In This Issue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Emerald City of Oz by L. Frank Baum Author of the Road to Oz
The Emerald City of Oz by L. Frank Baum Author of The Road to Oz, Dorothy and The Wizard in Oz, The Land of Oz, etc. Contents --Author's Note-- 1. How the Nome King Became Angry 2. How Uncle Henry Got Into Trouble 3. How Ozma Granted Dorothy's Request 4. How The Nome King Planned Revenge 5. How Dorothy Became a Princess 6. How Guph Visited the Whimsies 7. How Aunt Em Conquered the Lion 8. How the Grand Gallipoot Joined The Nomes 9. How the Wogglebug Taught Athletics 10. How the Cuttenclips Lived 11. How the General Met the First and Foremost 12. How they Matched the Fuddles 13. How the General Talked to the King 14. How the Wizard Practiced Sorcery 15. How Dorothy Happened to Get Lost 16. How Dorothy Visited Utensia 17. How They Came to Bunbury 18. How Ozma Looked into the Magic Picture 19. How Bunnybury Welcomed the Strangers 20. How Dorothy Lunched With a King 21. How the King Changed His Mind 22. How the Wizard Found Dorothy 23. How They Encountered the Flutterbudgets 24. How the Tin Woodman Told the Sad News 25. How the Scarecrow Displayed His Wisdom 26. How Ozma Refused to Fight for Her Kingdom 27. How the Fierce Warriors Invaded Oz 28. How They Drank at the Forbidden Fountain 29. How Glinda Worked a Magic Spell 30. How the Story of Oz Came to an End Author's Note Perhaps I should admit on the title page that this book is "By L. Frank Baum and his correspondents," for I have used many suggestions conveyed to me in letters from children. -

THE WACKY WIZARD of OZ by Patrick Dorn
THE WACKY WIZARD OF OZ By Patrick Dorn Copyright © 2015 by Patrick Dorn, All rights reserved. ISBN: 978-1-60003-837-2 CAUTION: Professionals and amateurs are hereby warned that this Work is subject to a royalty. This Work is fully protected under the copyright laws of the United States of America and all countries with which the United States has reciprocal copyright relations, whether through bilateral or multilateral treaties or otherwise, and including, but not limited to, all countries covered by the Pan-American Copyright Convention, the Universal Copyright Convention and the Berne Convention. RIGHTS RESERVED: All rights to this Work are strictly reserved, including professional and amateur stage performance rights. Also reserved are: motion picture, recitation, lecturing, public reading, radio broadcasting, television, video or sound recording, all forms of mechanical or electronic reproduction, such as CD-ROM, CD-I, DVD, information and storage retrieval systems and photocopying, and the rights of translation into non-English languages. PERFORMANCE RIGHTS AND ROYALTY PAYMENTS: All amateur and stock performance rights to this Work are controlled exclusively by Brooklyn Publishers, LLC. No amateur or stock production groups or individuals may perform this play without securing license and royalty arrangements in advance from Brooklyn Publishers, LLC. Questions concerning other rights should be addressed to Brooklyn Publishers, LLC. Royalty fees are subject to change without notice. Professional and stock fees will be set upon application in accordance with your producing circumstances. Any licensing requests and inquiries relating to amateur and stock (professional) performance rights should be addressed to Brooklyn Publishers, LLC. Royalty of the required amount must be paid, whether the play is presented for charity or profit and whether or not admission is charged. -

