Dr. Pelto's Welcome Packet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

Pediatric MSK Protocols
UT Southwestern Department of Radiology Ankle and Foot Protocols - Last Update 5-18-2015 Protocol Indications Notes Axial Coronal Sagittal Ankle / Midfoot - Routine Ankle Pain Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD SPAIR T1 FSE Injury, Internal Derangement Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR STIR Talar OCD, Coalition Protocol Indications Notes Axial Coronal Sagittal Ankle / Midfoot - Arthritis Arthritis Axial = In Relation to Leg "Footprint" (Long Axis to Foot) PD SPAIR PD SPAIR T1 FSE Coronal = In Relation to Leg (Short Axis Foot) STIR T1 SPIR POST T1 SPIR POST Protocol Indications Notes Axial Coronal Sagittal Foot - Routine Pain, AVN Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD FSE T1 FSE Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR PD SPAIR STIR Protocol Indications Notes Axial Coronal Sagittal Foot - Arthritis Arthritis Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD SPAIR STIR Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR T1 SPIR POST 3D WATS T1 SPIR POST Protocol Indications Notes Axial Coronal Sagittal Great Toe / MTP Joints Turf Toe Smallest Coil Possible (Microcoil if Available) PD FSE T1 FSE PD FSE Sesamoiditis FoV = Mid Metatarsal Through Distal Phalanges PD SPAIR PD SPAIR PD SPAIR Slice thickness = 2-3 mm, 10% gap Axial = In relation to the great toe (short axis foot) Coronal = In relation to the great toe (long axis foot / footprint) Appropriate Coronal Plane for Both Ankle and Foot Imaging UT Southwestern Department -

Desarrollo De La Podología En España
Desarrollo de la podología en España Virginia Novel Martí ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tdx.cat) i a través del Dipòsit Digital de la UB (diposit.ub.edu) ha estat autoritzada pels titulars dels drets de propietat intelꞏlectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX ni al Dipòsit Digital de la UB. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX o al Dipòsit Digital de la UB (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tdx.cat) y a través del Repositorio Digital de la UB (diposit.ub.edu) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR o al Repositorio Digital de la UB. -

First Metatarsophalangeal Joint Replacement with Total Arthroplasty in the Surgical Treatment of the Hallux Rigidus R
Acta Biomed 2014; Vol. 85, Supplement 2: 113-117 © Mattioli 1885 Original article First metatarsophalangeal joint replacement with total arthroplasty in the surgical treatment of the hallux rigidus R. Valentini, G. De Fabrizio, G. Piovan Clinica Ortopedica e Traumatologica, Università degli Studi di Trieste, Azienda Ospedaliero-Universitaria “Ospedali Riuniti” di Trieste Abstract. The hallux rigidus, especially in advanced stage, has always been a challenge as regards the surgical treatment. Over the years there have been various surgical techniques proposed with the aim of relieving pain, correcting deformity and maintain a certain degree of movement. For some years we have addressed the prob- lem with the replacement metatarsophalangeal joint arthroplasty with Reflexion system. As far as our experi- ence we have operated and monitored 25 patients (18 females and 7 males) of mean age 58.1 years, operated with this technique from June 2008 to June 2011. It reached an average ROM of 72° (extension and flexion 45° and 27°) with a good functional recovery in 8 patients, and this articulation was good (50° - 40°) in 12 patients and moderate in 5 with a articular range from 40°- 30°. The clinical results, according to our experience, appear to be favorable, as even patient satisfaction is complete. (www.actabiomedica.it) Key words: hallux rigidus, metatarsophalangeal, arthroprosthesis Introduction The pathology of stiff big toe has ranked about Regnauld classification (5) in three stages, so that the Degenerative disease of the first metatarsal- I stage is characterized by wear of the joint with mini- phalangeal articulation, the so-called “Hallux rigi- mal osteophytes reaction, the II stage is reached when dus”, especially in advanced phase, has always been the joint line is further reduced, the articular surfaces a sort of challenge as a surgical treatment. -

