Pediatric MSK Protocols
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Elbow Arthroscopy for Osteochondral Lesions in Athletes
SPORTS SURGERY ELBOW ARTHROSCOPY FOR OSTEOCHONDRAL LESIONS IN ATHLETES – Written by Luigi Pederzini et al, Italy Several sports specific injuries of the elbow OSTEOCHONDRAL DEFECT have been well-described. For example, Definition and symptoms the prevalence of medial elbow instability Osteochondral defect is a detachment is high in throwing athletes such as of bone and cartilage in a joint that can Osteochondral baseball players. Similarly, javelin throwers, cause pain. The clinical presentation defect is a volleyball players and tennis players are is characterised by an acute or chronic frequently complaining about elbow pain. onset of symptoms. The majority of detachment of This can be the result of intensive training patients with osteochondral defects of or chronic overuse which results in an the elbow complain of pain. In some bone and cartilage acute or chronic injury. Some of these patients the defect is associated with injuries can be osteochondral lesions such a loose body, and the patient presents in a joint that as osteochondral defects, osteochondrosis clinically with pain, giving way, swelling, can cause pain... of the capitulum humeri or osteochondritis catching, clicking, crepitus and elbow dissecans (OCD). stiffness aggravated by joint movements. characterised Standard X-rays are the initial studies of choice, but sometimes are negative. by an acute or Magnetic resonance imaging (MRI) and 3D computed tomography (CT) scan can chronic onset of be extremely useful in establishing an symptoms. accurate diagnosis and to add in pre- operative planning. 210 OSTEOCHONDROSIS OF CAPITULUM HUMERI (PANNER’S DISEASE) Definition and symptoms Panner’s disease, an ostechondrosis of the capitellum, is a rare disorder that usually affects the dominant elbow in individuals younger than 10 years old. -

SAS Journal of Surgery (SASJS) Panner's Disease: About a Case
SAS Journal of Surgery (SASJS) ISSN 2454-5104 Abbreviated Key Title: SAS J. Surg. ©Scholars Academic and Scientific Publishers (SAS Publishers) A Unit of Scholars Academic and Scientific Society, India Panner's Disease: About A Case Mohamed Ben-Aissi1, Redouane Hani1, Mohammed Kadiri1, Mouad Beqqali-Hassani1, Paolo Palmari2, Moncef Boufettal1, Mohamed Kharmaz1, Moulay Omar Lamrani1, Ahmed El Bardouni1, Mustapha Mahfoud1, Mohamed Saleh Berrada1 1Orthopedic surgery and traumatology department, Ibn Sina Hospital, Rabat, Morocco 2Orthopedic surgery and traumatology departemnt, Robert Ballanger Hospital, Paris, France Abstract: Panner's disease, or osteochondrosis of the lateral condylar nucleus, is an Case Report avascular necrosis leading to subchondral bone loss, it was first described in 1927. We report a case of Panner's disease, which has been evolving since 1 month, in a child of 8 *Corresponding author years sportsman practicing karate. The evolution was favorable with restitution ad Mohamed Ben-Aissi integrum in 8 months after a short anti-inflammatory treatment and a sports rest of 3 months, without any immobilization of the neither elbow nor surgical intervention. Article History Keywords: Osteochondrosis, Panner’s disease, Treatment. Received: 03.10.2018 Accepted: 06.10.2018 INTRODUCTION Published: 30.10.2018 Panner's disease, or osteochondrosis of the lateral condylar nucleus, is an avascular necrosis leading to a loss of subchondral bone fissuring the radio-humeral DOI: articular surfaces, occurring in the hyperspottive child, in connection with an overuse of 10.21276/sasjs.2018.4.10.7 the elbow [1, 2]. It was first described in 1927 by Dane Panner, a Danish orthopedic surgeon [2, 3]. -

Desarrollo De La Podología En España
Desarrollo de la podología en España Virginia Novel Martí ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tdx.cat) i a través del Dipòsit Digital de la UB (diposit.ub.edu) ha estat autoritzada pels titulars dels drets de propietat intelꞏlectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX ni al Dipòsit Digital de la UB. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX o al Dipòsit Digital de la UB (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tdx.cat) y a través del Repositorio Digital de la UB (diposit.ub.edu) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR o al Repositorio Digital de la UB. -

