Comparison of Computed Tomographic and Magnetic Resonance Imaging in Fracture Healing After Spinal Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Computed Tomography (CT) National Institutes of Health
NATIONAL INSTITUTE OF BIOMEDICAL IMAGING AND BIOENGINEERING Computed Tomography (CT) National Institutes of Health What is a computed tomography (CT) scan? The term “computed tomography”, or CT, refers to a computerized x-ray imaging procedure in which a narrow beam of x-rays is aimed at a patient and quickly rotated around the body, producing signals that are processed by the machine’s computer to generate cross- sectional images—or “slices”—of the body. These slices are called tomographic images and contain more detailed information than conventional x-rays. Once a number of successive slices are collected by the machine’s computer, they can be digitally “stacked” together Source: Terese Winslow to form a three-dimensional image of the patient that allows for easier identification and location of basic structures as well as possible tumors or abnormalities. How does CT work? Unlike a conventional x-ray—which uses a fixed x-ray tube—a CT scanner uses a motorized x-ray source that rotates around the circular opening of a donut-shaped structure called a gantry. During a CT scan, the patient lies on a bed that slowly moves through the gantry while the x-ray tube rotates around the patient, shooting narrow beams of x-rays through the body. Instead of film, CT scanners use special digital x-ray detectors, which are located directly opposite the x-ray source. As the x-rays leave the patient, they are picked up by the detectors and transmitted to a computer. Each time the x-ray source completes one full rotation, the CT computer uses sophisticated mathematical techniques to construct a 2D image slice of the patient. -

Acr–Nasci–Sir–Spr Practice Parameter for the Performance and Interpretation of Body Computed Tomography Angiography (Cta)
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2021 (Resolution 47)* ACR–NASCI–SIR–SPR PRACTICE PARAMETER FOR THE PERFORMANCE AND INTERPRETATION OF BODY COMPUTED TOMOGRAPHY ANGIOGRAPHY (CTA) PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

Optical Coherence Tomography (OCT) Anterior Segment of the Eye
Corporate Medical Policy Optical Coherence Tomography (OCT) Anterior Segment of the Eye File Name: optical_coherence_tomography_(OCT)_anterior_segment_of_the_eye Origination: 2/2010 Last CAP Review: 6/2021 Next CAP Review: 6/2022 Last Review: 6/2021 Description of Procedure or Service Optical Coherence Tomography Optical coherence tomography (OCT) is a noninvasive, high-resolution imaging method that can be used to visualize ocular structures. OCT creates an image of light reflected from the ocular structures. In this technique, a reflected light beam interacts with a reference light beam. The coherent (positive) interference between the 2 beams (reflected and reference) is measured by an interferometer, allowing construction of an image of the ocular structures. This method allows cross-sectional imaging a t a resolution of 6 to 25 μm. The Stratus OCT, which uses a 0.8-μm wavelength light source, was designed to evaluate the optic nerve head, retinal nerve fiber layer, and retinal thickness in the posterior segment. The Zeiss Visante OCT and AC Cornea OCT use a 1.3-μm wavelength light source designed specifically for imaging the a nterior eye segment. Light of this wa velength penetrates the sclera, a llowing high-resolution cross- sectional imaging of the anterior chamber (AC) angle and ciliary body. The light is, however, typically blocked by pigment, preventing exploration behind the iris. Ultrahigh resolution OCT can achieve a spatial resolution of 1.3 μm, allowing imaging and measurement of corneal layers. Applications of OCT OCT of the anterior eye segment is being eva luated as a noninvasive dia gnostic and screening tool with a number of potential a pplications. -

