Urgent Care Pearls
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Trauma Treating Traumatic Facial Nerve Paralysis
LETTERS TO EDITOR 205 206 LETTERS TO EDITOR In conclusion, the most frequent type of HBV R. Hepatitis B virus genotype A is more often hearing loss, and an impedance audiogram Strands of facial nerve interconnect with genotype in our study was D type, which associated with severe liver disease in northern showed absent stapedial reflex. CT scan cranial nerves V, VIII, IX, X, XI, and XII and usually causes a mild liver disease. Hence India than is genotype D. Indian J Gastroenterol showed no fracture of the temporal bone and with the cervical cutaneous nerves. This free proper vaccination, e ducational programs, 2005;24:19-22. intact ossicles. The patient was prescribed intermingling of Þ bers of the facial nerve with and treatment with lamivudine are efficient 6. Thakur V, Sarin SK, Rehman S, Guptan RC, high-dose steroids, along with vigorous facial Þ bers of other neural structures (particularly Kazim SN, Kumar S. Role of HBV genotype strategies in controlling HBV infection in our nerve stimulation and massages. the cranial nerve V) has been proposed as in predicting response to lamivudine therapy area. the mechanism of spontaneous return of facial in patients with chronic hepatitis B. Indian J After 3 weeks of treatment, the facial nerve nerve function after peripheral injury to the Gastroenterol 2005;24:12-5. stimulation tests were repeated and the ABDOLVAHAB MORADI, nerve.[4] VAHIDEH KAZEMINEJHAD1, readings were compared to those taken prior to GHOLAMREZA ROSHANDEL, treatment. There was negligible improvement. KHODABERDI KALAVI, Early onset/complete palsy indicates disruption EZZAT-OLLAH GHAEMI2, SHAHRYAR SEMNANI The patient was offered an exploratory of continuity of the nerve. -

Middle Ear Disorders
3/2/2014 ENT CARRLENE DONALD, MMS PA-C ANTHONY MENDEZ, MMS PA-C MAYO CLINIC ARIZONA DEPARTMENT OF OTOLARYNGOLOGY AND HEAD & NECK SURGERY No Disclosures OBJECTIVES • 1. Identify important anatomic structures of the ears, nose, and throat • 2. Assess and treat disorders of the external, middle and inner ear • 3. Assess and treat disorders of the nose and paranasal sinuses • 4. Assess and treat disorders of the oropharynx and larynx • 5. Educate patients on the risk factors for head and neck cancers 1 3/2/2014 Otology External Ear Disorders External Ear Anatomy 2 3/2/2014 Trauma • Variety of presentations. • Rule out temporal bone trauma (battle’s sign & hemotympanum). CT head w/out contrast. • Tx lacerations/avulsions with copious irrigation, closure with dissolvable sutures (monocryl), tetanus update, and antibiotic coverage (anti- Pseudomonal). May need to bolster if concerned for a hematoma . Auricular Hematoma • Due to blunt force trauma. • Drain/aspirate, cover with anti- biotics (anti- Pseudomonals), and apply bolster or passive drain if needed. • Infection and/or cauliflower ear may result if not treated. Chondritis • Inflammation and infection of the auricular cartilage. usually due to Pseudomonas aeruginosa. • Cultures • Treat with empiric antibiotics (anti-Pseudomonal) and I&D if needed. • Differentiate from relapsing polychondritis, which is an autoimmune disorder. 3 3/2/2014 External Auditory Canal Foreign Body • Children –Foreign bodies • Adults – Cerumen plugs • May present with hearing loss, ear pain and drainage • Exam under microscopic otoscopy. Check for otitis externa. • Remove under direct visualization. Can try to neutralize bugs with mineral oil. Do not attempt to irrigate organic material with water as this may cause an infection. -
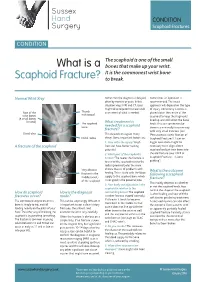
What Is a Scaphoid Fracture?
