EM Cases Digest Vol. 1 MSK & Trauma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Episode 35 - Pediatric Orthopedics - Emergencymedicinecases.Com
EPISODE 35 - PEDIATRIC ORTHOPEDICS - EMERGENCYMEDICINECASES.COM KNEE INJURIES: Check the X-ray for a Segond fracture, a vertically oriented In general, children’s ligaments are avulsion fracture off the lateral stronger than their bones, thus proximal tibia. This is highly fractures are more likely than associated with ACL and meniscal sprains. Have a low threshold for tears. (See page 4 for a picture.) imaging if suspicious. Management of ACL tears: The same ACL-injury mechanism (sudden deceleration - pain management in acute phase of distal leg with forward and (NSAIDs, tylenol, morphine) rotatory movement) will cause a - short term immobilization (splint EPISODE 35: tibial spine fracture in a as needed, +/-crutches), but PEDIATRIC ORTHOPEDICS younger child, and an ACL tear in atrophy of quadriceps occurs WITH DR. SANJAY MEHTA & a teenager or adult. (See page 4 for quickly, so start range of motion in DR. JONATHAN PIRIE a photo of a tibial spine fracture.) 2–3 days. Some experts Patellar subluxations: the child Lachman test for ACL tear recommend weight bearing as may feel a “pop”, from the kneecap involves pulling the proximal tibia tolerated immediately. subluxing, and feel unstable on the anteriorly while holding the knee in - Surgical repair is delayed until leg. First time patella dislocations flexion. It has good sensitivity (>80% range of motion has recovered. and non-displaced fractures do and specificity of 95%) (1). The Refer to outpatient orthopedics. need knee immobilization, pivot shift test (valgus force and with weight bearing as tolerated. internal rotation to extended leg, Displaced fractures or fractures with which is then flexed to feel Additional X-ray views: an impaired extensor mechanism subluxation) is also sensitive for ACL - patellar injury requires a “skyline need urgent orthopedic tear. -

Ottawa Knee Rule: Investigating Use and Application in a Tertiary Teaching Hospital
Open Access Original Article DOI: 10.7759/cureus.8812 Ottawa Knee Rule: Investigating Use and Application in a Tertiary Teaching Hospital Abubakr Mohamed 1 , Elkhidir Babikir 1 , Mohamed Kamal Elbashir Mustafa 2 1. Emergency Medicine, University Hospital Galway, Galway, IRL 2. Vascular Surgery, University Hospital Galway, Galway, IRL Corresponding author: Abubakr Mohamed, [email protected] Abstract Background Knee injuries are encountered commonly in the emergency departments (EDs) in Ireland. Validated clinical decision rules such as Ottawa knee rule (OKR) can be used in acute knee injury settings to reduce the number of unnecessary radiography. Clinical judgment can be used to distinguish between suspected fractures and non-fractures in many cases; however, radiography is still routinely requested. Objectives We evaluated the OKRs in a high-volume tertiary teaching hospital in Ireland to determine whether the rule could be safely used to decide whether patients with acute blunt knee trauma should undergo radiography. Methods This was an observational study conducted in the ED over a three-month period in a tertiary referral hospital. A total of 110 patients with acute knee injuries were examined using OKR. Inclusion criteria included patients with acute knee injuries due to blunt trauma or twisting injury and patients with lacerations or contusions. Open fractures and fractures due to penetrating injury were excluded from the study. Results Fractures were seen in 12 (13.2%) of the 110 patents who met the inclusion criteria. The OKR predicted all 12 fractures. Sensitivity was 100%, and specificity was 39%. Conclusions Received 06/04/2020 Review began 06/18/2020 The OKR is highly sensitive for fracture in this setting and can be safely used to decide whether Review ended 06/21/2020 patients with acute blunt knee trauma should undergo radiography. -

