A Case Report from the Anesthesia Incident Reporting System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Risk Assessment Guidance
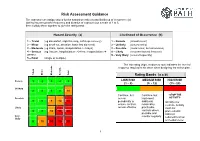
Risk Assessment Guidance The assessor can assign values for the hazard severity (a) and likelihood of occurrence (b) (taking into account the frequency and duration of exposure) on a scale of 1 to 5, then multiply them together to give the rating band: Hazard Severity (a) Likelihood of Occurrence (b) 1 – Trivial (eg discomfort, slight bruising, self-help recovery) 1 – Remote (almost never) 2 – Minor (eg small cut, abrasion, basic first aid need) 2 – Unlikely (occurs rarely) 3 – Moderate (eg strain, sprain, incapacitation > 3 days) 3 – Possible (could occur, but uncommon) 4 – Serious (eg fracture, hospitalisation >24 hrs, incapacitation >4 4 – Likely (recurrent but not frequent) weeks) 5 – Very likely (occurs frequently) 5 – Fatal (single or multiple) The risk rating (high, medium or low) indicates the level of response required to be taken when designing the action plan. Trivial Minor Moderate Serious Fatal Rating Bands (a x b) Remote 1 2 3 4 5 LOW RISK MEDIUM RISK HIGH RISK (1 – 8) (9 - 12) (15 - 25) Unlikely 2 4 6 8 10 Continue, but Continue, but -STOP THE Possible review implement ACTIVITY- 3 6 9 12 15 periodically to additional Identify new ensure controls reasonably controls. Activity Likely remain effective practicable must not controls where 4 8 12 16 20 proceed until possible and risks are Very monitor regularly reduced to a low likely 5 10 15 20 25 or medium level 1 Risk Assessments There are a number of explanations needed in order to understand the process and the form used in this example: HAZARD: Anything that has the potential to cause harm. -

Laryngospasm Caused by Removal of Nasogastric Tube After Tracheal Extubation: Case Report
Yanaka A, et al. J Anesth Clin Care 2021, 8: 061 DOI: 10.24966/ACC-8879/100061 HSOA Journal of Anesthesia & Clinical Care Case Report pCO2: Partial pressure of carbon dioxide pO : Partial pressure of oxygen Laryngospasm Caused by 2 mmHg: Millimeter of mercury Removal of Nasogastric Tube mg/dl: Milligram per deciliter mmol/L: Millimole per litter after Tracheal Extubation: Case Introduction Report Background Laryngospasm (spasmodic closure of the larynx) is an airway Ayumi Yanaka1 and Takuo Hoshi2* complication that may occur when a patient emerges from general 1Department of Anesthesiology and Critical Care Medicine, Ibaraki Prefectur- anesthesia. It is a protective reflex, but may sometimes result in al Central Hospital, Japan pulmonary aspiration, pulmonary edema, arrhythmia and cardiac 2Department of Anesthesiology and Critical Care Medicine, Clinical and Edu- arrest [1]. It does not often cause severe hypoxemia in the patient, and cational Training Center, Tsukuba University Hospital, Japan our review of the literature revealed no previous reports of such cases that cause of the laryngospasm was the removal of nasogastric tube. Here, we describe this significant adverse event in a case and suggest Abstract ways to lessen the possibility of its occurrence. We obtained written informed consent for publication of this case report from the patient. Background: We report a case of laryngospasm during nasogastric tube removal. Laryngospasm is a severe airway complication after Case report surgery and there have been no reports associated with the removal of nasogastric tubes. A 54-year-old woman height, 157 cm; weight, 61 kg underwent abdominal surgery (partial hepatectomy with right partial Case Report: After abdominal surgery, the patient was extubated the tracheal tube, and was removed the nasogastric tube. -
Operational Risk Management Guide
OPERATIONAL RISK MANAGEMENT GUIDE U.S. DEPARTMENT OF AGRICULTURE FOREST SERVICE 2020 Last Updated 02/26/2020 RISK MANAGEMENT COUNCIL IN COOPERATION WITH THE OFFICE OF SAFETY & OCCUPATIONAL HEALTH and THE NATIONAL AVIATION SAFETY COUNCIL Contents Contents ....................................................................................................................................................................................... 2 Executive Summary .................................................................................................................................................................. i Introduction ............................................................................................................................................................................... 1 What is Operational Risk Management? ................................................................................................................... 1 The Terminology of ORM ................................................................................................................................................ 1 Principles of ORM Application ........................................................................................................................................... 6 The Five-Step ORM Process ................................................................................................................................................ 7 Step 1: Identify Hazards .................................................................................................................................................. -
Hanging, Strangulation and Other Forms of Asphyxiation
Hanging, Strangulation and Other Forms of Asphyxiation Steven Campman, M.D. Chief Deputy Medical Examiner San Diego County 16 October 2018 Overview • Terms • Other forms of asphyxiation • Neck Compression –Hanging –Strangulation Asphyxia • The physical and chemical state caused by the interference with normal respiration. • A condition that interferes with cells ability to receive or use oxygen. General Effects • Decrease and cessation of breathing • Leads to bradycardia and eventually asystole • Slowing, then flattening of the EEG Many Terms • Gag: to obstruct the mouth • Choke: to compress or otherwise obstruct the airway • Strangle: asphyxia by external compression of the throat •Throttle: same as strangle; especially manual strangulation • Garrote: strangle; especially ligature strangulation •Burking: chest compression and smothering. Many Terms • Suffocate: (broad term) a layperson’s synonym for asphyxiation, sometimes used to mean smother. • Choke –a layperson’s term for strangulation –A medical term for internal blocking of the airway Classification of Asphyxia Neck Airway Mechanical Exclusion Compression Obstruction Asphyxia of Oxygen Airway Obstruction •Smothering •Gagging •Choking (laryngeal blockage, aspiration, food bolus) Suicide Kit Choking Internal obstruction of airway • Mouth: gag • Larynx or trachea: obstruction by foreign body, “café coronary,” anaphylaxis, laryngospasm, epiglottitis • Tracheobronchial tree: aspiration, drowning FOOD BOLUS Anaphylaxis from Wasp Stings Mechanical Asphyxia Ability to breath is compromised -

