Dynamic Geometry and Plaque Development in the Coronary Arteries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ronald Davis Oral History Collection on the Performing Arts
Oral History Collection on the Performing Arts in America Southern Methodist University The Southern Methodist University Oral History Program was begun in 1972 and is part of the University’s DeGolyer Institute for American Studies. The goal is to gather primary source material for future writers and cultural historians on all branches of the performing arts- opera, ballet, the concert stage, theatre, films, radio, television, burlesque, vaudeville, popular music, jazz, the circus, and miscellaneous amateur and local productions. The Collection is particularly strong, however, in the areas of motion pictures and popular music and includes interviews with celebrated performers as well as a wide variety of behind-the-scenes personnel, several of whom are now deceased. Most interviews are biographical in nature although some are focused exclusively on a single topic of historical importance. The Program aims at balancing national developments with examples from local history. Interviews with members of the Dallas Little Theatre, therefore, serve to illustrate a nation-wide movement, while film exhibition across the country is exemplified by the Interstate Theater Circuit of Texas. The interviews have all been conducted by trained historians, who attempt to view artistic achievements against a broad social and cultural backdrop. Many of the persons interviewed, because of educational limitations or various extenuating circumstances, would never write down their experiences, and therefore valuable information on our nation’s cultural heritage would be lost if it were not for the S.M.U. Oral History Program. Interviewees are selected on the strength of (1) their contribution to the performing arts in America, (2) their unique position in a given art form, and (3) availability. -

Thirty-Eighth Annual Convocation, June
t ?s3 SOUTHERN METHODIST UNIVERSITY THIRTY-EIGHTH ANNUAL CONVOCATION COMMENCEMENT EXERCISES and CONFERRING OF DEGREES TUESDAY EVENING, THE SECOND OF JUNE NINETEEN HUNDRED FIFTY-THREE AT SIX O'CLOCK McFARLIN MEMORIAL AUDITORIUM THE ORDER OF EXERCISES Flrrvrprrrr,¡. Flosrono, Ph,D,, Prouost ol the Uniaersìty, Presiding THE PRELUDE Toccata Gìgout Sil,ence is reqøested d'ariøg tbe þrelade. Done Bencr,lt, 8.M., A,A.G.O., Associøte Prolessor ol Otgøt THE CONVOCATION PROCESSION The Mamh¿ls of the Unive¡sfty The R,epresentatives of the Cl¡ss of 1928 The Offlcen of the Unlvenity The Candidates for Baccalaureate Degreeg The Candldatæ for llonorary Degrees The Candidates for lligher Deg¡ees (]r THE PROCESSIONAL Marche Pontitcele Lemmms Tlte øadience aill støød for the þrocession, THE INVOCATION TrrB RBvsnrNo R. J. LePneon, B.D. Pøstor, Centrøl Methodìst Churcb, Brownwood, Texøs THE SOLO Eternal Life Dangøn Mnnr KaTrrERTNE JoRDAN, Contralto {'r \_.¿ THE ANNUAL STATEMENT Docron Flosrono Thc Tfurlitze¡ Organ is fu¡nishcd by Btooh Mays and Comprny 2 l { Candìdøtes for tbe Bøccølaureøte Degree wíth Honors: IN rrrs Co¡,rEcE or Anrs aNo ScrnNcrs 'Vitb Highest Honors Margaret Ann Alll¡o¡ Loulse Kent Kst¡e Mary Anne Hein Beatrice Ethel Marcu¡ Lee Glrard Pondron 'Vitb Hígb Honors Ernest Eottorff Be¿ttt Ellnor J¿nlce Klrby Allce lIart Bockus John Har4r LaPr¿tlc Beverly Lou C¿mpbell Bsy M¿rie Porter Helen Atrell Fi¡ley M¿rjo¡le Ann Reynolil¡ Robert Charles CþntD/ Doris Je¿n Stew¡lt Marion Goldman RobeÈ llyer lbomsg Ma¡y Owen Jone¡ Reb¿ Gerane B4rber W€rt Ife¡¡y Ye¡te¡, J¿ Vitb Ho¡ors Elm¡ Âdele A¡el Eleanor Jo¿¡ Joril¿¡ Barb¿ra Di¿ne Brolle¡ B¿¡b¡ra Lynetts McCluna \ftlligm Ch¿rle¡ Crouch Js¡lce Rr¡¡hùuÌ Patrlcla Brown Ourrln S¡llv Brlght Sutto¡ Røan¡e Díckso¡ ìf¡¡¡hsll Northw¡v Terrv. -
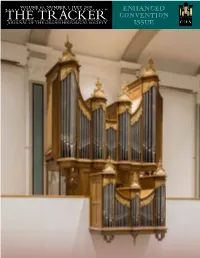
THE TRACKER CONVENTION JOURNAL of the ORGAN HISTORICAL SOCIETY ISSUE Schantz OHS-Tracker Ad Art.Qxp Layout 1 5/6/19 1:10 PM Page 1
VOLUME 63, NUMBER 3, JULY 2019 ENHANCED THE TRACKER CONVENTION JOURNAL OF THE ORGAN HISTORICAL SOCIETY ISSUE Schantz OHS-Tracker Ad Art.qxp_Layout 1 5/6/19 1:10 PM Page 1 Meeting the needs of organbuilding clients P. O. Box 156 Orrville, Ohio 44667 for one-hundred and forty-six years, www.schantzorgan.com Schantz Organ Company provides a tailored, [email protected] artistic response relying upon time-honored 800.416.7426 mechanisms and design principles. find us on A RTISTRY - R ELIABILITY - A DAPTABILITY Re-imaging Estey Organ Company, Opus 1318 (1914) - built for Fair Lane – the estate of Henry and Clara Ford – Dearborn, Michigan. The III-17, fitted with extant Estey pipework from the second two decades of the twentieth century, will be installed in the summer of 2019. Not simply an assembler of components, our artisans creatively adapt to each project's parameters – be that a newly commissioned instrument, the rebuild and adaptation of a long-serving example, or a strict historic restoration. S.L.Huntington&Co. PIPE ORGAN BUILDERS We are honored to have been commissioned to restore Hook & Hastings No. 1171, 1883 the only remaining unaltered three-manual Hook & Hastings from the 1880 decade. Completion Fall 2021 S.L.Huntington&Co. P.O. Box 56, stonington, ct 06378 J 401.348.8298 J www.slhorgans.com An International Monthly Devoted to the Organ, Harpsichord, Carillon and Church Music Now in Our Second Century Announcing The Diapason’s new digimag subscription. The digital edition is available at a special price ($35/year), and yet incorporates all the content in the traditional print edition. -