A Rhetorical Analysis of Wicked's Elphaba
“IT’S JUST THAT FOR THE FIRST TIME, I FEEL… WICKED”: A RHETORICAL ANALYSIS OF WICKED’S ELPHABA USING KENNETH BURKE’S GUILT-PURIFICATION-REDEMPTION CYCLE by Patricia C. Foreman A Thesis Submitted in Partial Fulfillment of the Requirements for the Degree Master of Arts in Communication Studies at Liberty University May 2013 Foreman 2 Acknowledgements First and foremost, to “my Dearest, Darlingest Momsy and Popsicle,” and to my brother Gary, thank you so much for your constant support, encouragement, direction and love. I appreciate your words of wisdom and advice that always seem to be just what I need to hear. To each of my fellow graduate assistants, thank you for “dancing through life” with me. Thank you for becoming not only co-workers, but also some of my best friends. To my thesis committee – Dr. William Mullen, Dr. Faith Mullen, and Dr. Lynnda S. Beavers – thank you all so much for your help. This finished thesis is, without a doubt, the “proudliest sight” I’ve ever seen, and I thank you for your time, effort and input in making this finished product a success. Finally, to Mrs. Kim, and all of my fellow “Touch of Swing”-ers, who inspired my love of the Wicked production, and thus, this study. For the long days of rehearsals, even longer nights on tour buses, and endless hours of memories that I’ll not soon forget... “Who can say if I’ve been changed for the better? I do believe I have been changed for the better. And because I knew you, I have been changed for good.” Foreman 3 In Memory Of… Lauren Tuck May 14, 1990 – September 2, 2010 “It well may be that we will never meet again in this lifetime, so let me say before we part, so much of me is made of what I learned from you. -

Wizard of Oz Red 2Bused.Fdx
The Wizard of OZ __________________________ a LINX adaptation RED CAST LINX 141 LINDEN ST. WELLESLEY, MA 01746 (781) 235-3210 [email protected] PROLOGUE [ALL] GLINDA GREETS THE AUDIENCE CURTAIN OPENS. Behind the curtain is GLINDA. She looks at the audience with wonder.] GLINDA_PP What a wonderful audience. So many excited and eager faces. Are we all ready for an adventure? Watch one another’s back now. Things do sneak up on you in Oz. Fortunately, they can be very nice things... (points to back of house) Like that... 1ST SONG - FIREWORK ACT I, SCENE 1 [PP] IN WHICH DOROTHY IS CALLED BEFORE THE WIZARD. CHARACTERS: WIZARD, DOROTHY, SCARECROW, LION, TIN MAN [Head of Wizard hovers before audience. Below, Dorothy, Scarecrow, Lion and Tin Man tremble in terror. Mid-runner curtain is closed behind them. Also onstage is a booth with a hanging curtain. Thick ducts branch out from the booth.] WIZARD I am the great and powerful OZ! Who dares approach me? [Scarecrow, Lion and Tin Man shove Dorothy forward. Dorothy looks back at them.] SCARECROW_PP You got this. LION_PP We’re right behind you. [Dorothy turns toward Wizard. Scarecrow, Lion and Tin Man shuffle backwards. Dorothy turns to them, noticing the increased distance.] TIN MAN_PP Right behind you! 2. WIZARD (to Dorothy) Who are you? DOROTHY_PP My name is Dorothy. Dorothy Gale. WIZARD And where do you come from, “Dorothy Gale”? DOROTHY_PP Kansas. WIZARD Kansas? (long pause) What is Kansas? DOROTHY_PP It’s a place. My home - and I so want to return. A tornado picked up my home, picked up me and my little dog - only, he’s not so little anymore. -

Tin Woodman by L
The TIN WOODMAN by L. Frank Baum of Oz CHAPTER 16 - CAPTAIN FYTER “Are you really a soldier?” asked Woot, “She is called Nimmie Amee,” said the when they had all watched this strange tin per- Tin Soldier. Hearing this, they were all so as- son parade up and down the path and proudly tonished that they were silent for a time, re- flourish his sword. garding the stranger with wondering looks. “I was a soldier,” was the reply, “but I’ve Finally the Tin Woodman ventured to ask: been a prisoner to Mr. Rust so long that I don’t “And did Nimmie Amee return your know exactly what I am.” love?” “But—dear me!” cried the Tin Woodman, “Not at first,” admitted the Soldier. “When sadly perplexed; “how came you to be made of first I marched into the forest and met her, she tin?” was weeping over the loss of her former sweet- “That,” answered the Soldier, “is a sad, sad heart, a woodman whose name was Nick Chop- story. I was in love with a beautiful Munch- per.” kin girl, who lived with a Wicked Witch. The “That is me,” said the Tin Woodman. Witch did not wish me to marry the girl, so “She told me he was nicer than a soldier, she enchanted my sword, which began hack- because he was all made of tin and shone beau- ing me to pieces. When I lost my legs I went to tifully in the sun. She said a tin man appealed the tinsmith, Ku-Klip, and he made me some to her artistic instincts more than an ordinary tin legs. -
Antelope Class Writing Term 6, Week 3 Learning- 15.6.20 the Wonderful Wizard of Oz
Antelope Class Writing Term 6, Week 3 learning- 15.6.20 The Wonderful Wizard of Oz Hello Antelopes, well done for all of your hard work so far. This week, we are going to begin a 3 week fantasy story focus by looking at ‘The Wonderful Wizard of Oz’. It has been a pleasure to see the learning that has been taking place, and we look forward to hearing more about that this week. Please send a picture or scan of your writing to [email protected], either every couple of days or at the end of the week. There are 5 lessons and each lesson will take approximately 30-40 minutes. Miss McMillan and Mrs Smith Lesson 1 To understand the events of a text. This lesson, you are going to become familiar with ‘The Wizard of Oz’ and answer questions about the text. Context • ‘The Wonderful Wizard of Oz’ is a high fantasy novel, written by L. Frank Baum, published in 1900. It was the first published of 14 novels in the Oz series and it is the best known among all the author’s books. • Most of the novels are set in Oz, a land full of wonder, strange rules and mythical beings. • In the story, Dorothy lives in Kansas (America) on her aunt and uncle’s farm. One day, a huge tornado carries her house into the sky. She lands in the fantastical Land of Oz. • Dorothy meets three friends and they travel together to the Emerald City - to visit the Wizard and ask for his help. -