Overuse Injuries in Elite Athletes
ATHLETES: OVERUSE MRI of Overuse INJURIES VERY COMMON Injury in the Elite Athlete • Muscle William B. Morrison, M.D. Associate Professor of • Joints Radiology Thomas Jefferson • Tendon University Hospital Philadelphia, PA USA • Ligament • Bone [email protected] How is this Relevant to My Practice? • High performance athletes get similar injuries as ‘regular’ people… but: – More of them, & at a younger age MUSCLE / SOFT TISSUE – More commonly imaged – Secondary gain involved INJURY • All the cases here are high performance athletes – but most injuries are conventional • Exceptions – Some weird sport-specific patterns of stress and other injuries – Acute injuries as opposed to overuse •Overuse –DOMS Muscle Injury Delayed Onset Muscle • Acute injury Soreness (DOMS) – Tendon – Myotendinous junction • All athletes are susceptible if they – Muscle belly change training regimen • Athletes tend to work out intensely – leads to muscle injury • Rarely imaged (“no pain no gain”) – Weightlifting / aerobic exercise – 24hr later – soreness – Can be severe, even look like a tear 1 Acute Muscle Injury • Direct → muscle belly, esp quadriceps T2 – esp rugby, football • Indirect → myotendinous junction – eccentric contraction – sudden acceleration / DOMS: Lateral gastrocnemius deceleration Finding can be subtle, even with T2 and fat sat Professional football player Acute Injury – T1 Quadriceps hematoma Muscle belly injury Myotendinous Unit Hit with helmet • Myotendinous Junction – ‘weak link’ of normal myotendinous complex T2 – Common place for injury – Most common mechanism: eccentric contraction (muscle lengthens and contracts at the same High time) T1 = blood Gastrocnemius tear: Grade 1 Muscle Strain “V” sign • Ill-defined edema T2 T1 STIR Weishaupt D, JCAT 2001; 25:677 2 Gd Gd can help identify Grade 2 Muscle Strain subtle muscle injury AKA “Partial Tear” STIR Professional baseball player Grade 1 strain Sartorius m. -
Information to Users
INFORMATION TO USERS This manuscript has been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter free, i ^ e others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely afreet reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand comer and continuing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. Higher quality 6” x 9” black and white photographic prints are available for any photographs or illustrations appearing in this copy for an additional charge. Contact UMI directly to order. UMI A Bell & Howell Information Compaiy 300 North Zeeb Road, Ann Arbor MI 48106-1346 USA 313/761-4700 800/521-0600 PHYSIOLOGIC RESPONSES TO INFLAMMATION IN ISOLATED EQUINE JOINTS DISSERTATION Presented in Partial Fulfilment of the Requirements for the Degree of Doctor of Philosophy in the Graduate School of The Ohio State University B y Joanne Hardy, D.V.M., M.S. -
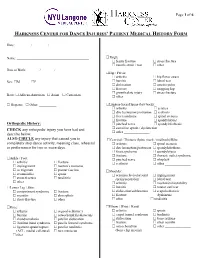
Harkness Center for Dance Injuries' Patient Medical History Form
Page 1 of 6 HARKNESS CENTER FOR DANCE INJURIES’ PATIENT MEDICAL HISTORY FORM Date: ________ / ________ / ________ Name: __________________________________________ Thigh: femur fracture stress fracture muscle strain / tear other_______________ Date of Birth: _______ / _______ / _______ Hip / Pelvis: arthritis hip flexor strain Sex: M F bursitis labral tear dislocation osteitis pubis fracture snapping hip growth plate injury stress fracture Race: African-American Asian Caucasian other _______________ Hispanic Other: __________ Lumbar-Sacral Spine (low back): arthritis sciatica disc herniation/protrusion scoliosis facet syndrome spinal stenosis fracture spondylolysis Orthopedic History: pinched nerve spondylolisthesis CHECK any orthopedic injury you have had and sacroiliac sprain / dysfunction other _______________ describe below. ALSO CIRCLE any injury that caused you to Cervical / Thoracic Spine (neck / mid back)/Ribs: completely stop dance activity, meaning class, rehearsal arthritis spinal stenosis or performance for two or more days. disc herniation/protrusion spondylolisthesis facet syndrome spondylolysis fracture thoracic outlet syndrome Ankle / Foot: pinched nerve whiplash arthritis fracture scoliosis other _______________ impingement morton’s neuroma os trigonum plantar fasciitis Shoulder: sesamoiditis sprain acromioclavicular joint impingement stress fracture tendinitis sprain/separation labral tear other________________ arthritis mechanical instability Lower Leg / Shin: -