C K’NAY C (To Her) C (Poem by A
K ney C k’NAY C (To Her) C (poem by A. Belïy [(A.) BAY-lee] set to music by Sergei Rachmaninoff [sehr-GAYEE rahk-MAH-nyih-nuff]) Kaan C JindÍich z Albestç Kàan C YINND-rshihk z’AHL-bess-too KAHAHN C (known also as Heinrich Kàan-Albest [H¦N-rihh KAHAHN-AHL-besst]) Kabaivanska C Raina Kabaivanska C rah-EE-nah kah-bahih-WAHN-skuh C (known also as Raina Yakimova [yah-KEE-muh-vuh] Kabaivanska) Kabalevsky C Dmitri Kabalevsky C d’MEE-tree kah-bah-LYEFF-skee C (known also as Dmitri Borisovich Kabalevsky [d’MEE-tree bah-REE-suh-vihch kah-bah-LYEFF-skee]) C (the first name is also transliterated as Dmitry) Kabasta C Oswald Kabasta C AWSS-vahlt kah-BAHSS-tah Kabelac C Miloslav Kabelá C MIH-law-slahf KAH-beh-lahahsh Kabos C Ilona Kabós C IH-law-nuh KAH-bohohsh Kacinskas C Jerome Ka inskas C juh-ROHM kah-CHINN-skuss C (known also as Jeronimas Ka inskas [yeh-raw-NEE-mahss kah-CHEEN-skahss]) Kaddish for terezin C Kaddish for Terezin C kahd-DIHSH (for) TEH-reh-zinn C (a Holocaust Requiem [{REH-kôôee-umm} REH-kôôih-emm] by Ronald Senator [RAH-nulld SEH-nuh-tur]) C (Kaddish is a Jewish mourner’s prayer, and Terezin is a Czechoslovakian town converted to a concentration camp by the Nazis during World War II, where more than 15,000 Jewish children perished) Kade C Otto Kade C AWT-toh KAH-duh Kadesh urchatz C Kadesh Ur'chatz C kah-DEHSH o-HAHTSS C (Bless and Wash — a prayer song) Kadosa C Pál Kadosa C PAHAHL KAH-daw-shah Kadosh sanctus C Kadosh, Sanctus C kah-DAWSH, SAHNGK-tawss C (section of the Holocaust Reqiem — Kaddish for Terezin [kahd-DIHSH (for) TEH-reh-zinn] -