Breast Tomosynthesis: the New Age of Mammography Tomosíntesis: La Nueva Era De La Mamografía
BREAST TOMOSYNTHESIS: THE NEW AGE OF MAMMOGRAPHY TOMOSÍNTESIS: LA NUEVA ERA DE LA MAMOGRAFÍA Gloria Palazuelos1 Stephanie Trujillo2 Javier Romero3 SUMMARY Objective: To evaluate the available data of Breast Tomosynthesis as a complementary tool of direct digital mammography. Methods: A systematic literature search of original and review articles through PubMed was performed. We reviewed the most important aspects of Tomosynthesis in breast imaging: Results: 36 Original articles, 13 Review articles and the FDA and American College of Radiology standards were included. Breast Tomosynthesis has showed a positive impact in breast cancer screening, improving the rate of cancer detection EY WORDS K (MeSH) due to visualization of small lesions unseen in 2D (such as distortion of the architecture) Mammography Tomography and it has greater precision regarding tumor size. In addition, it improves the specificity of Diagnosis mammographic evaluation, decreasing the recall rate. Limitations: Interpretation time, cost and Breast neoplasms low sensitivity to calcifications.Conclusions : Breast Tomosynthesis is a new complementary tool of digital mammography which has showed a positive impact in breast cancer diagnosis in comparison to the conventional 2D mammography. Decreased recall rates could have PALABRAS CLAVE (DeCS) significant impact in costs, early detection and a decrease in anxiety. Mamografía Tomografía Diagnóstico RESUMEN Neoplasias de la mama Objetivo: Evaluar el estado del arte de la tomosíntesis como herramienta complementaria de la mamografía digital directa. Metodología: Se realizó una búsqueda sistemática de la literatura de artículos originales y de revisión a través de PubMed. Se revisaron los aspectos más importantes en cuanto a utilidad y limitaciones de la tomosíntesis en las imágenes de mama. -
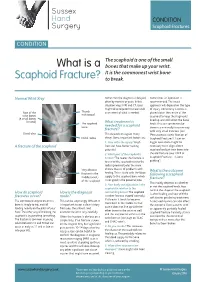
What Is a Scaphoid Fracture?
Sussex Hand CONDITION Surgery Scaphoid Fractures CONDITION The scaphoid is one of the small What is a bones that make up your wrist. It is the commonest wrist bone Scaphoid Fracture? to break. Normal Wrist Xray Sometimes the diagnosis is delayed, Sometimes an operation is often by months or years. In this recommended. The exact situation xrays, MRI and CT scans approach will depend on the type might all be required to make a full of injury. Commonly a screw is Rest of the Thumb assessment of what is needed. placed down the centre of the metacarpal wrist bones scaphoid to keep the fragments (8 small bones lined up and still whilst the bone in total) The scaphoid What treatment is heals. This can sometimes be bone needed for a scaphoid done in a minimally invasive way fracture? with very small incisions (see Distal ulna This depends on a great many ‘Percutaneous screw fixation of Distal radius things. Some important factors are: Scaphoid Fractures’). Later on 1. How old is the injury? Fresh bigger operations might be A fracture of the scaphoid fractures have better healing necessary to re-align a bent potential scaphoid and put new bone into 2. Which part of the scaphoid is the old fracture (see ‘ORIF of broken? The nearer the fracture is Scaphoid Fractures +/-bone to end of the scaphoid next to the grafting’). radius (proximal pole) the more Very obvious chance there is of problems with What is the outcome fracture in the healing. This is to do with the blood following a scaphoid middle (waist) supply to the scaphoid bone which fracture? of the scaphoid is not good in the proximal pole. -
EM Cases Digest Vol. 1 MSK & Trauma
THE MAGAZINE SERIES FOR ENHANCED EM LEARNING Vol. 1: MSK & Trauma Copyright © 2015 by Medicine Cases Emergency Medicine Cases by Medicine Cases is copyrighted as “All Rights Reserved”. This eBook is Creative Commons Attribution-NonCommercial- NoDerivatives 3.0 Unsupported License. Upon written request, however, we may be able to share our content with you for free in exchange for analytic data. For permission requests, write to the publisher, addressed “Attention: Permissions Coordinator,” at the address below. Medicine Cases 216 Balmoral Ave Toronto, ON, M4V 1J9 www.emergencymedicinecases.com This book has been authored with care to reflect generally accepted practices. As medicine is a rapidly changing field, new diagnostic and treatment modalities are likely to arise. It is the responsibility of the treating physician, relying on his/her experience and the knowledge of the patient, to determine the best management plan for each patient. The author(s) and publisher of this book are not responsible for errors or omissions or for any consequences from the application of the information in this book and disclaim any liability in connection with the use of this information. This book makes no guarantee with respect to the completeness or accuracy of the contents within. OUR THANKS TO... EDITORS IN CHIEF Anton Helman Taryn Lloyd PRODUCTION EDITOR Michelle Yee PRODUCTION MANAGER Garron Helman CHAPTER EDITORS Niran Argintaru Michael Misch PODCAST SUMMARY EDITORS Lucas Chartier Keerat Grewal Claire Heslop Michael Kilian PODCAST GUEST EXPERTS Andrew Arcand Natalie Mamen Brian Steinhart Mike Brzozowski Hossein Mehdian Arun Sayal Ivy Cheng Sanjay Mehta Laura Tate Walter Himmel Jonathan Pirie Rahim Valani Dave MacKinnon Jennifer Riley University of Toronto, Faculty of Medicine EM Cases is a venture of the Schwartz/ Reisman Emergency Medicine Institute. -