THE WONDERFUL WIZARD of OZ Adapted by Rachel Teagle from the Book by L
THE WONDERFUL WIZARD OF OZ Adapted by Rachel Teagle From the book by L. Frank Baum For all inquiries, please contact: Rachel Teagle (408) 316-8123 [email protected] Serenbe Playhouse Production Draft 2014 SMALL CAST CHARACTER BREAKDOWN Dorothy ACTOR 1- Scarecrow (male) ACTOR 2 - Tin Man (male) ACTOR 3 - Lion (female) ACTOR 4 – With of the North, Witch of the South, Oz Guard, Auxiliary Puppeteer, etc (female) ACTOR 5 – Witch of the West, Elfra, Glinda Guard, Aunt Em, Auxiliary Puppeteer (female) ACTOR 6 - Oz, King of Flying Monkeys, Boq, Auxiliary Puppeteer (male) ALTERNATE LARGE CAST BREAKDOWN Dorothy Toto Scarecrow Tin Man Lion Elfra Boq Additional Munchkin Townspeople Witch of the North/Witch of the South Oz Guard Oz Witch of the West/Aunt Em King of Flying Monkeys Additional Flying Monkeys STAGE: In an arc through the audience runs the yellow brick road, functioning like an apron, to accommodate travel and distraction from scene changes, with a path down the middle of the audience for the Witch of the West's entrance and the poppy scene. PRELUDE The audience gathers in Kansas. Perhaps Aunt Em passes through, looking for Dorothy. Dorothy passes through avoiding Aunt Em, her nose in a book. A tornado siren signals the audience to enter the space, and they travel down a path passing by characters they will see later in the play. SCENE 1: THE COUNCIL WITH THE MUNCHKINS DOROTHY Toto? Toto! Are you okay? I thought I'd lost you. Toto, I don't know what I would have done. I swear, Kansas has got to be the absolute most boring, awful place I've ever been. -
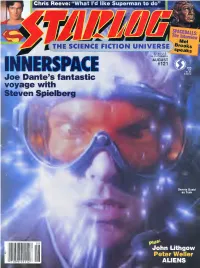
Starlog Magazine Issue
'ne Interview Mel 1 THE SCIENCE FICTION UNIVERSE Brooks UGUST INNERSPACE #121 Joe Dante's fantastic voyage with Steven Spielberg 08 John Lithgow Peter Weller '71896H9112 1 ALIENS -v> The Motion Picture GROUP, ! CANNON INC.*sra ,GOLAN-GLOBUS..K?mEDWARO R. PRESSMAN FILM CORPORATION .GARY G0D0ARO™ DOLPH LUNOGREN • PRANK fANGELLA MASTERS OF THE UNIVERSE the MOTION ORE ™»COURTENEY COX • JAMES TOIKAN • CHRISTINA PICKLES,* MEG FOSTERS V "SBILL CONTIgS JULIE WEISS Z ANNE V. COATES, ACE. SK RICHARD EDLUND7K WILLIAM STOUT SMNIA BAER B EDWARD R PRESSMAN»™,„ ELLIOT SCHICK -S DAVID ODEll^MENAHEM GOUNJfOMM GLOBUS^TGARY GOODARD *B«xw*H<*-*mm i;-* poiBYsriniol CANNON HJ I COMING TO EARTH THIS AUGUST AUGUST 1987 NUMBER 121 THE SCIENCE FICTION UNIVERSE Christopher Reeve—Page 37 beJohn Uthgow—Page 16 Galaxy Rangers—Page 65 MEL BROOKS SPACEBALLS: THE DIRECTOR The master of genre spoofs cant even give the "Star wars" saga an even break Karen Allen—Page 23 Peter weller—Page 45 14 DAVID CERROLD'S GENERATIONS A view from the bridge at those 37 CHRISTOPHER REEVE who serve behind "Star Trek: The THE MAN INSIDE Next Generation" "SUPERMAN IV" 16 ACTING! GENIUS! in this fourth film flight, the Man JOHN LITHGOW! of Steel regains his humanity Planet 10's favorite loony is 45 PETER WELLER just wild about "Harry & the CODENAME: ROBOCOP Hendersons" The "Buckaroo Banzai" star strikes 20 OF SHARKS & "STAR TREK" back as a cyborg centurion in search of heart "Corbomite Maneuver" & a "Colossus" director Joseph 50 TRIBUTE Sargent puts the bite on Remembering Ray Bolger, "Jaws: -