The Semi-Weekly Campus, Volume
presumptious Sifters Mustangs Face Spirited Falsehood Raxorbacks "The Semi-Weekly Campus" Is Published by the S. M. U. Students Publishing Co. I !QL. 24 SOUTHERN METHODIST UNIVERSITY, DALLAS, TEXAS, SATURDAY, NOVEMBER 12, 1938 No. 15 ews Cameras Will S.M.U. In Brazil Former S. M. U. Prof Gets "Scoop" Dean Of Women H. R* Knickerbocker', tick Today When Drive To Start Named Member War Correspondent, Sunday Morning Of Frosh Frat onies Play Hogs LINDOLFO LEUSIN TO TO REPRESENT SOUTH Will Lecture Here SPEAK BEFORE CHURCH ERN DISTRICT FOR GROUP THREE YEARS lfeWsreel cameramen for screenland's major studios are H. R. Knickerbocker, world-famous foreign correspondent .ected to be on hand today when the S.M.U. Mustangs S. M. U.'s annual drive for funds Miss Lide Spragins, dean of for International News Service, will speak in McFarlin Mem £t the Arkansas Razorbacks on the Ownby stadium grid- to support "Little S. M. U. in Bra women, has recently been appoint orial auditorium at 8 p. m., December 1, under the auspices zil" will get underway at 9:30 a. m. ed as a member-at-large of the of Sigma Delta Chi, professional journalism fraternity. ' was learned Friday that contacts have been made Sunday when Lindolfo Leusin, for National Executive council of Al Knickerbocker will speak on "A Texan at the Ringside of ugh R. J. O'Donnell, manager of Interstate theatres, mer student of the South American pha Lambda Delta, national fresh History." From 1923, when he left S.M.U. as head of the E. -

Piano Roll Review
~. @!IIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIil1.1111"11111111"111111111"1111111111111111111111111'IllllIllYU]llllllllllllllllllllllllllllllllllllllllllllllllllllml!JjllllllllllllllilllllllllllllllllUIlIIIIIIIIlIIIIrnl'~IIII~III~lIImlll~IIII~III~II!mllli~lIIfiDlII[jj1ll1 I . New . e MICA Th A s Bulletm of the AutomarIC MUSical Instrument Collectors' Association March 1983 Volume 20 Number 2 AMICA International AUTOMATIC MUSICAL INSTRUMENT COLLECTORS' ASSOCIATION AMICA MEMBERSHIP RATES: NEWS BULLETIN Continuing Members: $20 Annual Dues Overseas Members: $26 Dues PUBLISHER New Members, add $5 processing fee Dorothy Bromage (Write to Membership Secretary, P.O. Box 387 see address below) La Habra, CA 90631 USA Change of Address: If you move, send the new address and phone number to the Published by the Automatic Musical Instrument Collectors' Membership Secretary, Bobby Clark. Association, a non-profit club devoted to the restoration, dist".ibution and enjoyment of musical instruments using INTERNATIONAL OFFICERS perforated paper music rolls. AMICA was founded in San Francisco in 1963. PRESIDENT Terry Smythe (204) 452-2180 Contributions: All subjects of interest to readers of the 547 Waterloo St., Winnipeg, Manitoba Bulletin are encouraged and invited by the publisher. All Canada R3N 012 articles must be received by the 10th of the preceding PAST PRESIDENT Robert M. Taylor month. Every attempt will be made to publish all articles of (215) 735-2662 general interest to AMICA members at the earliest possible 1326 Spruce St. #3004, Phildelphia, PA 19107 time and at the discretion of the publisher. VICE PRESIDENT Molly Yeckley (419) 684-5742 Original Bulletin articles, or material for reprint that is of 612 Main St., Castalia, OH 44824 significant historical quality and interest, are encouraged and will be rewarded in the form of AMICA membership SECRETARY Richard Reutlinger (415) 346-8669 dues discounts. -