1. MOA AAA 2016 Abstract
Abstract Combined Meeting of the th Malaysian Orthopaedic 46Association Annual General Meeting / Annual Scientific Meeting th ASEAN Arthroplasty 10 Association Meeting 2016 Fundamentals In Orthopaedics – Back To Basics Pre-Conference Day Conference Days 25th May 2016 26th to 28th May 2016 Persada Johor International Convention Centre, Johor Bahru, Malaysia. www.moa-home.com Abstract CD (Please click on the links below to view the respective categories of abstracts.) Oral Presentations Abstracts Poster Presentations Abstracts (Click Here...) Combined Meeting of the 46th Malaysian Orthopaedic Association Annual General Meeting / Annual Scientific Meeting & 10th ASEAN Arthroplasty Association Meeting 2016 26th May 2016 (Thursday) - Lecture Hall MOA 1, Level 3 TIME TOPIC SPEAKER 0700 -1730 REGISTRATION COUNTER OPENS SUBIR SENGUPTA MEMORIAL LECTURE Chairperson Prof Dr Saw Aik 0830 - 0900 Prevention And Early Detection Of DDH - The Japanese SM 01 Prof Dr Makoto Kamegaya Experience OPENING CEREMONY 0900 - 1030 Orthopaedics At The Frontlines In A Changing Globalised World. SK 01 Roles And Responsibilities. Dato' Dr Ahmad Faizal Mohd Perdaus A View From A Humanitarian And Colleauge. 1030 - 1100 TEA BREAK & EXHIBIT VISIT SPORTS Dr Shamsul Iskandar Hussein Chairperson Dr Raymond Yeak Dieu Kiat Revision Anterior Cruciate Ligament Reconstruction: Analysis 1100 - 1112 SX 01 Of Causes Of Failures, Preoperative Clinical Evaluation And Dr Deepak V. Patel Planning, Surgical Technique, And Clinical Outcomes SLAP (Superior Labrum Anterior Posterior) -

SPA Referral Guidelines
SUTTER PHYSICIANS ALLIANCE (SPA) 2800 L Street, 7th Floor Sacramento, CA 95816 SPA Specialty Referral Guideline Pittsburg Knee Rules for Ordering Radiology Ottawa Ankle Rules for Ordering Radiology Developed May 10, 2005 Revised April 23, 2007 Reviewed July 27, 2009 I. Indications for Ordering X-ray of the Knee.......................................Page 2 II. Indications for Ordering X-ray of the Ankle .....................................Page 2 III. Indications for Ordering X-ray of the Foot ........................................Page 2 IV. Exclusion Criterion for Ankle and Foot.............................................Page 2 SPA Specialty Referral Guideline – Pittsburg Knee / Ottawa Ankle Referral Indications Revised 4/23/07 Page 2 of 2 I. Indications for Ordering X-ray of the Knee Pittsburg Knee Rules/Indications for Ordering Plain Films of the Knee A) If the patient experienced a fall or blunt trauma, and is unable to walk four (4) weight- bearing steps, an X-ray is indicated. B) If the patient experienced a fall or blunt trauma, and is under 12 or over 50 years of age, an X-ray is indicated. If the above criteria are not present, no need for X-ray. II. Indications for Ordering X-ray of the Ankle Ottawa Ankle Rules Pain in the malleolar zone and ANY of the following: A) Bony tenderness at posterior edge of distal 6cm of the lateral malleolus. B) Bony tenderness at posterior edge of distal 6cm of the medial malleolus. C) Inability to weight-bear immediately. III. Indications for Ordering X-ray of the Foot Pain in the mid-foot zone and ANY of the following: A) Bony tenderness at the base of the 5th metatarsal. -
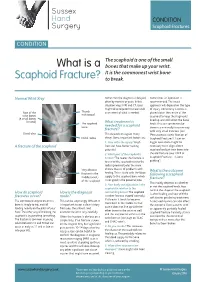
What Is a Scaphoid Fracture?
Sussex Hand CONDITION Surgery Scaphoid Fractures CONDITION The scaphoid is one of the small What is a bones that make up your wrist. It is the commonest wrist bone Scaphoid Fracture? to break. Normal Wrist Xray Sometimes the diagnosis is delayed, Sometimes an operation is often by months or years. In this recommended. The exact situation xrays, MRI and CT scans approach will depend on the type might all be required to make a full of injury. Commonly a screw is Rest of the Thumb assessment of what is needed. placed down the centre of the metacarpal wrist bones scaphoid to keep the fragments (8 small bones lined up and still whilst the bone in total) The scaphoid What treatment is heals. This can sometimes be bone needed for a scaphoid done in a minimally invasive way fracture? with very small incisions (see Distal ulna This depends on a great many ‘Percutaneous screw fixation of Distal radius things. Some important factors are: Scaphoid Fractures’). Later on 1. How old is the injury? Fresh bigger operations might be A fracture of the scaphoid fractures have better healing necessary to re-align a bent potential scaphoid and put new bone into 2. Which part of the scaphoid is the old fracture (see ‘ORIF of broken? The nearer the fracture is Scaphoid Fractures +/-bone to end of the scaphoid next to the grafting’). radius (proximal pole) the more Very obvious chance there is of problems with What is the outcome fracture in the healing. This is to do with the blood following a scaphoid middle (waist) supply to the scaphoid bone which fracture? of the scaphoid is not good in the proximal pole. -