Core Concepts in Heroism Science, Volume Two
University of Richmond UR Scholarship Repository Bookshelf 2020 Core Concepts in Heroism Science, Volume Two Scott T. Allison University of Richmond Follow this and additional works at: https://scholarship.richmond.edu/bookshelf Part of the Community Psychology Commons, Social Psychology Commons, and the Theory and Philosophy Commons Recommended Citation Allison, S. T. (Ed.). (2020). Core Concepts in Heroism Science (Vol. Two). Richmond, VA: Palsgrove. NOTE: This PDF preview of Core Concepts in Heroism Science, Volume Two includes only the preface and/or introduction. To purchase the full text, please click here. This Book is brought to you for free and open access by UR Scholarship Repository. It has been accepted for inclusion in Bookshelf by an authorized administrator of UR Scholarship Repository. For more information, please contact [email protected]. CORE CONCEPTS IN HEROISM SCIENCE VOLUME TWO First published 2020 by Palsgrove Copyright © 2020 by Scott T. Allison. All rights reserved. Printed in the United States of America. No part of the book may be used or reproduced without written permission with the exception of brief quotations. Library of Congress Cataloging in Publication Data Name: Allison, Scott T., Editor Title: Core Concepts in Heroism Science, Volume 2 Edited by Scott T. Allison Description: 1 Edition | Richmond: Palsgrove, 2020 | Includes bibliographical references Identifiers: ISBN-9798650178880 ISBN: 9798650178880 COVER IMAGE: Illustration by Jamie Katz. Design by Dylan Vavra CORE CONCEPTS IN HEROISM SCIENCE VOLUME TWO Edited by Scott T. Allison University of Richmond Praise for Core Concepts in Heroism Science “Meticulously researched, and a lively read, this book is a brilliant example of the meaningful and collaborative scholarship that emerges from the partnership between gifted students and their faculty mentors.” -- Dr. -