Patient Medical History Form
Date of Visit: ________ / ________ / ________ ID # (R=Research) +MR# Patient Medical History Form Name: __________________________________________ Knee: arthritis osgood-schlatter’s Date of Birth: _______ / _______ / _______ Sex: M F bursitis osteochondritis dissecans Social Security ______-_____-________ chondromalacia patellar dislocation iliotibial band syndrome patella femoral syndrome Race: African-American Asian Caucasian ligament sprain/rupture patellar tendinitis Hispanic Other: __________ (ACL, medial collateral) torn meniscus other________________ Address:___________________________________________ ______________________________________________ Thigh: femur fracture stress fracture City: _________________ State: _______ ZIP: ________ muscle strain / tear other_______________ Primary Phone: _______ - ________ - __________ Hip / Pelvis: Email: ___________________________________________ arthritis hip flexor strain bursitis labral tear Emergency Contact Information: dislocation osteitis pubis Name: ___________________________________________ fracture snapping hip growth plate injury stress fracture Relation: ______________ Phone:_____________________ other _______________ Health Insurance Information: Lumbar-Sacral Spine (low back): Name of Insurance Co: _____________________________ arthritis sciatica Name of Policy Holder: _____________________________ disc herniation/protrusion scoliosis facet syndrome spinal stenosis Policy #: _________________ Group#: ________________ fracture spondylolsysis -
SPR 2015 the Good, the Bad and the Ugly
SPR 2015 The Good, the Bad and the Ugly Diego Jaramillo, M.D., M.P.H. Department of Radiology Children’s Hospital of Philadelphia University of Pennsylvania Pearlman School of Medicine Variants, small abnormalities, and disease are closelyo related Little holes in the humeral head? Developmental proximal humeral cyst Posterior, adjacent to union between greater and lesser tuberosity Cyst related to rotator cuff injury (courtesy of Tal Laor, MD) • Anterior, adjacent to footprint (insertion) Intertuberosity Cysts vs. Rotator Cuff Cyts Intertuberosity Rotator Cuff Cysts Cysts Age (yr) <15 >10 Location Posterior Anterior Rotator Cuff Not usually Yes Disease Little hole in the capitellum? Osteochondral injury with loose body Acute Osteochondral Injuries • Anterior capitellum • Fragment usually detaches at o-c junction • Only acute changes in the bone Persistent pain after a fall 13-year-old competitive tennis player Osteochondritis Dissecans 6 month follow up Osteochondritis Dissecans • Anterior to inferior capitellum • Bone marrow edema • Cystic changes • Findings similar to those of OCD in the knee 8-year-old with elbow pain Panner’s Disease • Osteonecrosis of the capitellum • First decade • Repetitive trauma 17 “Pseudo Panner”: Irregular ossification variant Regarding elbow OCD and Panner’s disease, which of these statements is true: 1. Both affect the same age group 2. The trochlea is the structure most frequently affected by Panner’s disease 3. The capitellum is the structure most frequently affected by OCD 4. The articular cartilage is disrupted in Panner’s disease Regarding elbow OCD and Panner’s disease, which of these statements is true: 1. Both affect the same age group 2. -

Rotator Cuff Tendinitis Shoulder Joint Replacement Mallet Finger Low
We would like to thank you for choosing Campbell Clinic to care for you or your family member during this time. We believe that one of the best ways to ensure quality care and minimize reoccurrences is through educating our patients on their injuries or diseases. Based on the information obtained from today's visit and the course of treatment your physician has discussed with you, the following educational materials are recommended for additional information: Shoulder, Arm, & Elbow Hand & Wrist Spine & Neck Fractures Tears & Injuries Fractures Diseases & Syndromes Fractures & Other Injuries Diseases & Syndromes Adult Forearm Biceps Tear Distal Radius Carpal Tunnel Syndrome Cervical Fracture Chordoma Children Forearm Rotator Cuff Tear Finger Compartment Syndrome Thoracic & Lumbar Spine Lumbar Spine Stenosis Clavicle Shoulder Joint Tear Hand Arthritis of Hand Osteoporosis & Spinal Fx Congenital Scoliosis Distal Humerus Burners & Stingers Scaphoid Fx of Wrist Dupuytren's Comtracture Spondylolysis Congenital Torticollis Shoulder Blade Elbow Dislocation Thumb Arthritis of Wrist Spondylolisthesis Kyphosis of the Spine Adult Elbow Erb's Palsy Sprains, Strains & Other Injuries Kienböck's Disease Lumbar Disk Herniation Scoliosis Children Elbow Shoulder Dislocation Sprained Thumb Ganglion Cyst of the Wrist Neck Sprain Scoliosis in Children Diseases & Syndromes Surgical Treatments Wrist Sprains Arthritis of Thumb Herniated Disk Pack Pain in Children Compartment Syndrome Total Shoulder Replacement Fingertip Injuries Boutonnière Deformity Treatment -