What Is the Best Way to Evaluate an Acute Traumatic Knee Injury?
From the CLINICAL INQUIRIES Family Physicians Inquiries Network Matthew L. Silvis, MD, C. Randall Clinch, DO, MS, What is the best way and Janine S. Tillet, MSLS Wake Forest University, to evaluate an acute Winston-Salem, NC traumatic knee injury? Evidence-based answer Use the Ottawa Knee Rules. When there or ligamentous injury (SOR: C, based on is a possibility of fracture, they can guide studies of intermediate outcomes). the use of radiography in adults who Sonographic examination of a present with isolated knee pain. However, traumatized knee can accurately detect information on use of these rules in the internal knee derangement (SOR: C, pediatric population is limited (strength based on studies of intermediate of recommendation [SOR]: A, based on outcomes). Magnetic resonance imaging systematic review of high-quality studies (MRI) of the knee is the noninvasive and a validated clinical decision rule). standard for diagnosing internal knee Specific physical examination maneuvers derangement, and it is useful for both adult (such as the Lachman and McMurray tests) and pediatric patients (SOR: C, based on FAST TRACK may be helpful when assessing for meniscal studies of intermediate outcomes). Employ the Clinical commentary Ottawa Knee Rules Ottawa rules for ankles—yes, test, Drawer sign, and McMurray test to determine but they’re good for knees, too are useful in diagnosing the presence of whether plain The evidence presented here suggests internal ligamentous injuries without MRI, x-rays are needed a number of practical and useful and an ultrasound can help to detect knee to rule out fracture approaches for the evaluation of acute effusion when it is not clinically obvious. -

Comparison of Ottawa Ankle Rules and Bernese Ankle Rules in Acute Ankle and Midfoot Injuries
ORIGINAL ARTICLE Comparison of Ottawa Ankle Rules and Bernese Ankle Rules in Acute Ankle and Midfoot Injuries Ayak ve ayak bileği yaralanmalarında Ottawa ayak bileği kuralları ve Bernese ayak bileği kurallarının karşılaştırılması Türkiye Acil Tıp Dergisi - Turk J Emerg Med 2010;10(3):101-105 Ozkan KOSE,1 Servan GOKHAN,2 Ayhan OZHASENEKLER,2 Mustafa CELIKTAS,3 Seyhmus YIGIT,3 Serkan GURCAN4 1Antalya Training and Research Hospital, SUMMARY Department of Orthopedics and Traumatology, Antalya Objective: The purpose of this study was to compare the sensitivity and specificity of Ottawa Ankle Rules (OAR) 2Diyarbakır Training and Research and Bernese Ankle Rules (BAR) in acute ankle and midfoot injuries in the emergency department. Hospital, Department of Emergency Medicine, Diyarbakır Methods: 100 consecutive patients presented to our emergency department with acute ankle and/or midfoot 3Diyarbakır State Hospital, injuries following a blunt trauma were included. Patients were physically examined and evaluated regarding the Department of Orthopedics and BAR and OAR respectively by the same emergency medicine physician. All patients were referred for standard radi- Traumatology, Diyarbakır ography of the ankle or foot or both according to the presence of pain or tenderness in one or both of these zones. 4Diyarbakır Training and Research Hospital, Radiography results were interpreted by a consultant orthopedic surgeon who had not examined the patients. Department of Orthopedics and Sensitivity, specificity, positive and negative predictive values of each test were calculated. Traumatology, Diyarbakır Results: Radiographic examinations showed 19 fractures out of 100 investigated patients. Sensitivity and specificity of OAR were 100% and 77% respectively. Sensitivity and specificity of BAR were 94% and 95% respectively. -