Thermography) for Population Screening and Diagnostic Testing of Breast Cancer
NZHTA TECH BRIEF SERIES July 2004 Volume 3 Number 3 Review of the effectiveness of infrared thermal imaging (thermography) for population screening and diagnostic testing of breast cancer Jane Kerr New Zealand Health Technology Assessment Department of Public Health and General Practice Christchurch School of Medicine Christchurch, NZ. Division of Health Sciences, University of Otago NEW ZEALAND HEALTH TECHNOLOGY ASSESSMENT (NZHTA) Department of Public Health and General Practice Christchurch School of Medicine and Health Sciences Christchurch, New Zealand Review of the effectiveness of infrared thermal imaging (thermography) for population screening and diagnostic testing of breast cancer Jane Kerr NZHTA TECH BRIEF SERIES July 2004 Volume 3 Number 3 This report should be referenced as follows: Kerr, J. Review of the effectiveness of infrared thermal imaging (thermography) for population screening and diagnostic testing of breast cancer. NZHTA Tech Brief Series 2004; 3(3) Titles in this Series can be found on the NZHTA website: http://nzhta.chmeds.ac.nz/thermography_breastcancer.pdf 2004 New Zealand Health Technology Assessment (NZHTA) ISBN 1-877235-64-4 ISSN 1175-7884 i ACKNOWLEDGEMENTS This Tech Brief was commissioned by the National Screening Unit of the New Zealand Ministry of Health. The report was prepared by Dr Jane Kerr (Research Fellow) who selected and critically appraised the evidence. The research protocol for this report was developed by Ms Marita Broadstock (Research Fellow). The literature search strategy was developed and undertaken by Mrs Susan Bidwell (Information Specialist Manager). Mrs Ally Reid (Administrative Secretary) provided document formatting. Internal peer review was provided by Dr Robert Weir (Senior Research Fellow), Dr Ray Kirk (Director) and Ms Broadstock. -

Learn More About X-Rays, CT Scans and Mris (Pdf)
What is the difference between X-Rays, CT Scans, and MRIs? X-Rays are a form of electromagnetic radiation, like light. They are less energetic than gamma rays, and more energetic than ultraviolet light. Because they pass easily through soft tissue, like organs and muscles, but not so easily through hard tissue like bones and teeth, we are most familiar with them being used to look at skeletal structures. Sometimes a person ingests or has injected an X-ray opaque fluid that will fill a space of interest for X-ray imaging. This is called an angiogram. A nuclear scan uses an injected gamma ray emitting substance that accumulates in the organ of interest and a special camera records the gamma rays. A CT Scan is usually a series of X-rays taken from different directions that are then assembled into a three dimensional model of the subject in a computer. CT stands for computed tomography, and tomography means a picture of a slice. Where an X-ray may show edges of soft tissues all stacked on top of each other, the computer in a CT scan can figure out how those edges relate to each other in depth, and so the image has much more soft tissue usability. Another kind of CT scan uses positrons. I have to mention this because positrons are antimatter electrons (Yes, antimatter does exist and it is useful!) In Positon Emission Tomography (PET) a positron emitting radionuclide (radioactive material) is attached to a metabolically useful molecule. This is introduced to the tissue, and as emitted positrons decompose they emit gamma rays which can be traced by the machine and computer back to their points of origin, and an image is formed. -

Ijp 18 5 Coward 8.Pdf
Coward 8/25/05 1:54 PM Page 405 A Comparison Between Computerized Tomography, Magnetic Resonance Imaging, and Laser Scanning for Capturing 3-Dimensional Data from an Object of Standard Form Trevor J. Coward, PhD, MPhila/Brendan J. J. Scott, BDS, BSc, PhD, FDSRCS (Ed)b/ Roger M. Watson, BDS, MDS, FDSRCSc/Robin Richards, BSc, MSc, PhDd Purpose: The study’s aim was to compare dimensional measurements on computer images generated from data captured digitally by 3 different methods of the surfaces of a plastic cube of known form to those obtained directly from the cube itself. Materials and Methods: Three-dimensional images were reconstructed of a plastic cube obtained by computerized tomography (CT), magnetic resonance imaging (MRI), and laser scanning. Digital calipers were used to record dimensional measurements be- tween the opposing faces of the plastic cube. Similar dimensional measurements were recorded between the cube faces on each of the reconstructed images. The data were analyzed using a 2-way ANOVA to determine whether there were differences between dimensional measurements on the computer images generated from the digitization of the cube surfaces by the different techniques, and the direct measurement of the cube itself. Results: A significant effect of how the measurements were taken (ie, direct, CT, MRI, and laser scanning) on the overall variation of dimensional measurement (P < .0005) was observed. Post hoc tests (Bonferroni) revealed that these differences were due principally to differences between the laser-scanned images compared to other sources (ie, direct, CT, and MRI). The magnitude of these differences was very small, up to a maximum mean difference of 0.71 mm (CI ± 0.037 mm). -