Overuse Injuries in Elite Athletes
ATHLETES: OVERUSE MRI of Overuse INJURIES VERY COMMON Injury in the Elite Athlete • Muscle William B. Morrison, M.D. Associate Professor of • Joints Radiology Thomas Jefferson • Tendon University Hospital Philadelphia, PA USA • Ligament • Bone [email protected] How is this Relevant to My Practice? • High performance athletes get similar injuries as ‘regular’ people… but: – More of them, & at a younger age MUSCLE / SOFT TISSUE – More commonly imaged – Secondary gain involved INJURY • All the cases here are high performance athletes – but most injuries are conventional • Exceptions – Some weird sport-specific patterns of stress and other injuries – Acute injuries as opposed to overuse •Overuse –DOMS Muscle Injury Delayed Onset Muscle • Acute injury Soreness (DOMS) – Tendon – Myotendinous junction • All athletes are susceptible if they – Muscle belly change training regimen • Athletes tend to work out intensely – leads to muscle injury • Rarely imaged (“no pain no gain”) – Weightlifting / aerobic exercise – 24hr later – soreness – Can be severe, even look like a tear 1 Acute Muscle Injury • Direct → muscle belly, esp quadriceps T2 – esp rugby, football • Indirect → myotendinous junction – eccentric contraction – sudden acceleration / DOMS: Lateral gastrocnemius deceleration Finding can be subtle, even with T2 and fat sat Professional football player Acute Injury – T1 Quadriceps hematoma Muscle belly injury Myotendinous Unit Hit with helmet • Myotendinous Junction – ‘weak link’ of normal myotendinous complex T2 – Common place for injury – Most common mechanism: eccentric contraction (muscle lengthens and contracts at the same High time) T1 = blood Gastrocnemius tear: Grade 1 Muscle Strain “V” sign • Ill-defined edema T2 T1 STIR Weishaupt D, JCAT 2001; 25:677 2 Gd Gd can help identify Grade 2 Muscle Strain subtle muscle injury AKA “Partial Tear” STIR Professional baseball player Grade 1 strain Sartorius m. -

Bilateral Hallux Varus Deformity Correction with a Suture Button Construct
A Case Report & Literature Review Bilateral Hallux Varus Deformity Correction With a Suture Button Construct Andrew R. Hsu, MD, Christopher E. Gross, MD, and Johnny L. Lin, MD common surgery for hallux varus correction is transfer of the Abstract extensor hallucis longus partially or completely under the deep Hallux varus deformity typically results from transverse intermetatarsal ligament to the lateral aspect base soft-tissue overcorrection at the metatarsopha- of the proximal phalanx.10,11 However, complications include langeal joint during surgery for hallux valgus. weakened extension and the inability to fix an overcorrected There are several soft-tissue procedures avail- intermetatarsal angle. Alternatively, the abductor hallucis can able for flexible hallux varus deformity includ- be tenotomized or transferred to the base of the proximal ing transfer of the extensor hallucis longus or phalanx to reconstruct the lateral capsular ligaments.8,9 The abductor hallucis. To our knowledge, there have lateral capsular ligaments can be reinforced or reconstructed not been any previous reports in the literature of with fascia lata or soft-tissue anchors, but these procedures rely bilateral hallux varus deformities in the setting of on adequate healthy tissue remaining around the MTP joint.9,12 potential pregnancy-related ligamentous laxity The Mini TightRope (Arthrex Inc, Naples, Florida) is an im- combined with iatrogenic injury. We present the planted suture endobutton device that has previously been used 13 case of an isolated bilateral hallux varus defor- for hallux valgus repair. The suture button technique has also mity occurring after pregnancy and prior bunion been used to recreate ligaments and tendons in syndesmotic 14,15 14 surgery. -
Information to Users
INFORMATION TO USERS This manuscript has been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter free, i ^ e others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely afreet reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand comer and continuing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. Higher quality 6” x 9” black and white photographic prints are available for any photographs or illustrations appearing in this copy for an additional charge. Contact UMI directly to order. UMI A Bell & Howell Information Compaiy 300 North Zeeb Road, Ann Arbor MI 48106-1346 USA 313/761-4700 800/521-0600 PHYSIOLOGIC RESPONSES TO INFLAMMATION IN ISOLATED EQUINE JOINTS DISSERTATION Presented in Partial Fulfilment of the Requirements for the Degree of Doctor of Philosophy in the Graduate School of The Ohio State University B y Joanne Hardy, D.V.M., M.S. -
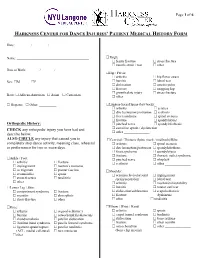
Harkness Center for Dance Injuries' Patient Medical History Form
Page 1 of 6 HARKNESS CENTER FOR DANCE INJURIES’ PATIENT MEDICAL HISTORY FORM Date: ________ / ________ / ________ Name: __________________________________________ Thigh: femur fracture stress fracture muscle strain / tear other_______________ Date of Birth: _______ / _______ / _______ Hip / Pelvis: arthritis hip flexor strain Sex: M F bursitis labral tear dislocation osteitis pubis fracture snapping hip growth plate injury stress fracture Race: African-American Asian Caucasian other _______________ Hispanic Other: __________ Lumbar-Sacral Spine (low back): arthritis sciatica disc herniation/protrusion scoliosis facet syndrome spinal stenosis fracture spondylolysis Orthopedic History: pinched nerve spondylolisthesis CHECK any orthopedic injury you have had and sacroiliac sprain / dysfunction other _______________ describe below. ALSO CIRCLE any injury that caused you to Cervical / Thoracic Spine (neck / mid back)/Ribs: completely stop dance activity, meaning class, rehearsal arthritis spinal stenosis or performance for two or more days. disc herniation/protrusion spondylolisthesis facet syndrome spondylolysis fracture thoracic outlet syndrome Ankle / Foot: pinched nerve whiplash arthritis fracture scoliosis other _______________ impingement morton’s neuroma os trigonum plantar fasciitis Shoulder: sesamoiditis sprain acromioclavicular joint impingement stress fracture tendinitis sprain/separation labral tear other________________ arthritis mechanical instability Lower Leg / Shin: -