Worksheet: the Wizard of Oz – a Timeline
WORKSHEET: THE WIZARD OF OZ – A TIMELINE Match the dates listed below to the events that happened that year. The events (on the next page) are jumbled up and in no particular order. You can write them next to the date or cut out and paste them. Year Event 1856 1886 1897 1900 1902 1904 1911 1919 1925 1939 1942 1987 2011 2017 www.wizardofozthemusical.com WORKSHEET: THE WIZARD OF OZ – A TIMELINE The Royal Shakespeare Company creates a theatrical adaptation based on the MGM film. The first novel sequel (one of 13 such sequels) The Marvellous Land of Oz is reluctantly written by Baum. Baum dies in Hollywood. His last words are, reportedly, “Now we can cross the Shifting Sands”. The Wizard of Oz (Lloyd Webber / Rice version) Australian tour opens. Baum publishes his first book,The Book of the Hamburgs. The subject of the book: how to raise chickens. MGM makes The Wizard of Oz, starring Judy Garland, billed as “the happiest film ever”. The first stage musical ofThe Wizard of Oz is produced with lyrics by Baum and runs on Broadway for 293 shows. The Wonderful Wizard of Oz book is published, and is a great hit, earning praise in a New York Times review. L. Frank Baum born in Chittenango, New York, as the seventh of nine children. Dorothy makes her first appearance in Baum’s first children’s book,Mother Goose in Prose, a collection of 22 children’s stories based on Mother Goose nursery rhymes. The St Louis Municipal Opera creates a stage musical based on the MGM film. -

An Introduction to the Award Winning Musical About Wicked
TEACHERS PACK: AN INTRODUCTION TO THE AWARD WINNING MUSICAL ABOUT WICKED The premise of Wicked is that you have not been told the whole story about the land of Oz. It encourages you to look at things very differently by exploring the themes of friendship, trust and tolerance, the use of propaganda and the manipulation of public opinion. Was the Wicked Witch of the West really wicked? Was Glinda the Good really so good? Why was the Lion so cowardly? How did the Tin Man lose his heart and the Scarecrow his brain? And why did the Wicked Witch of the West want the jewelled shoes so much? Wicked sets out to explore all of this and more. The musical is often described as a ‘prequel’ to The Wizard of Oz but in fact the story takes place before, simultaneously and after the familiar Oz tale. It has been described as creating ‘a parallel universe to that of the Wizard of Oz’ and a ‘re-imagining of the same world’ that looks at things very differently. SYNOPSIS OF THE WIZARD OF OZ Whisked away from Kansas by a swirling tornado, Dorothy’s house crushes the Wicked Witch of the East when it lands in the dazzling world of Oz. Glinda the Good Witch gives Dorothy the dead witch’s jewelled slippers and sends her off along the yellow brick road which leads to the Wizard’s Kingdom. Along the way she is joined by a scarecrow with no brain, a tin man without a heart and a lion that lacks courage, each of them believing that the Wizard can give them what they want most in life. -

Wizard E-Mail Sample
(This is a 50 page abridged version of the 62 page full-length play .) “School Play” By Michele L. Vacca Version (From the famous L. Frank Baum novel.) © Copyright as an unpublished work by Michele L. Vacca /1994 © Copyright by ON STAGE! 1994, 2001 All rights reserved IMPORTANT NOTICE : This E-mail “sample” of the complete playbook is formatted in the same “size” and pagination as the complete script – and is intended for individual perusal for production only. The possession of this “sample,” without written authorization having first been obtained from the publisher, confers no right or license to use this copyrighted material in any way not sanctioned in writing by the publisher, either publicly or in private. PLEASE NOTE : It is forbidden by copyright law to reproduce copyrighted material in any form, without the written permission of the copyright owner. For information concerning production rights requests, Royalty fees, etc., contact the author or the publisher: ON STAGE! – CLASSICS ON STAGE! P.O. Box 25365 Chicago, IL 60625 (USA) Tel: 1 773 989-0532 E-mail: [email protected] Website – http://www.classicsonstage.com/ IT IS AGAINST FEDERAL LAW TO COPY – 1 – copyright – On Stage! PRODUCTION NOTES : CHARACTERS : IN KANSAS : DOROTHY, a young orphan AUNT EM and UNCLE HENRY, Dorothy’s only family MR. LYON, MR. CROWE, and MR. WOODMAN, farmhands MIZ SWITCH, a nasty neighbor TOTO, a stuffed toy in a basket IN THE LAND OF OZ : GLINDA, a good witch The MUNCHKINS, a group of timid folks who love to eat The WICKED WITCH of the West SCARECROW TIN MAN LION GATEKEEPER of the City of Oz OZMA, loyal employee of Oz OGMA, the Wizard’s very efficient secretary WIZARD, the “Great and Powerful” HOCUS and POCUS, sidekicks to the Wicked Witch The script is designed so that a total of 8 actors (four women and four men) can play all of the roles.