Positron Emission Tomography
Positron emission tomography A.M.J. Paans Department of Nuclear Medicine & Molecular Imaging, University Medical Center Groningen, The Netherlands Abstract Positron Emission Tomography (PET) is a method for measuring biochemical and physiological processes in vivo in a quantitative way by using radiopharmaceuticals labelled with positron emitting radionuclides such as 11C, 13N, 15O and 18F and by measuring the annihilation radiation using a coincidence technique. This includes also the measurement of the pharmacokinetics of labelled drugs and the measurement of the effects of drugs on metabolism. Also deviations of normal metabolism can be measured and insight into biological processes responsible for diseases can be obtained. At present the combined PET/CT scanner is the most frequently used scanner for whole-body scanning in the field of oncology. 1 Introduction The idea of in vivo measurement of biological and/or biochemical processes was already envisaged in the 1930s when the first artificially produced radionuclides of the biological important elements carbon, nitrogen and oxygen, which decay under emission of externally detectable radiation, were discovered with help of the then recently developed cyclotron. These radionuclides decay by pure positron emission and the annihilation of positron and electron results in two 511 keV γ-quanta under a relative angle of 180o which are measured in coincidence. This idea of Positron Emission Tomography (PET) could only be realized when the inorganic scintillation detectors for the detection of γ-radiation, the electronics for coincidence measurements, and the computer capacity for data acquisition and image reconstruction became available. For this reason the technical development of PET as a functional in vivo imaging discipline started approximately 30 years ago. -

Breast Imaging Faqs
Breast Imaging Frequently Asked Questions Update 2021 The following Q&As address Medicare guidelines on the reporting of breast imaging procedures. Private payer guidelines may vary from Medicare guidelines and from payer to payer; therefore, please be sure to check with your private payers on their specific breast imaging guidelines. Q: What differentiates a diagnostic from a screening mammography procedure? Medicare’s definitions of screening and diagnostic mammography, as noted in the Centers for Medicare and Medicaid’s (CMS’) National Coverage Determination database, and the American College of Radiology’s (ACR’s) definitions, as stated in the ACR Practice Parameter of Screening and Diagnostic Mammography, are provided as a means of differentiating diagnostic from screening mammography procedures. Although Medicare’s definitions are consistent with those from the ACR, the ACR's definitions of screening and diagnostic mammography offer additional insight into what may be included in these procedures. Please go to the CMS and ACR Web site links noted below for more in- depth information about these studies. Medicare Definitions (per the CMS National Coverage Determination for Mammograms 220.4) “A diagnostic mammogram is a radiologic procedure furnished to a man or woman with signs and symptoms of breast disease, or a personal history of breast cancer, or a personal history of biopsy - proven benign breast disease, and includes a physician's interpretation of the results of the procedure.” “A screening mammogram is a radiologic procedure furnished to a woman without signs or symptoms of breast disease, for the purpose of early detection of breast cancer, and includes a physician’s interpretation of the results of the procedure. -

PE310 PET / CT Scan
PET / CT Scan What is a PET A positron emission tomography (PET) scan is a safe and non-painful way scan? to take detailed images of the human body. PET scans show how the cells in your child’s body are working and using energy. Since changes in the way cells work often happen before changes in the way they look, a PET scan can help with early diagnosis of cancer, as well as diseases of the brain and heart. A CT (computed tomography) scan is done at the same time as the PET. The CT shows the location of the cells imaged on the PET. What are some PET/CT scans are used most often to find cancer or to check if cancer common uses of treatments are working. PET/CT scans of the brain are used to evaluate patients who have tumors or who have seizure problems that do not the PET/CT scan? respond to medical treatment and may need surgery. How do I prepare If we will be giving your child anesthesia, follow the instructions that the my child? nurse practitioner gives you. If your child has diabetes or needs to take insulin, please tell the technologist the night before the PET/CT scan. 1 of 3 To Learn More Free Interpreter Services • Radiology • In the hospital, ask your nurse. 206-987-2089 • From outside the hospital, call the • Ask your child’s healthcare provider toll-free Family Interpreting Line, 1-866-583-1527. Tell the interpreter • seattlechildrens.org the name or extension you need. PET / CT Scan For all other children: 24 hours before Your child should avoid exercise 24 hours before their PET/CT scan the scan because exercise may interfere with the images.