Patient Medical History Form
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pediatric MSK Protocols
UT Southwestern Department of Radiology Ankle and Foot Protocols - Last Update 5-18-2015 Protocol Indications Notes Axial Coronal Sagittal Ankle / Midfoot - Routine Ankle Pain Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD SPAIR T1 FSE Injury, Internal Derangement Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR STIR Talar OCD, Coalition Protocol Indications Notes Axial Coronal Sagittal Ankle / Midfoot - Arthritis Arthritis Axial = In Relation to Leg "Footprint" (Long Axis to Foot) PD SPAIR PD SPAIR T1 FSE Coronal = In Relation to Leg (Short Axis Foot) STIR T1 SPIR POST T1 SPIR POST Protocol Indications Notes Axial Coronal Sagittal Foot - Routine Pain, AVN Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD FSE T1 FSE Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR PD SPAIR STIR Protocol Indications Notes Axial Coronal Sagittal Foot - Arthritis Arthritis Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD SPAIR STIR Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR T1 SPIR POST 3D WATS T1 SPIR POST Protocol Indications Notes Axial Coronal Sagittal Great Toe / MTP Joints Turf Toe Smallest Coil Possible (Microcoil if Available) PD FSE T1 FSE PD FSE Sesamoiditis FoV = Mid Metatarsal Through Distal Phalanges PD SPAIR PD SPAIR PD SPAIR Slice thickness = 2-3 mm, 10% gap Axial = In relation to the great toe (short axis foot) Coronal = In relation to the great toe (long axis foot / footprint) Appropriate Coronal Plane for Both Ankle and Foot Imaging UT Southwestern Department -

Differential Diagnosis and Treatment of Iliotibial Band Pain Secondary to a Hypomobile Cuboid in a 24-Year-Old Female Tri-Athlete
INTERNATIONAL ACADEMY OF ORTHOPEDIC MEDICINE VOLUME 4, ISSUE 1 WINTER 2015/2016 Differential Diagnosis and Treatment of Iliotibial Band Pain Secondary to a Hypomobile Cuboid in a 24-Year-Old Female Tri-Athlete Femoroacetabular Impingement in the Adolescent Population: A Review Immediate Changes in Widespread Pressure Pain Sensitivity, Neck Pain, and Cervical Spine Range of Motion after Cervical or Thoracic Thrust Manipulation in Patients with Bilateral Chronic Mechanical Neck Pain: A Randomized Clinical Trial IAOM-US CONNECTION DIRECTORY is published by John Hoops PT, COMT The International Managing Editor Academy of Orthopedic Medicine-US (IAOM-US) Valerie Phelps PT, ScD, OCS, FAAOMPT PO Box 65179 Chief Editor / Education Director Tucson, AZ 85728 (p) 866.426.6101 Tanya Smith PT, ScD, FAAOMPT (f) 866.698.4832 Senior Editor (e) [email protected] (w) www.iaom-us.com John Woolf MS, PT, ATC, COMT Business Director CONTACT (p) 866.426.6101 Sharon Fitzgerald (f) 866.698.4832 Executive Assistant (e) [email protected] (w) www.iaom-us.com Andrea Cameron All trademarks are the property Administrative Assistant/ of their respective owners. Marketing Liaison The IAOM-US CONNECTION VOLUME 4 CONNECTION Differential Diagnosis and Dear Colleagues: Treatment of Iliotibial Band Pain Secondary to a Hypomobile Cuboid We hope you’ve had a happy and healthy 2015 2 in a 24-Year-Old Female Tri-Athlete and are ready to set your sights on 2016. Our 2016 course schedule is set, though we’re always adding new course locations and topics. If you haven’t had a chance to see what’s coming to your neck of the woods, here’s a link to the schedule. -