Biomechanics of Nerve and Muscle
The Biomechanics of the Human Lower Extremity DR.AYESH BASHARAT BSPT, PP.DPT. M.Phil (Gold-medalist) Hip joint One of the largest and most stable joint: The hip joint Rigid ball-and-socket configuration (Intrinsic stability) The femoral head Femoral head : convex component Two-third of a sphere, Cover with cartilage Rydell (1965) suggested : most load----- superior quadrant Femur Long, strong & most weight bearing bone. But most weakest structure of it is its neck. During walk in single leg support move medially to support C0G. This results in the leg being shortened on non-weight bearing side. Fracture of femur-neck common as bone tissue in the neck of the femur is softer than normal. Acetabulum Concave component of ball and socket joint Facing obliquely forward, outward and downward Covered with articular cartilage Provide static stability Labrum: a flat rim of fibro cartilage Acetabulum Also contain Transverse acetabular ligament provide stability Ligaments and Bursae •Iliofemoral ligament: Y shaped extremely strong= anterior stability •Pubofemoral ligament: anterior stability • Ischiofemoral ligament: posterior stability • Ligamentum teressupplies a direct attachment from rim of acetabulum to head of femur Iliopsoas burs b/w illiopsoas & capsule Trochantric bursitis The femoral neck Frontal plane (the neck-to-shaft angle/ angle of inclination), Transverse plane (the angle of anteversion) Neck-to- shaft angle : 125º, vary from 110º to 135-140º Effect : lever arms Angle of anteversion :12º Effect : during gait >12º :internal rotation <12º :external rotation aa The anteverted femur effect the biomechanics of not only hip joint but also disturbed the knee and ankle joint normal mechanics during different physical activities a Structure of the Hip Sacrum Ilium Acetabulum Femoral head Pubis Ischium Femur The pelvic girdle includes the two ilia and the sacrum,. -