The “Best” Way to Breath
Journal of Lung, Pulmonary & Respiratory Research Case Report Open Access The “Best” way to breath Abstract Volume 2 Issue 2 - 2015 A “best” way to breath is described resulting from discovering a pre-Heimlich method Samuel A Nigro of preventing choking. Because of four episodes in three months of terrifying complete laryngospasm, the physician-patient-writer, consistent with many medical discoveries Retired, Assistant Clinical Professor Psychiatry, Case Western Reserve University School of Medicine, USA in history, discovered a method of aborting the episodes. Breathing has always been taken for granted as spontaneously and naturally most efficient. To the contrary, Correspondence: Samuel A Nigro, Retired, Assistant Clinical nasal breathing is best with first closing the mouth which enhances oxygenation and Professor Psychiatry, Case Western Reserve University School trans-laryngeal respiration. Physiologic aspects are reviewed including nasal and oral of Medicine, 2517 Guilford Road, Cleveland Heights, Ohio respiratory distinctions, laryngeal musculature and structures, diaphragm control and 44118, USA, Tel (216) 932-0575, Email [email protected] neuro-functional speculations. Proposed is the SAM: Shut your mouth, Air in nose, and then Mouth cough (or exhale). Benefits include prevention of choking making the Received: January 07, 2015 | Published: January 26, 2015 Heimlich unnecessary; more efficient clearing of the throat and coughs; improving oxygenation at molecular level of likely benefit for pre-cardiac or pre-stroke anoxic crises; improving exertion endurance; and offering a psycho physiologic method for emotional crises as panics, rages, and obsessive-compulsive impulses. This is a simple universal public health technique needing universal promulgation for the integration of care for all work forces and everyone else. -

Dive Medicine Aide-Memoire Lt(N) K Brett Reviewed by Lcol a Grodecki Diving Physics Physics
Dive Medicine Aide-Memoire Lt(N) K Brett Reviewed by LCol A Grodecki Diving Physics Physics • Air ~78% N2, ~21% O2, ~0.03% CO2 Atmospheric pressure Atmospheric Pressure Absolute Pressure Hydrostatic/ gauge Pressure Hydrostatic/ Gauge Pressure Conversions • Hydrostatic/ gauge pressure (P) = • 1 bar = 101 KPa = 0.987 atm = ~1 atm for every 10 msw/33fsw ~14.5 psi • Modification needed if diving at • 10 msw = 1 bar = 0.987 atm altitude • 33.07 fsw = 1 atm = 1.013 bar • Atmospheric P (1 atm at 0msw) • Absolute P (ata)= gauge P +1 atm • Absolute P = gauge P + • °F = (9/5 x °C) +32 atmospheric P • °C= 5/9 (°F – 32) • Water virtually incompressible – density remains ~same regardless • °R (rankine) = °F + 460 **absolute depth/pressure • K (Kelvin) = °C + 273 **absolute • Density salt water 1027 kg/m3 • Density fresh water 1000kg/m3 • Calculate depth from gauge pressure you divide press by 0.1027 (salt water) or 0.10000 (fresh water) Laws & Principles • All calculations require absolute units • Henry’s Law: (K, °R, ATA) • The amount of gas that will dissolve in a liquid is almost directly proportional to • Charles’ Law V1/T1 = V2/T2 the partial press of that gas, & inversely proportional to absolute temp • Guy-Lussac’s Law P1/T1 = P2/T2 • Partial Pressure (pp) – pressure • Boyle’s Law P1V1= P2V2 contributed by a single gas in a mix • General Gas Law (P1V1)/ T1 = (P2V2)/ T2 • To determine the partial pressure of a gas at any depth, we multiply the press (ata) • Archimedes' Principle x %of that gas Henry’s Law • Any object immersed in liquid is buoyed -