Desarrollo De La Podología En España
Desarrollo de la podología en España Virginia Novel Martí ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tdx.cat) i a través del Dipòsit Digital de la UB (diposit.ub.edu) ha estat autoritzada pels titulars dels drets de propietat intelꞏlectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX ni al Dipòsit Digital de la UB. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX o al Dipòsit Digital de la UB (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tdx.cat) y a través del Repositorio Digital de la UB (diposit.ub.edu) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR o al Repositorio Digital de la UB. -

Overuse Injuries in Elite Athletes
ATHLETES: OVERUSE MRI of Overuse INJURIES VERY COMMON Injury in the Elite Athlete • Muscle William B. Morrison, M.D. Associate Professor of • Joints Radiology Thomas Jefferson • Tendon University Hospital Philadelphia, PA USA • Ligament • Bone [email protected] How is this Relevant to My Practice? • High performance athletes get similar injuries as ‘regular’ people… but: – More of them, & at a younger age MUSCLE / SOFT TISSUE – More commonly imaged – Secondary gain involved INJURY • All the cases here are high performance athletes – but most injuries are conventional • Exceptions – Some weird sport-specific patterns of stress and other injuries – Acute injuries as opposed to overuse •Overuse –DOMS Muscle Injury Delayed Onset Muscle • Acute injury Soreness (DOMS) – Tendon – Myotendinous junction • All athletes are susceptible if they – Muscle belly change training regimen • Athletes tend to work out intensely – leads to muscle injury • Rarely imaged (“no pain no gain”) – Weightlifting / aerobic exercise – 24hr later – soreness – Can be severe, even look like a tear 1 Acute Muscle Injury • Direct → muscle belly, esp quadriceps T2 – esp rugby, football • Indirect → myotendinous junction – eccentric contraction – sudden acceleration / DOMS: Lateral gastrocnemius deceleration Finding can be subtle, even with T2 and fat sat Professional football player Acute Injury – T1 Quadriceps hematoma Muscle belly injury Myotendinous Unit Hit with helmet • Myotendinous Junction – ‘weak link’ of normal myotendinous complex T2 – Common place for injury – Most common mechanism: eccentric contraction (muscle lengthens and contracts at the same High time) T1 = blood Gastrocnemius tear: Grade 1 Muscle Strain “V” sign • Ill-defined edema T2 T1 STIR Weishaupt D, JCAT 2001; 25:677 2 Gd Gd can help identify Grade 2 Muscle Strain subtle muscle injury AKA “Partial Tear” STIR Professional baseball player Grade 1 strain Sartorius m. -

Information to Users
INFORMATION TO USERS This manuscript has been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter free, i ^ e others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely afreet reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand comer and continuing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. Higher quality 6” x 9” black and white photographic prints are available for any photographs or illustrations appearing in this copy for an additional charge. Contact UMI directly to order. UMI A Bell & Howell Information Compaiy 300 North Zeeb Road, Ann Arbor MI 48106-1346 USA 313/761-4700 800/521-0600 PHYSIOLOGIC RESPONSES TO INFLAMMATION IN ISOLATED EQUINE JOINTS DISSERTATION Presented in Partial Fulfilment of the Requirements for the Degree of Doctor of Philosophy in the Graduate School of The Ohio State University B y Joanne Hardy, D.V.M., M.S. -
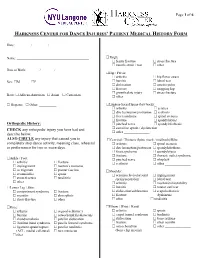
Harkness Center for Dance Injuries' Patient Medical History Form
Page 1 of 6 HARKNESS CENTER FOR DANCE INJURIES’ PATIENT MEDICAL HISTORY FORM Date: ________ / ________ / ________ Name: __________________________________________ Thigh: femur fracture stress fracture muscle strain / tear other_______________ Date of Birth: _______ / _______ / _______ Hip / Pelvis: arthritis hip flexor strain Sex: M F bursitis labral tear dislocation osteitis pubis fracture snapping hip growth plate injury stress fracture Race: African-American Asian Caucasian other _______________ Hispanic Other: __________ Lumbar-Sacral Spine (low back): arthritis sciatica disc herniation/protrusion scoliosis facet syndrome spinal stenosis fracture spondylolysis Orthopedic History: pinched nerve spondylolisthesis CHECK any orthopedic injury you have had and sacroiliac sprain / dysfunction other _______________ describe below. ALSO CIRCLE any injury that caused you to Cervical / Thoracic Spine (neck / mid back)/Ribs: completely stop dance activity, meaning class, rehearsal arthritis spinal stenosis or performance for two or more days. disc herniation/protrusion spondylolisthesis facet syndrome spondylolysis fracture thoracic outlet syndrome Ankle / Foot: pinched nerve whiplash arthritis fracture scoliosis other _______________ impingement morton’s neuroma os trigonum plantar fasciitis Shoulder: sesamoiditis sprain acromioclavicular joint impingement stress fracture tendinitis sprain/separation labral tear other________________ arthritis mechanical instability Lower Leg / Shin: -

