍeISSN 2005-3894 Ann Dermatol Vol. 31, No. 1, 2019 https://doi.org/10.5021/ad.2019.31.1.66 CASE REPORT Isolated Plantar Vein Thrombosis Resembling a Corn with a Bruise Ji Eun Hahm, Kang Su Kim, Jae Won Ha, Chul Woo Kim, Sang Seok Kim Department of Dermatology, Kangdong Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea Plantar vein thrombosis, rarely-reported disease, is usually or callus, plantar fibromatosis, or plantar verruca1. Among accompanied by pain and tenderness in the plantar region laborers, they may develop from excess pressure on the and should be differentiated from other dermatological con- bony prominences of the feet, repetitive uneven friction ditions causing plantar pain, such as hemorrhagic corn/cal- from footwear, or gait abnormalities. Plantar vein throm- lus, plantar epidermal cyst, verruca, or plantar fibromatosis. bosis is a rare condition causing plantar pain. The exact A 52-year-old man presented with a violaceous tender sub- cause of plantar vein thrombosis is yet unclear, but predis- cutaneous nodule overlying a hyperkeratotic plaque on his posing conditions, such as prior trauma, surgery, paraneo- sole. Initially, he thought it was a corn and applied keratolytic plastic syndromes, or coagulation disorders have been agents, which failed to work. Sonography revealed a well-de- described. To date, there is no established treatment ex- marcated mass with increased peripheral vascularity. His cept surgical excision, but reportedly, nonsteroidal anti-in- pain was relieved after a complete wide excision, which con- flammatory drug or heparin with elastic bandage is known firmed the mass to be plantar vein thrombosis after histo- to be effective for symptomatic control2-5. -

What Everyone Should Know to Stop Bleeding After an Injury
What Everyone Should Know to Stop Bleeding After an Injury THE HARTFORD CONSENSUS The Joint Committee to Increase Survival from Active Shooter and Intentional Mass Casualty Events was convened by the American College of Surgeons in response to the growing number and severity of these events. The committee met in Hartford Connecticut and has produced a number of documents with rec- ommendations. The documents represent the consensus opinion of a multi-dis- ciplinary committee involving medical groups, the military, the National Security Council, Homeland Security, the FBI, law enforcement, fire rescue, and EMS. These recommendations have become known as the Hartford Consensus. The overarching principle of the Hartford Consensus is that no one should die from uncontrolled bleeding. The Hartford Consensus recommends that all citizens learn to stop bleeding. Further information about the Hartford Consensus and bleeding control can be found on the website: Bleedingcontrol.org 2 SAVE A LIFE: What Everyone Should Know to Stop Bleeding After an Injury Authors: Peter T. Pons, MD, FACEP Lenworth Jacobs, MD, MPH, FACS Acknowledgements: The authors acknowledge the contributions of Michael Cohen and James “Brooks” Hart, CMI to the design of this manual. Some images adapted from Adam Wehrle, EMT-P and NAEMT. © 2017 American College of Surgeons CONTENTS SECTION 1 3 ■ Introduction ■ Primary Principles of Trauma Care Response ■ The ABCs of Bleeding SECTION 2 5 ■ Ensure Your Own Safety SECTION 3 6 ■ A – Alert – call 9-1-1 SECTION 4 7 ■ B – Bleeding – find the bleeding injury SECTION 5 9 ■ C – Compress – apply pressure to stop the bleeding by: ■ Covering the wound with a clean cloth and applying pressure by pushing directly on it with both hands, OR ■Using a tourniquet, OR ■ Packing (stuff) the wound with gauze or a clean cloth and then applying pressure with both hands SECTION 6 13 ■ Summary 2 SECTION 1: INTRODUCTION Welcome to the Stop the Bleed: Bleeding Control for the Injured information booklet. -

Bruise, Contusion & Ecchymosis Conventions
Bruise, Contusion and Ecchymosis MedDRA Proactivity Proposal Implementation MedDRA Version 16.0 I. MSSO Recognized Definitions of Concepts and Terms The MSSO has designated Dorland’s Illustrated Medical Dictionary as the standard reference for medical definitions. The following definitions are cited from Dorland’s 27th edition: Bruise – A superficial injury produced by impact without laceration; a contusion Contusion – A bruise; an injury of a part without a break in the skin Ecchymosis – A small hemorrhagic spot, larger than a petechia, in the skin or mucous membrane forming a nonelevated, rounded or irregular, blue or purplish patch. Hematoma – A localized collection of blood, usually clotted, in an organ, space, or tissue, due to a break in the wall of a blood vessel. Hemorrhage – The escape of blood from the vessels; bleeding. Petechia – A pinpoint, non-raised, perfectly round, purplish red spot caused by intradermal or submucous hemorrhage. Additional comments regarding the definitions: Bruise and contusion are synonymous, and are often used in a colloquial context. Bruise and contusion are each considered a result of injury. Bruise and contusion have been used to describe minor hemorrhage within tissue, where traumatized blood vessels leak blood into the interstitial space. Commonly, capillaries and sometimes venules are injured within skin, subcutaneous tissue, muscle, or bone. In addition to trauma, the terms bruise, ecchymosis, and to a lesser extent, contusion, have also been used as clinical signs of disorders of platelet function, coagulopathies, venous congestion, allergic reactions, etc. Hemorrhage may be used to describe blood escaping from vessels and retained in the interstitial space, and perhaps more commonly, to describe the escape of blood from vessels, and flowing freely external to the tissues. -