Sussex Hand CONDITION Surgery Scaphoid Fractures CONDITION The scaphoid is one of the small What is a bones that make up your wrist. It is the commonest wrist bone Scaphoid Fracture? to break. Normal Wrist Xray Sometimes the diagnosis is delayed, Sometimes an operation is often by months or years. In this recommended. The exact situation xrays, MRI and CT scans approach will depend on the type might all be required to make a full of injury. Commonly a screw is Rest of the Thumb assessment of what is needed. placed down the centre of the metacarpal wrist bones scaphoid to keep the fragments (8 small bones lined up and still whilst the bone in total) The scaphoid What treatment is heals. This can sometimes be bone needed for a scaphoid done in a minimally invasive way fracture? with very small incisions (see Distal ulna This depends on a great many ‘Percutaneous screw fixation of Distal radius things. Some important factors are: Scaphoid Fractures’). Later on 1. How old is the injury? Fresh bigger operations might be A fracture of the scaphoid fractures have better healing necessary to re-align a bent potential scaphoid and put new bone into 2. Which part of the scaphoid is the old fracture (see ‘ORIF of broken? The nearer the fracture is Scaphoid Fractures +/-bone to end of the scaphoid next to the grafting’). radius (proximal pole) the more Very obvious chance there is of problems with What is the outcome fracture in the healing. This is to do with the blood following a scaphoid middle (waist) supply to the scaphoid bone which fracture? of the scaphoid is not good in the proximal pole. -
EM Cases Digest Vol. 1 MSK & Trauma
THE MAGAZINE SERIES FOR ENHANCED EM LEARNING Vol. 1: MSK & Trauma Copyright © 2015 by Medicine Cases Emergency Medicine Cases by Medicine Cases is copyrighted as “All Rights Reserved”. This eBook is Creative Commons Attribution-NonCommercial- NoDerivatives 3.0 Unsupported License. Upon written request, however, we may be able to share our content with you for free in exchange for analytic data. For permission requests, write to the publisher, addressed “Attention: Permissions Coordinator,” at the address below. Medicine Cases 216 Balmoral Ave Toronto, ON, M4V 1J9 www.emergencymedicinecases.com This book has been authored with care to reflect generally accepted practices. As medicine is a rapidly changing field, new diagnostic and treatment modalities are likely to arise. It is the responsibility of the treating physician, relying on his/her experience and the knowledge of the patient, to determine the best management plan for each patient. The author(s) and publisher of this book are not responsible for errors or omissions or for any consequences from the application of the information in this book and disclaim any liability in connection with the use of this information. This book makes no guarantee with respect to the completeness or accuracy of the contents within. OUR THANKS TO... EDITORS IN CHIEF Anton Helman Taryn Lloyd PRODUCTION EDITOR Michelle Yee PRODUCTION MANAGER Garron Helman CHAPTER EDITORS Niran Argintaru Michael Misch PODCAST SUMMARY EDITORS Lucas Chartier Keerat Grewal Claire Heslop Michael Kilian PODCAST GUEST EXPERTS Andrew Arcand Natalie Mamen Brian Steinhart Mike Brzozowski Hossein Mehdian Arun Sayal Ivy Cheng Sanjay Mehta Laura Tate Walter Himmel Jonathan Pirie Rahim Valani Dave MacKinnon Jennifer Riley University of Toronto, Faculty of Medicine EM Cases is a venture of the Schwartz/ Reisman Emergency Medicine Institute. -
Final Program N
XXII Congress The International Society on Thrombosis and Haemostasis B July 11-16 2009 O 55th Annual Meeting S of the Scientific and Standardization Committee of the ISTH T O Final Program N Boston - July 11-16 2009 XXII Congress of the International Society on Thrombosis and Haemostasis 2009 Table ISTH of Contents Venue and Contacts 2 Wednesday 209 Welcome Messages 3 – Plenary Lectures 210 Committees 7 – State of the Art Lectures 210 Congress Awards and Grants 15 – Abstract Symposia Lectures 212 Other Meetings 19 – Oral Communications 219 – Posters 239 ISTH Information 20 Program Overview 21 Thursday 305 SSC Meetings and – Plenary Lectures 306 Educational Sessions 43 – State of the Art Lectures 306 – Abstract Symposia Lectures 309 Scientific Program 89 – Oral Communications 316 Monday 90 – Posters 331 – Plenary Lectures 90 Nursing Program 383 – State of the Art Lectures 90 Special Symposia 389 – Abstract Symposia Lectures 92 Satellite Symposia 401 – Oral Communications 100 – Posters 118 Technical Symposia Sessions 411 Exhibition and Sponsors 415 Tuesday 185 – Plenary Lectures 186 Exhibitor and Sponsor Profiles 423 – State of the Art Lectures 186 Congress Information 445 – Abstract Symposia Lectures 188 Map of BCEC 446 – Oral Communications 196 Hotel and Transportation Information 447 ISTH 2009 Congress Information 452 Boston Information 458 Social Events 463 Excursions 465 Authors’ Index 477 1 Venue & Contacts Venue Boston Convention & Exhibition Center 415 Summer Street - Boston, Massachusetts 02210 - USA Phone: +1 617 954 2800 - Fax: +1 617 954 3326 The BCEC is only about 10 minutes by taxi from Boston Logan International Airport. The 2009 Exhibition is located in Hall A and B of the Exhibit Level of the BCEC, along with posters and catering. -

Approach to the Trauma Patient Will Help Reduce Errors
The Approach To Trauma Author Credentials Written by: Nicholas E. Kman, MD, The Ohio State University Updated by: Creagh Boulger, MD, and Benjamin M. Ostro, MD, The Ohio State University Last Update: March 2019 Case Study “We have a motor vehicle accident 5 minutes out per EMS report.” 47-year-old male unrestrained driver ejected 15 feet from car arrives via EMS. Vital Signs: BP: 100/40, RR: 28, HR: 110. He was initially combative at the scene but now difficult to arouse. He does not open his eyes, withdrawals only to pain, and makes gurgling sounds. EMS placed a c-collar and backboard, but could not start an IV. What do you do? Objectives Upon completion of this self-study module, you should be able to: ● Describe a focused rapid assessment of the trauma patient using an organized primary and secondary survey. ● Discuss the components of the primary survey. ● Discuss possible pathology that can occur in each domain of the primary survey and recommend treatment/stabilization measures. ● Describe how to stabilize a trauma patient and prioritize resuscitative measures. ● Discuss the secondary survey with particular attention to head/central nervous system (CNS), cervical spine, chest, abdominal, and musculoskeletal trauma. ● Discuss appropriate labs and diagnostic testing in caring for a trauma patient. ● Describe appropriate disposition of a trauma patient. Introduction Nearly 10% of all deaths in the world are caused by injury. Trauma is the number one cause of death in persons 1-50 years of age and results in significant life years lost. According to the National Trauma Data Bank, falls were the leading cause of trauma followed by motor vehicle collisions (MVCs) and firearm related injuries with an overall mortality rate of 4.39% in 2016. -

Joint Faculty of Intensive Care Medicine
Joint Faculty of Intensive Care Medicine Australian and New Zealand The Royal Australasian College of Anaesthetists College of Physicians ABN 82 055 042 852 Exam Report Oct 2009 This report is prepared to provide candidates, tutors and their supervisors of training with information about the way in which the Examiners assessed the performance of candidates in the Examination. Answers provided are not model answers but guides to what was expected. Candidates should discuss the report with their tutors so that they may prepare appropriately for the future examinations The exam included two 2.5 hour written papers comprising of 15 ten-minute short answer questions each. Candidates were required to score at least 50% in the written paper before being eligible to sit the oral part of the exam. The oral exam comprised 8 interactive vivas and two separate hot cases. This is the fourth examination with the new regulations which came into force in 2008. The tables below provide an overall statistical analysis as well as information regarding performance in the individual sections. A comparison with April 2008, October 2008 and April 2009 data is also provided. Examiner comments Written paper 1) Lack of specificity and precision in the answers. 2) Poor pass rate on clinical methods questions – suggests that candidates are not taking clinical examination seriously and they will need to read books like Talley and O’Connor thoroughly. 3) Candidates seem to score well largely on Data interpretation / OSCE type questions. The inability to score well on other questions reflects a general lack of preparation and knowledge even of common topics in intensive care. -