Patient Medical History Form
Date of Visit: ________ / ________ / ________ ID # (R=Research) +MR# Patient Medical History Form Name: __________________________________________ Knee: arthritis osgood-schlatter’s Date of Birth: _______ / _______ / _______ Sex: M F bursitis osteochondritis dissecans Social Security ______-_____-________ chondromalacia patellar dislocation iliotibial band syndrome patella femoral syndrome Race: African-American Asian Caucasian ligament sprain/rupture patellar tendinitis Hispanic Other: __________ (ACL, medial collateral) torn meniscus other________________ Address:___________________________________________ ______________________________________________ Thigh: femur fracture stress fracture City: _________________ State: _______ ZIP: ________ muscle strain / tear other_______________ Primary Phone: _______ - ________ - __________ Hip / Pelvis: Email: ___________________________________________ arthritis hip flexor strain bursitis labral tear Emergency Contact Information: dislocation osteitis pubis Name: ___________________________________________ fracture snapping hip growth plate injury stress fracture Relation: ______________ Phone:_____________________ other _______________ Health Insurance Information: Lumbar-Sacral Spine (low back): Name of Insurance Co: _____________________________ arthritis sciatica Name of Policy Holder: _____________________________ disc herniation/protrusion scoliosis facet syndrome spinal stenosis Policy #: _________________ Group#: ________________ fracture spondylolsysis -

Understanding the First
CME / ORTHOTICS & BIOMECHANICS Goals and Objectives After reading this CME the practitioner will be able to: 1) Understand normal and abnormal function of the first ray with special emphasis on its integral role in medial longitudinal arch function and hypermobility. Understanding 2) Acquire knowledge of the various etiologic factors that result in first ray hypermobility. the First Ray 109 3) Appreciate its normal and abnormal motion along Here’s a review of its normal with its attendant bio and and abnormal function, identification, pathomechanics. and clinical significance. 4) Become familiar with vari- ous methods to subjectively and BY JOSEPH C D’AMICO, DPM objectively identify its presence. Welcome to Podiatry Management’s CME Instructional program. Our journal has been approved as a sponsor of Con- tinuing Medical Education by the Council on Podiatric Medical Education. You may enroll: 1) on a per issue basis (at $26.00 per topic) or 2) per year, for the special rate of $210 (you save $50). You may submit the answer sheet, along with the other information requested, via mail, fax, or phone. You can also take this and other exams on the Internet at www.podiatrym.com/cme. If you correctly answer seventy (70%) of the questions correctly, you will receive a certificate attesting to your earned credits. You will also receive a record of any incorrectly answered questions. If you score less than 70%, you can retake the test at no additional cost. A list of states currently honoring CPME approved credits is listed on pg. 144. Other than those entities currently accepting CPME-approved credit, Podiatry Management cannot guarantee that these CME credits will be acceptable by any state licensing agency, hospital, managed care organization or other entity. -

Foot Orthotics and Other Podiatric Appliances
MEDICAL POLICY POLICY TITLE FOOT ORTHOTICS AND OTHER PODIATRIC APPLIANCES POLICY NUMBER MP 6.028 Original Issue Date (Created): 7/1/2002 Most Recent Review Date (Revised): 3/19/2021 Effective Date: 8/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY APPENDIX I. POLICY Orthopedic shoes and other supportive devices of the feet are considered medically necessary ONLY when they are an integral part of a leg brace. These shoes and devices are described as Oxford shoes or other shoes, e.g. high top, depth inlay or custom for non- diabetics, heel replacements, sole replacements, and shoe transfers. Inserts and other shoe modifications are covered if they are on a shoe that is an integral part of a covered brace and if they are medically necessary for the proper functioning of the brace. Foot orthotics other than those that are an integral part of a brace may be considered medically necessary only when they are a benefit of a member’s contract, to meet specific needs of the patient, and prescribed by a physician for the below criteria: For Adults and Children [Any ONE Condition]: Chronic plantar fasciitis Calcaneal bursitis (chronic only) Calcaneal spurs (heel spurs) Chronic ankle instability Inflammatory conditions (i.e., sesamoiditis; submetatarsal bursitis; synovitis; tenosynovitis; synovial cyst; osteomyelitis; rheumatoid disease; and osteoarthritis) Medial osteoarthritis of the knee (lateral wedge insoles) Musculoskeletal/arthropathic