Sports Injuries in Children Continued
Me d i c i n eT o d a y PEER REVIEWED ARTICLE POINTS: 2 CPD/1 PDP Sports injuries in childre n The number of children with sports injuries seen in sports medicine practices is increasing. The usual outcome is full recovery, but the consequence of a missed diagnosis of a more serious condition may be significant for the child. The important issue of encouraging children to be injuries seen in sports medicine practices appears more active in an effort to improve their overall to be actually increasing.1 , 2 health is a complex public health problem.1 , 2 Fortunately, many of the sports injuries that Childhood sports participation in Australia has occur in children are self-limited and full recovery unfortunately declined over the past few decades. is the usual outcome. However, more serious con- Some 86% of children aged 5 to 14 years were ditions may occasionally occur and the conse- active in sport in 1985, but by 2003, the level of quence of a missed diagnosis, especially during the participation had fallen to 54% for girls and 69% rapid pubertal growth phase, may be significant for boys.1 During this time period, the number of for the child. overweight and obese children has been increas- Pain in a child should not be dismissed as ‘grow- TOM CROSS ing. At the other end of the spectrum, more active ing pains’. If an informed systematic approach FACSP, MBBS, DCH children are training more intensively and for is followed, the clinical assessment of a child will longer periods of time in one or several sports. -

9 10 Ii 12 13 14 15 AGE(YEARS) About 80% of the Patients Came from the City of Oulu Or from the Close Neighbourhood
Br J Sports Med: first published as 10.1136/bjsm.12.1.4 on 1 March 1978. Downloaded from Brit. J. Sports Med. - Vol. 12, No. 1, March 1978, pp. 4-10 EXERTION INJURIES IN ADOLESCENT ATHLETES S. ORAVA, M.D. and J. PURANEN, M.D. Sports Clinic of Deaconess Institute, Oulu, and Dept. of Surgery, University Central Hospital, Oulu, Finland ABSTRACT A series of 147 cases of exertion injuries in < 15 years old athletes is presented. All injuries occurred during training or athletic performances without trauma and caused symptoms that prevented athletic exercises. There were 67 girls (46%) and 80 boys (54%) in the material. About 90% of them had been training for more than one year before the onset of the symptoms; 65% were interested in track and field athletics, 13% in ball games, 11% in skiing, 4% in swimming, and 3% in orienteering. The rest were interested in other sports. About 33% of the injuries were growth disturbances or osteochondroses seen also in other children. About 15% were anomalies, deformities or earlier osteochondritic changes, which caused first symptoms during the physical exercise; 50% were typical overuse injuries that may bother adult athletes, too; 43% of the injuries were localized in ankle, foot and heel, 31% in knee, 8% in back and trunk, 7% in pelvic and hip region, and the rest in other parts of the body. The injuries were generally slight, no permanent disability was noticed. Rest and conservative therapy cured most cases; operative treatment was used in only eight cases. Adolescent athletes' non-traumatic exertion injuries often differ from the usual overuse syndromes seen in adult athletes (Quinby, Truman et al 1964, Adams 1965, Torg, Pollack et al 1972, Cahill 1973, Schwerdtner & Schobert 1973, Shaffer 1973, Williams & Sperryn 1976). -

Childhood and Adolescent Sports-Related Overuse Injuries KYLE J
Childhood and Adolescent Sports-Related Overuse Injuries KYLE J. CASSAS, M.D., and AMELIA CASSETTARI-WAYHS, M.D., Methodist Health System, Dallas, Texas Youth sports participation carries an inherent risk of injury, includ- ing overuse injuries. Little leaguer’s shoulder, a stress fracture of the proximal humerus that presents as lateral shoulder pain, usually is self- limited. Little leaguer’s elbow is a medial stress injury; treatment con- sists of complete rest from throwing for four to six weeks followed by rehabilitation and a gradual throwing program. Spondylolysis is a stress fracture of the pars interarticularis. Diagnostic modalities include plain film radiography, bone scan, computed tomography, single photon emission computed tomography, and magnetic resonance imaging. Treatment usually is conservative. Spondylolisthesis is the forward or anterior displacement of one vertebral body over another and may be related to a history of spondylolysis. Diagnosis is made with plain film radiography and graded according to the amount of displacement. Osgood-Schlatter disease presents as anterior knee pain localized to the tibial tubercle. Diagnosis is made clinically, and most patients respond to conservative measures. Calcaneal apophysitis (or Sever’s disease) is a common cause of heel pain in young athletes, presenting as pain in the posterior aspect of the calcaneus. (Am Fam Physician 2006;73:1014-22. Copyright © 2006 American Academy of Family Physicians.) SCOTT BY ILLUSTRATION BODELL S Patient information: ach year in the United States, develop in young athletes when this growth A handout on Osgood- approximately 30 million children center is unable to meet the demands placed Schlatter disease is available online at http:// and teenagers participate in orga- on it during activity.