Cuboid Syndrome in a College Basketball Player: a Case Report
CASE REVIEW Joseph J. Piccininni, Report Editor Cuboid Syndrome in a College Basketball Player: A Case Report Stephanie M. Mazerolle, PhD, ATC • University of Connecticut UBOID SYNDROME is a condition involv- Table 1. Clinical Presentation ing some degree of disruption of the of Cuboid Subluxation C normal structural congruity of the calca- • No edema or discoloration neo-cuboid (CC) joint.1-3 The condition is associated with several clinical terms for • Pain that may radiate to heel, mimicking heel spur midfoot pathology, including cuboid fault syndrome, pain dropped cuboid, subluxed cuboid, and lateral plantar • May or may not present with palpable defect in neuritis. The literature suggests that cuboid subluxation plantar fascia is associated with a lateral ankle sprain mechanism, • Point tenderness at calcaneo-cuboid joint and styloid occurring most often with a combination of inversion process of 5th metatarsal and plantar flexion.4 The inversion ankle sprain is the • Inability to “work through” the pain during the push- most common athletic injury, which accounts for 10- off phase of the gait cycle 15% of all sport participation time lost to injury.5 • Increased pain with stair climbing 1 Cuboid subluxations and dislocations are rare. The • Increased pain with side-to-side movements or majority of such cases reported in the literature have lateral movements involved long distance runners and ballet dancers.1,4 CC joint dysfunction following a traumatic episode usually results from a dislocation or subluxation injury, but lateral aspect of the foot. She reported having expe- foot pain and chronic instability of the lateral column rienced a traumatic episode three weeks earlier. -

Management Strategies for Cuboid Syndrome
CASE REVIEW Joe J. Piccininni, EdD, CAT(C) Management Strategies for Cuboid Syndrome Jennifer L. Roney, MS, ATC • University of Utah; Melissa L. Yamashiro, ATC • Orthopedic Specialty Group; and Charlie A. Hicks-Little, PhD, ATC • University of Utah Cuboid syndrome refers to a subluxation and Woodle3 reported that nearly all cases of the cuboid or calcaneo-cuboid joint dys- of cuboid syndrome were associated with function.1,2 Cuboid syndrome only accounts pes planus. Pronation of the subtalar joint for 4% of sports-related foot injuries, but provides the peroneal longus muscle with a represents 17% of foot injuries among ballet greater mechanical advantage.5 The intrinsic dancers.2,3 The purpose of this report is to foot muscles, predominantly the flexors, are present an effective management strategy believed to play an important role in stabiliz- for cuboid syndrome. ing the transverse tarsal joint during gait.4 The stability of the Current conservative management of Key PointsPoints articulation between the cuboid syndrome includes manual therapy, Cuboid syndrome is rarely found in ath- cuboid and the distal taping, padding, and use of an orthosis.5-10 letes, other than ballet dancers. portion of the calca- Newell and Woodle3 described a cuboid neus is maintained by manipulation technique that was later Current management options include a number of ligaments referred to as the “black snake heel whip.”1 manual techniques, taping, padding, and and a joint capsule. The patient stands with the affected leg in orthotics. The peroneus longus a knee-flexed, non-weight-bearing position. tendon runs through The clinician grasps the forefoot, placing the The “four mini-stirrup” taping can help the peroneal groove on thumbs on the plantar aspect of the cuboid manage cuboid syndrome. -