The Semi-Weekly Campus, Volume 25, Number 41, March 13, 1940
idcufb £djdtcto£UA. WuAtanqA filaif. Benefit To All <% §tmi-Wttk\# ® At Fat Stock Show 1915-1916 • The Silver Anniversary Year • 1939-1940 >L.25 Z727 SOUTHERN METHODIST UNIVERSITY, DALLAS, TEXAS, WEDNESDAY, MARCH 13, 1940 No. 41 oburn To Open Second Day Of Commerce Festivities Debate Teams Contest To Name Speaks Today Graduates Of Photo Contests Dean C. W. Thompson Starts Win In Meet Mechanical Man S.M.U. Live In For Engineers Is Announced Many States Annual Activity Tuesday At Waxahachie By JIMMY WILSON The annual contest for naming The graduates of the S. M. U. Is Announced the Engineering School's mechani Commerce School are scattered far Arthur Coburn, vice-president of the Southwestern Life Clymer, Ramey, Daniels and cal man for the Engineers show and wide over the United States Only Regularly Enrolled En Insurance Company, will open the second day of festivities Branson Capture Honors was announced Tuesday by Jerry and many are already well on their gineers Eligible, States in the annual Commerce School celebration with a speech to Last Week Stover, publicity chairman for the way to success in the business Dean E. H. Flath students and faculty of the Commerce School in Arden Hall event. world. at 11 a. m. today. All Commerce School classes will be dis Anne Clymer- and Ben Ramey Two photoplay contests, open missed at that time. The contest will be open to all Dudley W. Curry, '36, and only to engineering students, in won individual honors and Morris S. M. U. students except engineer Charles Anthony, '38, have both • The celebration will be brought Daniels and Robert Branson cap which a total of $20 in prizes will rtf • MM • 1 to a close this afternoon with a ing upperclassmen and will close earned a master's degree at North be awarded, were announced Tues tured team honors in a debate held Monday, March 18, he said. -

QRS Recorda PLAYER ROLLS Q.R.S
Catalog of Q.R.S Recorda Reproducing Player Rolls Complete to February 19 27 The individual recordings of the world's most famous concert pianists are included in this catalog. Recordo Rolls will also play on any standard 88 note player piano with. out any change. Manufactu red by THE Q.RS MUSIC C OMPANY NEW YORK CHICAGO SAN FRANCiSCO TORONTO, CANADA _ SIDNEY, AUSTRAUA Printed in U. S. A. " INTRODUCTORY USIc. wh ile it is the univer-sa l lang uag e. is s poken with different accents. As the S out her ner's slow, M mell ow intonations differ fr om the typical Eas t ern speech and the Western drawl, the interpretation s famous musician s place on identical com positi ons are essentially different. Li sten to any well known classic rendered by different artist s and yo u will ob serve that each ar -ti st will play it i ll his OWI1 style and feeling, which proves that mu sical interpretations, like faces, are never just alike . This graphically depicts t he real value of t he RECO RDO HEPRODCCfNG HO LLS. T hey arc positive reproduc tions of the technique and interpretation of the artist who played them-a musical pho tograph of his artistry. In Reccrdo Catalogs and Bulletins you will find the work of every g reat pianist. Yo u ma y take one number, inter preted by se veral different masters, and be as tonished at the difference ; these rolls breathe the fi re, the artistry. the very sp irit of th e ones who played them. -

The SMU Campus, Volume 36, Number 28, February 10, 1951
Council Announces Special Elections •osl® :• * To Fill Six Offices ! , ' '• "• .•'V;:.-?vVY A special election to replace editor elected in the special ejec the head cheerleader, associate edi tion would be replaced in the •Trxim tor of The Campus arid four Coun coming spring election. Fooshee pointed out that the constitution is cil members will be held within X.',. vague on the term of an associate V-'j'-c?;;'2''; three weeks, the. Student Council editor elected at a special election. decided Thursday. ; . - Two new members were elected Dick Wilke, chairman of the by the Council to serve on the so election committee, said that an cial: committee. Jane Allmari arid election code will be presented to Gordon Hosford will join Jane the Council at next Thursday's Hodge and Norman Cohen on the meeting. group which directs the social The position of head cheerleader affairs of religious, social and hono was left open when Marc Moore rary organizations on the campus. graduated at mid-term. Moore A motion to name a parliamen went to active duty in the Marine tarian to replace Dave Ilanlon, who Corps immediately after 'gradu acted as such for the Council, was K'- ation. tabled until a representative from •/•••v.'. The associate editorship' was the law , school was elected in the •; v vacated when Richard Vann re coming special election. Fhotos by Laughead placed Ardis Vancleave, who failed An appropriation was approved SWARM OF B'S to meet academic requirements for for $18 for-expenses on a trip to «*-:• Three girls at the wrong end of the alphabet for registration purposes beseech the PE department the editorship. -