Comparison of Diagnostic Accuracy of Bedside Ultrasonography and Radiography for Calcaneal Fractures in the Emergency Department
Open Access http://jept.ir Publish Free doi 10.34172/jept.2020.36 Journal of Emergency Practice and Trauma Original Article Volume 7, Issue 1, 2021, 2020, p. 17-21 Comparison of diagnostic accuracy of bedside ultrasonography and radiography for calcaneal fractures in the emergency department Majid Zamani ID , Maliheh Mazaheri ID , Farhad Heydari* ID , Babak Masoumi ID Department of Emergency Medicine, Faculty of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran Received: 1 June 2020 Abstract Accepted: 14 September 2020 Objective: Ultrasonography (US) is not the method of choice for the diagnosis of calcaneal Published online: 24 September fractures. The aim of this study was to compare the diagnostic accuracy of US with plain 2020 radiography in the diagnosis of calcaneus fractures following blunt ankle and foot trauma. *Corresponding author: Methods: In this cross-sectional study, 214 patients (over 18 years) presenting to the Farhad heydari; Emergency emergency department (ED) with suspicion of traumatic calcaneus fracture following acute Medicine Specialist; Department of Emergency Medicine, Faculty blunt trauma, were enrolled. Bedside ultrasonography was performed and interpreted by of Medicine, Isfahan University of emergency physicians. After that, plain radiography was performed. Furthermore, all the Medical Sciences, Isfahan, Iran patients were assessed by computed tomography (CT) scan as the gold standard. Alzahra Hospital, Sofeh Ave, Keshvari Results: Finally, 193 patients were enrolled with a mean age of 29.4 ± 15.7 years (85.5% Blvd., Isfahan, Iran. male). Fractures in the calcaneus were detected in 49 patients. The sensitivity and specificity Tel: +989131367643; Email: [email protected] of ultrasonography in the detection of calcaneal fractures were 83.6%, (confidence interval (CI), 69.7 –92.2) and 100% (95% CI, 96.7 –100), while the sensitivity and specificity of X-ray Competing interests: None. -

Talo-Calcaneal Distraction Ilizarov Frame: an Ergonomic Method to Manage Intra-Articular Fractures of Calcaneum
ORIGINAL ARTICLE ASIAN JOURNAL OF MEDICAL SCIENCES Talo-calcaneal distraction Ilizarov frame: an ergonomic method to manage intra-articular fractures of calcaneum Anoop Raj Singh1, Javed Ahmad 2, Vivek Kumar Shrivastava3, Pavneesh Kumar4 1Assistant Professor, Department of Orthopedics, SMMH Medical College, Saharanpur, Uttar Pradesh, India, 2,3Assistant Professor, Department of Orthopedics, Mahamaya Rajkiya Allopathic Medical College, Ambedkar Nagar, Uttar Pradesh, India, SMMH Medical College, Saharanpur, Uttar Pradesh, India, 4Assistant Professor, Department of Orthopedics, Government Doon Medical College Dehradun, India Submission: 07-03-2021 Revision: 27-05-2021 Publication: 01-07-2021 ABSTRACT Background: Principle of distraction and an indirect reduction was used to promote healing of Access this article online fractures and adequate regeneration of cartilage at the subtalar joint. Aims and Objectives: The Website: study was aimed to elaborate and develop role of Ilizarov as an alternative biological method to manage intraarticular fracture calcaneum with minimal chances of infection. http://nepjol.info/index.php/AJMS Materials and Methods: Twenty-one patients were studied and the mean age of patients DOI: 10.3126/ajms.v12i7.35459 was 40.7 years (span: 20 to 65 years). Sanders CT classification was used to divide into E-ISSN: 2091-0576 type II, 11 (52.38%); type III, 7 (33.33%) and type IV, 3 (14.28%). The average follow-up P-ISSN: 2467-9100 was 17.2 months (range: 6 to 24 months). AOFAS scale for ankle and hindfoot was used for assessment of patients- 7 (33.33%) excellent, 7 (33.33%) good, 3 (14.28%) fair, and 4 Copyright (c) 2021 Asian Journal of (19.04%) poor results. -