Scaphoid Fracture PA Radiograph
30 y/o male with acute left wrist pain Student Name….None was listed Atul Kumar, MD, MS PA Radiograph Non Contrast Coronal CT ? Scaphoid Fracture PA radiograph Distal pole Scaphoid fracture Proximal pole • PA x-ray showing transverse scaphoid fracture. Non Contrast Coronal CT Capitate Trapezoid Hamate Trapezium Triquetrum Lunate Scaphoid fracture Scaphoid Fracture • Mechanism: direct axial compression or with hyperextension (fall onto an outstretched hand). • Symptoms: pain localized at the radial aspect of wrist often associated with swelling and reduced grip strength. – Pain in anatomic snuffbox suspicious for waist fracture, which is the most common type. • Because scaphoid fractures are often radiologically occult, any tenderness in the anatomic snuffbox should be treated as a scaphoid fracture. • Scaphoid blood supply (palmar carpal branch of the radial artery) runs from the distal to the proximal pole. Transverse fracture of the proximal pole can lead to osteonecrosis and nonunion due to disruption of blood flow. http://epmonthly.com/wp-content/uploads/2016/04/OrthoB.png Scaphoid Fracture • Differential diagnosis: distal radius fracture, wrist sprain, and other carpal injuries other than scaphoid. • In suspected scaphoid fractures, plain radiographs (including PA, true lateral, oblique, and scaphoid views) are ordered as the first diagnostic step. • However, the false negative rate for radiographs taken immediately after injury up to 20-54%. • Definitive diagnosis can be made by MRI or CT scan. They have a comparable diagnostic accuracy and do not result in overtreatments. Avascular necrosis/Nonunion Scaphoid view radiograph (A) and CT scan (B) showing nonunion (arrow) and avascular necrosis (asterisk) and the Terry Thomas sign – scapholunate ligament injury (arrowhead). -

Wrist Injury Article 12-19-16
ARTICLE: Wrist Injuries This week we are going to talk about 3 unusual wrist injuries all of which can cause considerable problems and the potential complications of each. The first is a TFCC injury. The TFCC or triangular fibrocartilage is a small meniscus or pad on the ulnar side of the wrist (pinky side) which can become torn during a fall on an outstretched hand and can cause clicking, popping and pain on this side of the wrist. The TFCC is sometimes difficult to detect and often misdiagnosed as a wrist sprain but is rather different than a sprained wrist in that it is not an injury of ligament but is an injury of cartilage. The injury can be spotted with a shear test and is properly diagnosed with an arthrogram. The second unusual injury to the wrist is the scaphoid fracture. The scaphoid fracture of the wrist is a bone injury which occurs when the scaphoid bone on the radial side of the wrist (thumb side) is broken at it’s waist (center) injuring the blood supply to the proximal pole of the scaphoid. This injury results in avascular necrosis or bone death of the scaphoid. Also occurring after a fall on an outstretched hand the scaphoid fracture is often misdiagnosed as a wrist sprain but is more correctly described as a fracture. The hallmark symptom of a scaphoid fracture is it’s failure to heal and persistent pain on the radial side of the wrist. The scaphoid fracture is often missed on the initial x-ray as the bone has not had time yet to die off and is often seen on a second film. -

Your Wrist Bones
www.healthinfo.org.nz Your wrist bones Your wrist is made up of eight small bones (called the carpal bones). Each carpal bone has a specific name, shown in the image on the right. The carpal bones connect with the two long bones in your forearm (the radius and ulna). Your wrist moves where they connect. This makes your wrist a very complex structure, as there are many different joints within it. If any one of your carpal bones breaks, it can change position slightly, causing pain and problems with movement. Occasionally it can also lead to arthritis. Causes of a broken wrist A broken wrist usually happens from falling on to an outstretched hand. Serious accidents, such as car accidents, motorcycle accidents, or falls from a ladder cause more serious breaks. Weak