Immune Thrombocytopenic Purpura in a Twin Girl Revealed by a Traumatic Injury in Parakou (North Benin)
Immune thrombocytopenic purpura in a twin girl revealed by a traumatic injury in parakou (North Benin) Adedemy JD 1*, Noudamadjo A 1, Kpanidja G 1, Agossou J 1, Agbeille Mohamed F 1, Dovonou CA 2 1 Mother and Child Department, Parakou Teaching Hospital, Republic of Benin, and Faculty of Medicine, University of Parakou West Africa 2 Department of Medicine, Parakou Teaching Hospital, and Faculty of Medicine, University of Parakou, West Africa Abstract Background: ITP seems to be rare but in tropical settings thrombocytopenia is often encountered among children. Objective: Authors through this case report are putting emphasy on the diagnosis and management of ITP in a 4 year old twin girl admitted in the pediatric emergency ward for hematuria and bleeding from various origins seen in the context of a domestic trauma. Results: The various clinical signs have been analyzed to confirm ITP through exclusion of other possible health conditions. The management of ITP depend on the severity of clinical signs and in some cases the situations can be life threatening. In this case report, Blood transfusion and corticosteroids were the main treatment tools. The hospital stay was about 47 days and an ambulatory follow up was conducted for almost 6 months. Conclusion: In the context of various bleeding disorders, hematuria and thrombocytopenia, autoimmune thrombocytopenia in a twin girl was revealed by a domestic trauma. Citation: Adedemy JD, Noudamadjo A, Kpanidja G, Agossou J, Agbeille MF, Dovonou CA (2019) Immune Thrombocytopenic Purpura in a twin girl revealed by a traumatic injury in Parakou (North Benin). Adv Pediatr Res 6:27. -

How Significant Is Bleeding in Antiphospholipid Antibody
Treatment of Anti-Phospholipid Syndrome and Prothrombin Deficiency with Plasma Exchange Lowell Tilzer KU Medical Center Department of Pathology & Lab Medicine Case 72 YEARS OLD FEMALE PRESENTED TO KUMC WITH BLEEDING FOLLOWING ROUTINE HEMORRHOIDECTOMY SURGERY Past Medical History • Surgeries: Bilateral tubal ligation, appendectomy, partial hysterectomy, bilateral bunion surgery – No bleeding complications • 2008: Presented to ER with chest pain – Incidentally found prolonged PT and PTT + Lupus anticoagulant and anticardiolipin antibodies • 2009: Melanotic stool with severe anemia (Hb 4) – Blood transfusion (>10 units) – Attributed to long-term use of Aspirin Brief course Initial Work-up Reported Normal Test Value Range PT/INR 2.2 (HIGH) 0.8-1.2 PTT 87.4 (HIGH) 24.0-40.0 PT mixing study @ 60 mins 1.5 (HIGH) PTT mixing study @ 60 mins 82.8 (HIGH) Factor 2 assay 10% (LOW) 50-150% Factor 5 assay 78% 50-150% Factor 7 assay 153% (HIGH) 50-150% Factor 8 assay 235% (HIGH) 50-150% Factor 10 assay 68% 50-150% 300 Linear dilutions 250 200 150 100 % Normal control 50 0 Factor 2 Factor 5 Factor 7 Factor 8 Factor 10 Additional coagulation study Test Result Interpretation dRVVT Prolonged Lupus anticoagulant Abs Hexagonal Lupus Positive Lupus anticoagulant Abs anticoagulant Anti-b2 GPI IgG Positive Anti-b2 GPI IgM Positive Support APS diagnosis Anti-cardiolipin IgG Positive Anti-cardiolipin IgM Positive There is NO Factor 2 inhibitor, therefore previous result of low Factor 2 inhibitor <0.4 BU Factor 2 level was due to lupus (activity-based) anticoagulant Abs against phospholipids in the assay. Algorithm for Screening tests (PT/INR, aPTT) coagulopathies Mixing study Heparin, DTI PL dependent assays (aPTT or dRVVT + Hexa) PTT PT PT PTT LA+ Factor LA- Intrinsic Common Extrinsic inhibitors pathway pathway pathway Revised Criteria for Antiphospholipid Syndrome (APS) (Sydney Criteria) APS: ≥ 1 Laboratory Criteria AND ≥ 1 Clinical Criteria • Laboratory Criteria: “≥ 2 occasions 3 months apart” 1. -
Using Tourniquets to Stop Bleeding
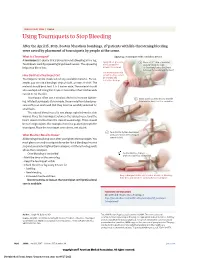
JAMA PATIENT PAGE | Trauma Using Tourniquets to Stop Bleeding After the April 15, 2013, Boston Marathon bombings, 27 patients with life-threatening bleeding were saved by placement of tourniquets by people at the scene. What Is a Tourniquet? Applying a tourniquet with a windlass device A tourniquet is a device that is placed around a bleeding arm or leg. Apply direct pressure 1 Place a 2-3” strip of material Tourniquets work by squeezing large blood vessels. The squeezing to the wound for about 2” from the edge helps stop blood loss. at least 15 minutes. of the wound over a long bone between the wound and the heart. Use a tourniquet only How Do I Put a Tourniquet On? when bleeding cannot be stopped and Tourniquets can be made out of any available material. For ex- is life threatening. ample, you can use a bandage, strip of cloth, or even a t-shirt. The material should be at least 2 to 3 inches wide. The material should also overlap itself. Using thin straps or material less than 2 inches wide can rip or cut the skin. Tourniquets often use a windlass device to increase tighten- 2 Insert a stick or other strong, straight ing. Inflated tourniquets (for example, those made from blood pres- item into the knot to act as a windlass. sure cuffs) can work well. But they must be carefully watched for small leaks. The injured blood vessel is not always right below the skin wound. Place the tourniquet between the injured vessel and the heart, about 2 inches from the closest wound edge. -