Ankle-Injuries-Guideline
RADIOGRAPHY OF THE ANKLE AND FOOT (OTTAWA ANKLE RULES) Clinical Practice Guideline | January 2007 This guideline has been adapted from the Ottawa Ankle Rules developed by Dr. Ian Stiell et al. Dr. Stiell received financial support from the Institute of Clinical and Evaluative Studies in Ontario. OBJECTIVE The Ottawa Ankle Rules will assist Alberta clinicians assess if radiography of the foot and ankle is required for adult patients presenting with blunt ankle trauma at health care facilities. TARGET POPULATION Adults, 18 years of age and older EXCLUSIONS Under 18 years of age, intoxicated, multiple painful injuries, pregnant, head injury, diminished sensation due to neurological deficit RECOMMENDATIONS An ankle x-ray series is required only if there is pain in the malleolar zone and any one of the following: o Bone tenderness along the distal 6 cm of the posterior edge of the fibula or tip of the lateral malleolus o Bone tenderness along the distal 6 cm of the posterior edge of the tibia or tip of the medial malleolus o Inability to bear weight for four steps immediately and in the emergency department A foot x-ray series is required only if there is pain in the midfoot zone and any one of the following: o Bone tenderness at the base of the 5th metatarsal o Bone tenderness at the navicular bone o Inability to bear weight for four steps both immediately and in the emergency department OTTAWA ANKLE RULES POSTER PDF http://www.ohri.ca/emerg/cdr/docs/cdr_ankle_poster.pdf (link available as of March 2014) These recommendations are systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances. -

Acute Ankle Trauma in Adults
For Information Only This document has been archived, much of the original content remains relevant; however, practice in this area develops continually, therefore the content of this document must be used for information only and is only valid as per the original approval date. Head Office: Level 9, 51 Druitt Street, Sydney NSW 2000, Australia Ph: +61 2 9268 9777 Email: [email protected] New Zealand Office: Floor 6, 142 Lambton Quay, Wellington 6011, New Zealand Ph: +64 4 472 6470 Email: [email protected] Web: www.ranzcr.com ABN 37 000 029 863 2015 Educational Modules for Appropriate Imaging Referrals ACUTE ANKLE TRAUMA IN ADULTS This document is part of a set of ten education modules which are aimed at improving the appropriateness of referrals for medical imaging by educating health professionals about the place of imaging in patient care. PUBLICATION INFORMATION: ©Royal Australian and New Zealand College of Radiologists 2015 More information is available on The Royal Australian and New Zealand College of Radiologists website: URL: http://www.ranzcr.edu.au/quality-a-safety/program/key-projects/education-modules-for- appropriate-imaging-referrals For educational purposes only. The preferred citation for this document is: Goergen S, Troupis J, Yalcin N, Baquie P and Shuttleworth G. Acute Ankle Trauma in Adults. Education Modules for Appropriate Imaging Referrals. Royal Australian and New Zealand College of Radiologists, 2015. ACKNOWLEDGEMENTS: The Educational Modules for Appropriate Imaging Referrals project is fully funded by the -

Calcaneal Fracture and Rehabilitation
1 Calcaneal Fracture and Rehabilitation Surgical Indications and Considerations Anatomic Considerations: The calcaneus articulates with the talus superiorly at the subtalar joint. The three articulating surfaces of the subtalar joint are the: anterior, middle, and posterior facets, with the posterior facet representing the major weight-bearing surface. The subtalar joint is responsible for the majority of foot inversion/eversion (or pronation/supination). The interosseous ligament and medial, lateral, and posterior talocalcaneal ligaments provide additional support for the joint. The tibial artery, nerve, posterior tibial tendon, and flexor hallucis longus tendon are located medially to the calcaneus and are at risk for impingement with a calcaneal fracture, as are the peroneal tendons located on the lateral aspect of the calcaneus. The calcaneus serves three major functions: 1) acts as a foundation and support for the body’s weight, 2) supports the lateral column of the foot and acts as the main articulation for inversion/eversion, and 3) acts as a lever arm for the gastrocnemius muscle complex. Pathogenesis: Fractures of the calcaneal body, anterior process, sustentaculum tali, and superior tuberosity are known as extra-articular fractures and usually occur as a result of blunt force or sudden twisting. Fractures involving any of the three subtalar articulating surfaces are known as intra-articular fractures and are common results of: a fall from a height usually 6 feet or more, a motor vehicle accident (MVA), or an impact on a hard surface while running or jumping. Intra-articular fractures are commonly produced by axial loading; a combination of shearing and compression forces produce both the primary and secondary fracture lines.