Introductory Chapter Is Chapter 2, in Which I Survey Guion’S Radio Shows
Copyright by Mark David Camann 2010 1 The Dissertation Committee for Mark David Camann certifies that this is the approved version of the following dissertation: DAVID GUION’S VISION FOR A MUSICAL AMERICANA Committee: ____________________________ Elliott Antokoletz, Supervisor ____________________________ Rebecca Baltzer ____________________________ Lorenzo Candelaria ____________________________ Kevin Mooney ____________________________ Edward Pearsall 2 DAVID GUION’S VISION FOR A MUSICAL AMERICANA by Mark David Camann, B.A., M.A. Dissertation Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas at Austin December, 2010 3 ACKNOWLEDGEMENTS In my research on this topic I have been assisted by many people to whom I wish to express my gratitude. On my first visit to David Guion’s hometown, Billie Smithson at the Ballinger Chamber of Commerce provided me with a biographical sketch of the composer written by the composer’s sister. I had the privilege of meeting with Neuman Smith, former chairman of the Runnels County Historical Commission in composer David Guion’s hometown of Ballinger, Texas, and his wife Barbara, who had written the Centennial Edition of the Ballinger Ledger, of which she gave me one of her two remaining copies. Through their assistance I met David Albright, at that time the chairman of that same Historical Commission, who gave me a tour of the city and who helped me greatly in a search for a certain church on a certain alley mentioned in the sheet music of a Guion composition, and together we came to the realization that if Ballinger were indeed the unnamed Southern town mentioned in the preface to this song, then surely both the church and the alley were fictitious. -

Download Program
About Kaleidoscope MusArt KaleidoscopeMusArt is a 501(c)(3) non-profit organization dedicated to promoting classical music as a relevant and evolving art form, through innovative concert programs and educational initiatives that explore links between new, rarely-heard, and well-known works while prominently featuring emerging artists and living composers. Inesa Gegprifti, President*^ Redi Llupa, Vice-President*^ Our goals are to: Akina Yura, Treasurer*^ Make artistic experience accessible and affordable to a broad and diverse audience. Cultivate the appreciation of classical music among young generations. Board of Directors Support living composers through commissions and calls for scores. Maria Sumareva, Chair*^ Showcase the plurality of styles found in classical music throughout time and across cultures. Emiri Nourishirazi, Secretary Support young artists under the age of 18 by creating and facilitating access to Ermir Bejo educational and performing opportunities. Rodrigo Bussad^ Contribute to building an inclusive classical music community that upholds the Luca Cubisino principles of equality, fairness, and non-discrimination. Ricardo Lewitus Andrew Rosenblum Kaleidoscope MusArt was born out of the necessity of making contemporary piano music *Artistic/Executive Committee an integral part of the classical concert experience. Our distinctive approach to ^KMA Co-Founders programming draws connections between standard and contemporary repertoire in thematic concerts, exploring a spectrum of stylistic and aesthetic perspectives. The Volunteer & Blog Contributor: format of our concerts incorporates brief presentations about the works performed, Gianna Milan catalyzing a stronger connection between the audience and the music. By engaging Volunteer: young artists to perform new and rarely-heard works we aim to stimulate their Anna Gryshyna continuous curiosity and active advocacy for the contemporary repertoire. -

Master Thesis Optimisation of Treatment Time in Ultrasound Guided High Intensity Focused Ultrasound (HIFU) in the Treatment of Breast Fibroadenomata
CONFIDENTIAL Master Thesis Optimisation of Treatment Time in Ultrasound guided High Intensity Focused Ultrasound (HIFU) in the Treatment of Breast Fibroadenomata. Mirjam Peek, BSc Master Thesis Technical Medicine Faculty of Science and Technology December 5th, 2014 Optimisation of Treatment Time in Ultrasound guided High Intensity Focused Ultrasound (HIFU) in the Treatment of Breast Fibroadenomata. By Mirjam Peek, BSc S0200441 Master Thesis Technical Medicine Faculty of Science and Technology [email protected] [email protected] Graduation date: December 5th 2014 Graduation Committee: Chairman: Prof. Wiendelt Steenbergen [email protected] Medical Supervisor: Dr. Mr. Michael Douek [email protected] Technical Supervisors University of Twente: Dr. Ir. Bennie ten Haken [email protected] Guy’s hospital: Dr. Muneer Ahmed [email protected] External Supervisor: Dr. Srirang Manohar [email protected] Process Supervisor: Drs. Paul van Katwijk [email protected] THIS THESIS AND THE INFORMATION IN IT ARE PROVIDED IN CONFIDENCE AND MAY NOT BE DISCLOSED TO ANY THIRD PARTY OR USED FOR ANY OTHER PURPOSE WITHOUT THE WRITTEN PERMISSION OF THE AUTHOR UNTILL DECEMBER 5TH 2015. ii Preface In December 2013 I started my Technical Medicine graduation on the HIFU-F project at Guy's and St. Thomas' hospitals after a previous three month internship in London. This thesis reports the results of the work I performed in the last 12 months for the master in Technical Medicine. Firstly, I would like to thank my medical supervisor, Michael Douek, for giving me the opportunity to do my graduation in London.