A Guide for People Living with Von Willebrand Disorder CONTENTS
A guide for people living with von Willebrand disorder CONTENTS What is von Willebrand disorder (VWD)?................................... 3 Symptoms............................................................................................... 5 Types of VWD...................................................................................... 6 How do you get VWD?...................................................................... 7 VWD and blood clotting.................................................................... 11 Diagnosis................................................................................................. 13 Treatment............................................................................................... 15 Taking care of yourself or your child.............................................. 19 (Education, information, first aid/medical emergencies, medication to avoid) Living well with VWD......................................................................... 26 (Sport, travel, school, telling others, work) Special issues for women and girls.................................................. 33 Connecting with others..................................................................... 36 Can I live a normal life with von Willebrand disorder?............. 37 More information................................................................................. 38 2 WHAT IS VON WILLEBRAND DISORDER (VWD)? Von Willebrand disorder (VWD) is an inherited bleeding disorder. People with VWD have a problem with a protein -

Intracranial Haemorrhage in a 26 Year-Old Woman with Idiopathic Thrombocytopenic Purpura
Postgraduate Medical Journal (1987) 63, 781-783 Postgrad Med J: first published as 10.1136/pgmj.63.743.781 on 1 September 1987. Downloaded from Intracranial haemorrhage in a 26 year-old woman with idiopathic thrombocytopenic purpura Gavin Awerbuch and Reuven Sandyk Department ofNeurology, University ofArizona Health Sciences Center, Tucson, AZ. 85724, USA. Summary: Intracranial haemorrhage (ICH), a rare complication of idiopathic thrombocytopenic purpura (ITP), described only once previously in an adult, is usually fatal. We report a previously healthy 26 year old woman with chronic ITP in whom spontaneous ICH developed. The eventual favourable outcome in this case despite severe initial neurological deficit makes this case unusual. The importance of aggressive management in an ITP associated ICH is stressed and a plan for management is suggested. Introduction Although relatively rare, intracranial haemorrhage of 5.7 g/dl, white blood count of 15.5 x I09/l with a (ICH) is the most serious complication of idiopathic normal differential and a platelet count of 6.0 x 109/l, thrombocytopenic purpura (ITP) and is the leading reticulocyte count was 3.2%. The prothrombin time, reported cause ofdeath.'`3 In children, nearly 20 cases partial thromboplastin time, thrombin time, fibrin- Protected by copyright. of acute ITP complicated by ICH have been reported. ogen, fibrin monomers, and fibrin split products were Previous reports have alluded to ICH associated with all normal. An electroencephalogram (EEG), gallium ITP in adults,4`7 but ICH has been documented only scan of the abdomen, chest X-ray, and computerized once in adults.8 We report the occurrence of an axial tomography (CT scan) of the head were normal.