Near Drowning
Near Drowning McHenry Western Lake County EMS Definition • Near drowning means the person almost died from not being able to breathe under water. Near Drownings • Defined as: Survival of Victim for more than 24* following submission in a fluid medium. • Leading cause of death in children 1-4 years of age. • Second leading cause of death in children 1-14 years of age. • 85 % are caused from falls into pools or natural bodies of water. • Male/Female ratio is 4-1 Near Drowning • Submersion injury occurs when a person is submerged in water, attempts to breathe, and either aspirates water (wet) or has laryngospasm (dry). Response • If a person has been rescued from a near drowning situation, quick first aid and medical attention are extremely important. Statistics • 6,000 to 8,000 people drown each year. Most of them are within a short distance of shore. • A person who is drowning can not shout for help. • Watch for uneven swimming motions that indicate swimmer is getting tired Statistics • Children can drown in only a few inches of water. • Suspect an accident if you see someone fully clothed • If the person is a cold water drowning, you may be able to revive them. Near Drowning Risk Factor by Age 600 500 400 300 Male Female 200 100 0 0-4 yr 5-9 yr 10-14 yr 15-19 Ref: Paul A. Checchia, MD - Loma Linda University Children’s Hospital Near Drowning • “Tragically 90% of all fatal submersion incidents occur within ten yards of safety.” Robinson, Ped Emer Care; 1987 Causes • Leaving small children unattended around bath tubs and pools • Drinking -

Cough and Laryngospasm Prevention During Orotracheal Extubation In
Brazilian Journal of Anesthesiology 71 (2021) 90---95 LETTER TO THE EDITOR −1 −1 0.25 mg.kg and ketamine 0.25 mg.kg also have showed Cough and laryngospasm 4 being effective for such purpose. prevention during orotracheal The timing of extubation according to the child’s breath- extubation in children with ing cycle is another point of interest. The author of an SARS-CoV-2 infection educational review about extubation in children mentions that he extubates the child at the end of spontaneous inspi- Dear Editor, ration without suction or positive pressure, arguing that at this point the child’s lungs are full of O2-enriched air and that Little is mentioned about the importance of avoiding cough the first trans laryngeal movement of air that follows directs and laryngospasm during extubation in the Operating Room all secretions away from the laryngeal structures decreasing 5 (OR) in pediatric patients with suspected or confirmed SARS- the risk of laryngospasm. CoV-2 infection. Coughing is an important source of viral According to the former, from the perspective of respira- contagion among humans and must be considered a high-risk tory complications associated with extubation, it is safer for complication for the health workers. Laryngospasm, more the health personnel to perform the extubation to a deep frequent in children than in adults, compels to intervene anesthetized patient, during spontaneous ventilation at the with positive pressure on the patient’s airway increasing the end of inspiration and in lateral decubitus. Special attention described risk. Different from intubation in the OR, where must be given to the use of the medications described for the anesthesiologist has certain control on the procedure, coughing and laryngospasm prevention after the withdrawal extubation and emergence from anesthesia have a greater of the orotracheal tube. -

Assigning Risk Assessment Codes
Exhibit 1 240 FW 5 Page 1 of 4 Assigning Risk Assessment Codes The Department of the Interior describes its Risk Assessment System in 485 DM 6, Inspections and Abatements. The policy mandates inspections, assignment of Risk Assessment Codes (RACs) to identified hazards, and abatement of the hazards within certain timeframes. The RACs are based on the hazard severity, probability of occurrence, and number of people exposed or potentially lost in the event of an accident. While all hazards should be resolved as soon as possible, the Risk Assessment System provides managers with safety risk ranking information to assist them in making informed decisions concerning hazard control. It also provides decisionmakers with a consistent and defensible approach to prioritizing safety hazard abatement efforts among the many competing resource demands and priorities. Step 1 – Learn the terminology Hazard – Anything that may cause harm, injury, or ill health. Risk – Risk is a measure of both the likelihood (probability) and the consequence (severity) of all hazards related to an activity or condition. Risk Assessment System (RAS) – A method provided by the Department to assist managers to prioritize safety and health deficiencies. Risk Assessment Code (RAC) – A hazard number ranking system from 1 (the highest level of risk) to 5 (the lowest level of risk). Risk Assessment Matrix – A tool used to assign RACs (see example below). XX/XX/13 OCCUPATIONAL SAFETY AND HEALTH Exhibit 1 240 FW 5 Page 2 of 4 Step 2 – Using the RAC Matrix Tool, assigning a code Evaluate each deficiency based on both the likelihood (probability) of an outcome occurring and the consequence (severity) of a potential outcome. -