bones (for example, in someone with osteoporosis) tend to break more easily. If you break your wrist without significant force, your doctor may recommend checking if you have osteoporosis. If you meet the criteria, they may send you for a bone density scan. Any one of the 10 bones in your wrist can break, but the most common bone to break is the radius, in your forearm. This is called a distal radius fracture. Another common wrist fracture is a scaphoid fracture, which is a break in one of your small carpal bones. This can be difficult to diagnose, and there is a risk a scaphoid fracture might not heal. Your wrist can break in many different ways, and some breaks are worse than others. How bad a break it is depends on how many pieces a bone breaks into, whether they are stable or move around a lot, and whether the broken ends of the bone are still in the right place. -

Imaging and Treatment of Scaphoid Fractures and Their Complications
159 Imaging and Treatment of Scaphoid Fractures and Their Complications Mihra S. Taljanovic, M.D., M.Sc., F.A.C.R. 1 Apostolos Karantanas, M.D., Ph.D. 2, 3 James F. Griffith, M.D. 4 Gregory L. DeSilva, M.D. 5 Joshua D. Rieke, M.D. 1 Joseph E. Sheppard, M.D. 5 1 Department of Medical Imaging, The University of Arizona Health Address for correspondence and reprint requests Mihra S. Taljanovic, Network, Tucson, Arizona. M.D., M.Sc., Department of Medical Imaging, The University of Arizona 2 Department of Radiology, University of Crete, Heraklion, Greece. Health Network, 1501 N. Campbell Ave., Tucson, AZ 85724-5067 3 Department of Medical Imaging, University Hospital, Heraklion, (e-mail: [email protected]). Greece. 4 Department of Imaging and Interventional Radiology, Prince of Wales Hospital, Shatin, New Territories, Hong Kong. 5 Department of Orthopaedic Surgery, The University of Arizona Health Network, Tucson, Arizona. Semin Musculoskelet Radiol 2012;16:159–174. Abstract The scaphoid is the most commonly fractured carpal bone, with frequent complications that are predisposed by its anatomical location, anatomical configuration (shape and length), and vascular supply. The most common mechanism of injury is a fall onto an outstretched hand. Imaging plays a significant role in the initial evaluation and treatment of scaphoid fractures and their complications. Radiography should be the first imaging modality in the initial evaluation and follow-up of scaphoid fractures. Computed tomography with its superb spatial resolution enables better visualization and charac- terization of the fracture line, and the amount of displacement and angulation of the fracture fragments. -

Section J: Trauma J
Section J: Trauma J Clinical/Diagnostic Investigation Recommendation Dose Comment Problem (Grade) Head J01. Head injury SXR Not indicated [B] d There is poor correlation between the presence of a skull fracture and a clinically significant head injury. The only (For children see indications for skull x-rays in the setting of trauma are Section L) suspected open or depressed skull fractures, if CT is not available and suspected child abuse. Section J: Trauma CT Indicated [A] dd CT is indicated in all patients with a severe head injury (GCS <13). In patients with a minor head injury (GCS 13-15 and witnessed loss of consciousness or disorientation or definite amnesia) CT is indicated to rule out an injury requiring neurosurgical intervention if there is: • GCS <15 2 hours after the injury • Suspected open or depressed skull fracture • Any sign of a basal skull fracture • Two or more episodes of vomiting • Age > 65 years To rule out any other clinically significant intracranial injury, the following additional risk factors justify obtaining CT: • Amnesia for before the impact lasting > 30 minutes • Dangerous mechanism of injury (motor vehicle accident or fall from> 3 feet or 5 stairs or more). CTA Specialized dd CTA should be performed with presentation of high energy Investigation [B] transfer mechanism or if associated with any of the following: • Displaced mid-face fracture • Basilar skull fracture with carotid canal involvement • Focal neurological deficit • Cervical vertebral body or transverse foramen fracture • Fracture at C1-C3 • Clothesline type injury or seat belt abrasion with significant swelling/pain • Altered mental status Face and orbits J02.