Overuse Injuries & Special Skeletal Injuries Dr M.Taghavi
Overuse Injuries & special skeletal injuries Dr M.Taghavi Director of sport medicine center of olympic academy Created with Print2PDF. To remove this line, buy a license at: http://www.software602.com/ Prevalence of Overuse Injuries 30 to 50% of all sport injuries are from overuse In some sports such as distance running, swimming, rock climbing ,and pitching the majority of injuries are from overuse Created with Print2PDF. To remove this line, buy a license at: http://www.software602.com/ Examples of Overuse Injuries Tendonitis Tenosynovitis Shin splints = posterior tibial tendonitis Cuboid Syndrome Patellar alignment and compression syndromes Runner’s knee = illiotibial band tendonitis Created with Print2PDF. To remove this line, buy a license at: http://www.software602.com/ Examples of Overuse Injuries Swimmer’s shoulder and pitcher’s shoulder = rotator cuff tendonitis Pitcher’s or little league elbow = flexor/pronator tendonitis; medial epicondylitis Stress fracture Osgood Schlatter Disease Calcaneal Apophysitis Created with Print2PDF. To remove this line, buy a license at: http://www.software602.com/ Examples of Overuse Injuries Jumper’s Knee = Patellar tendonitis Plantar Fascitis/Heal Spur Syndrome Created with Print2PDF. To remove this line, buy a license at: http://www.software602.com/ Causes of Overuse Injuries Training errors Muscle imbalance Lack of flexibility Malalignment of body structures Over training Poor equipment Poor foot mechanics (over pronation) Created with Print2PDF. To remove this line, buy a license at: http://www.software602.com/ Prevention of Overuse Injuries Slow progression in training overload Increase training overload no more than 10% per week Improve flexibility Improve muscle strength in agonist vs. antagonist muscles Look for worn out equipment/shoes Created with Print2PDF. -

Ankle Injuries
Sport & Exercise Medicine Ankle Injury Differential Resident Guidebook Ankle Injuries Achilles tendon sprain/tear Peroneal tendinopathy Extensor Hallucis Longus Tenosynovitis Peroneal subluxation Weber Fracture Stress fracture Calcaneal bursitis Calcaneal fracture Base of 5th metatarsal fracture/stress fracture/Jones fracture/Pseudo-Jones Medial Tibial Stress syndrome/ reaction/fracture Posterior tibial tendon dysfunction Tibialis Anterior Tenosynovitis Tibialis Posterior tendinopathy Synovitis FHL tendinitis Posterior tibial artery pseudoaneurysm Referred Pain Image retrieved from: https://humananatomycharty.com/anatomy-of-the-foot-ligaments- and-tendons/anatomy-of-the-foot-ligaments-and-tendons-foot-anatomy-tendons-ankle- anatomy-ligaments-and-tendons-ankle/ Dr. A Francella MD CCFP, Dr. Neil Dilworth CCFP (SEM, EM), Dr. Mark Leung CCFP (SEM) 1 Sport & Exercise Medicine Ankle Injury Differential Resident Guidebook Syndesmotic sprain/tear AITFL Sprain/Tear Anterior Impingement Anterolateral Impingement PITFL Sprain/Tear Posterior Impingement PTFL Sprain/Tear Os trigonum syndrome Referred pain CFL Sprain/Tear Sinus Tarsi Coarctation of talocalcaneal ATFL Sprain/Tear Chronic Lateral Ankle Instability Gout Cuboid avulsion fracture Pseudogout Cuboid syndrome Talar dome fracture Osteochondritis dissecans Pilon/Plafond fracture Osteochondral defect Deltoid Sprain/Tear Spring ligament sprain/tear Navicular fracture Navicular impingement Os Naviculare synchondrosis Coarctation of calcaneonavicular Images retrieved from: Dr. A Francella MD CCFP, -