Incidence of Laryngospasm and Bronchospasm in Pediatric Adenotonsillectomy
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln US Army Research U.S. Department of Defense 2012 Incidence of Laryngospasm and Bronchospasm in Pediatric Adenotonsillectomy Michael I. Orestes Walter Reed Army Medical Center Lina Lander University of Nebraska Medical Center, [email protected] Susan Verghese Children’s National Medical Center Rahul K. Shah Children’s National Medical Center, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/usarmyresearch Orestes, Michael I.; Lander, Lina; Verghese, Susan; and Shah, Rahul K., "Incidence of Laryngospasm and Bronchospasm in Pediatric Adenotonsillectomy" (2012). US Army Research. 257. https://digitalcommons.unl.edu/usarmyresearch/257 This Article is brought to you for free and open access by the U.S. Department of Defense at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in US Army Research by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. The Laryngoscope VC 2012 The American Laryngological, Rhinological and Otological Society, Inc. Incidence of Laryngospasm and Bronchospasm in Pediatric Adenotonsillectomy Michael I. Orestes, MD; Lina Lander, ScD; Susan Verghese, MD; Rahul K. Shah, MD Objectives/Hypothesis: To evaluate and describe airway complications in pediatric adenotonsillectomy. Study Design: Retrospective case-control study. Methods: A chart review of patients that underwent adenotonsillectomy between 2006 and 2010 was performed. Peri- operative complications, patient characteristics, and surgeon and anesthesia technique were recorded. Results: A total of 682 charts were reviewed. Eleven cases (1.6%) of laryngospasm were identified: one was preopera- tive, seven occurred in the operating room postextubation, and three occurred in the recovery area. Four patients were given succinylcholine, one was reintubated, and the other cases were managed conservatively. -

Personal Protective Equipment
LABORATORY BIOSAFETY MANUAL FOURTH EDITION AND ASSOCIATED MONOGRAPHS PERSONAL PROTECTIVE EQUIPMENT LABORATORY BIOSAFETY MANUAL FOURTH EDITION AND ASSOCIATED MONOGRAPHS PERSONAL PROTECTIVE EQUIPMENT Personal protective equipment (Laboratory biosafety manual, fourth edition and associated monographs) ISBN 978-92-4-001141-0 (electronic version) ISBN 978-92-4-001142-7 (print version) © World Health Organization 2020 Some rights reserved. This work is available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/ licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization (http://www.wipo.int/amc/en/ mediation/rules/). Suggested citation. Personal protective equipment. Geneva: World Health Organization; 2020 (Laboratory biosafety manual, fourth edition and associated monographs). -
Risk Assessment Checklist
Preventing Workplace Harassment & Violence: Toolkit for Trucking & Logistics Employers WORKPLACE HARASSMENT AND VIOLENCE PREVENTION REGULATIONS Workplace Risk Assessment Checklist Recent changes to the Canada Labour Code introduce new obligations for federally regulated employers. One important new piece of legislation is Bill C-65, which protects against harassment and violence in the workplace. BillC-65 introduced new Workplace Harassment and Violence Prevention Regulations, which came into force on January 1st, 2021. Under this new framework, employers are required to conduct a Work Place Risk Assessment as part of their responsibility to prevent workplace harassment and violence. Below you will find a Workplace Risk Assessment Checklist to help monitor your company’s practices and ensure compliance. The checklist contains information that is both required and recommended. Regulatory requirements per the Act are denoted by *. Legal Statement: The information contained within does not constitute legal advice. Trucking HR Canada, and all content contributors bear no responsibility for any circumstances arising out of or related to the adoption, or decision not to adopt any of the recommendations contained in the Workplace Risk Assessment Checklist. WORKPLACE RISK ASSESSMENT CHECKLIST 1 GETTING STARTED *You will be required to complete the workplace assessment with your company’s applicable partner. Depending on the size of your organization, "applicable partner" is defined as the policy committee (for employers with more than 300 employees), the workplace committee (for employers with 20 or more employees), or the health and safety representative (for employers with less than 19 employees). *Ensure individuals that are directed to identify the risks, or to develop and implement the preventative measures, are properly qualified and trained.