Rotator Cuff Tendinitis Shoulder Joint Replacement Mallet Finger Low
We would like to thank you for choosing Campbell Clinic to care for you or your family member during this time. We believe that one of the best ways to ensure quality care and minimize reoccurrences is through educating our patients on their injuries or diseases. Based on the information obtained from today's visit and the course of treatment your physician has discussed with you, the following educational materials are recommended for additional information: Shoulder, Arm, & Elbow Hand & Wrist Spine & Neck Fractures Tears & Injuries Fractures Diseases & Syndromes Fractures & Other Injuries Diseases & Syndromes Adult Forearm Biceps Tear Distal Radius Carpal Tunnel Syndrome Cervical Fracture Chordoma Children Forearm Rotator Cuff Tear Finger Compartment Syndrome Thoracic & Lumbar Spine Lumbar Spine Stenosis Clavicle Shoulder Joint Tear Hand Arthritis of Hand Osteoporosis & Spinal Fx Congenital Scoliosis Distal Humerus Burners & Stingers Scaphoid Fx of Wrist Dupuytren's Comtracture Spondylolysis Congenital Torticollis Shoulder Blade Elbow Dislocation Thumb Arthritis of Wrist Spondylolisthesis Kyphosis of the Spine Adult Elbow Erb's Palsy Sprains, Strains & Other Injuries Kienböck's Disease Lumbar Disk Herniation Scoliosis Children Elbow Shoulder Dislocation Sprained Thumb Ganglion Cyst of the Wrist Neck Sprain Scoliosis in Children Diseases & Syndromes Surgical Treatments Wrist Sprains Arthritis of Thumb Herniated Disk Pack Pain in Children Compartment Syndrome Total Shoulder Replacement Fingertip Injuries Boutonnière Deformity Treatment -

Preventing Musculoskeletal Injury (MSI) for Musicians and Dancers
Preventing Musculoskeletal Injury (MSI) for Musicians and Dancers A Resource Guide Preventing Musculoskeletal Injury (MSI) for Musicians and Dancers A Resource Guide June 6, 2002 About SHAPE SHAPE (Safety and Health in Arts Production and Entertainment) is an industry association dedicated to promoting health and safety in film and television production, theatre, dance, music, and other performing arts industries in British Columbia. SHAPE provides information, education, and other services that help make arts production and entertainment workplaces healthier and safer. For more information, contact: SHAPE (Safety and Health in Arts Production and Entertainment) Suite 280–1385 West 8th Avenue Vancouver, BC V6H 3V9 Phone: 604 733-4682 in the Lower Mainland 1 888 229-1455 toll-free Fax: 604 733-4692 E-mail: [email protected] Web site: www.shape.bc.ca © 2002 Safety and Health in Arts Production and Entertainment (SHAPE). All rights reserved. SHAPE encourages the copying, reproduction, and distribution of this document to promote health and safety in the workplace, provided that SHAPE is acknowledged. However, no part of this publication may be copied, reproduced, or distributed for profit or other commercial enterprise, nor may any part be incorporated into any other publication, without written permission of SHAPE. National Library of Canada Cataloguing in Publication Data Robinson, Dan. Preventing musculoskeletal injury (MSI) for musicians and dancers : a resource guide Writers: Dan Robinson, Joanna Zander and B.C. Research. Cf. Acknowledgments. Includes bibliographical references: p. ISBN 0-7726-4801-8 1. Musculoskeletal system - Wounds and injuries - Prevention. 2. Entertainers - Wounds and injuries - Prevention. 3. Musicians - Wounds and injuries - Prevention.