Hand Anatomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
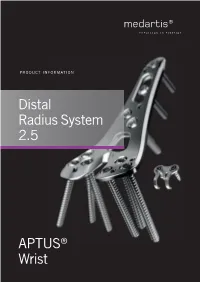
Distal Radius System 2.5
PRODUCT INFORMATION Distal Radius System 2.5 APTUS® Wrist 2 | Distal Radius System 2.5 Contents 3 A New Generation of Radius Plates 4 One System for Primary and Secondary Reconstruction 6 ADAPTIVE II Distal Radius Plates 8 FPL Plates 10 Hook Plates 11 Lunate Facet Plates 12 Rim Plates 13 Fracture Plates 14 Correction Plates 15 Volar Frame Plates 16 Extra-Articular Plates 17 Small Fragment Plates 18 Dorsal Frame Plates 19 XL Plates 20 Distal Ulna Plates 21 Fracture Treatment Concept 22 Technology, Biomechanics, Screw Features 24 Precisely Guided Screw Placement 25 Instrument for Reconstruction of the Volar Tilt 26 Storage 27 Overview Screw Trajectories 29 Ordering Information 47 Bibliography For further information regarding the APTUS product line visit: www.medartis.com Medartis, APTUS, MODUS, TriLock, HexaDrive and SpeedTip are registered trademarks of Medartis AG / Medartis Holding AG, 4057 Basel, Switzerland www.medartis.com Distal Radius System 2.5 | 3 A New Generation of Radius Plates Why is a new generation of radius plates needed? Distal radius fractures are the most common fractures of the stable plate systems have enabled open reduction and inter- upper extremities. The knowledge of these fractures has grown nal fixation to become an established treatment method for enormously over the last years. Treatment concepts have like- intra- and extra-articular distal radius fractures. These sys- wise been refined. It is now generally accepted that the best tems have enabled even severe extension fractures with dor- possible anatomical reconstruction of the radiocarpal joint sal defect zones to be precisely repositioned and treated with (RCJ) and distal radioulnar joint (DRUJ) to produce a func- osteosynthesis via volar access without the need for additional tional outcome is a requirement. -

Intrinsic Hand Muscles of the Japanese Monkey, Macaca Fuscata
Anthropol.Sci. 102(Suppl.), 85-95,1994 Intrinsic Hand Muscles of the Japanese Monkey, Macaca fuscata TOSHIHIKO HOMMA AND TATSUO SAKAI Department of Anatomy, School of Medicine, Juntendo University, Hongo 2-1-1, Bunkyo-ku, Tokyo 113, Japan Received December 24, 1993 •ôGH•ô Abstract•ôGS•ô Anatomy of the intrinsic hand muscles in the Japanese monkeys was studied with an improved method to dissect the muscles and nerves in water after removal of the skeletal framework. The thenar eminence contained four muscles, namely m. abductor pollicis brevis, m. opponens pollicis, m, flexor pollicis brevis, and m. adductor pollicis. The hypothenar eminence contained four muscles, namely m. palmaris brevis, m. abductor digiti minimi, m. flexor digiti minimi brevis, and m. opponens digiti minimi. Majority of the thenar muscles are fused more or less with each other, so that clear separation of these muscles was difficult. The lumbrical muscles arose from the palmar parts of four main tendons of the deep flexor muscle to the second, third, fourth, and fifth digits. The mm, contrahentes arose mainly from a medial tendinous septum attached on the palmar surface to the third metacarpus, and included three muscles destined to the second, fourth and fifth digits. The interossei were found on the radial side of the second, third, fourth and fifth finger as well as on the ulnar side of the second, third and fourth finger. The intrinsic hand muscles in the Japanese monkey received innervation either from the median or the ulnar nerve. Branching pattern of these nerves to the individual muscles was fundamentally similar to those in man except for the fact that the median and the ulnar nerve in the Japanese monkey do not communi cateto make a loop in the thenar muscles. -

Carpal Tunnel Syndrome
Information O from Your Family Doctor Carpal Tunnel Syndrome What is carpal tunnel syndrome? hands a lot. You may notice that over time your Carpal tunnel syndrome (KAR-pal TUN-el grip gets weaker and you tend to drop heavy SIN-drome) is a common, painful disorder objects. of the wrist and hand. It happens when the median nerve, which runs through the wrist, How is it diagnosed? gets squeezed under a band of tissue called a Talk to your doctor if you are having these ligament. This causes pain and other symptoms symptoms. He or she will ask questions about along the nerve (see drawing). the ways you use your hands and about specific What causes it? Anything that increases Shading indicates area pressure on the median where symptoms are felt nerve can cause carpal tunnel syndrome. Sometimes pregnancy and health conditions like arthritis and diabetes can increase the pressure. People who use their hands and wrists repeatedly in the same way (for example, Transverse typists, carpenters, and carpal cashiers) are more likely to get ligament carpal tunnel syndrome. What are the symptoms? Carpal tunnel syndrome Thenar may cause pain, numbness, muscles Wrist or tingling in your wrist and bone hand, mostly in the middle finger, index finger, and Tendon thumb. The symptoms are Median usually worse at night and nerve when you use your wrists and ILLUSTRATION BY KATHRYN BORN continued O Page 1 of 2 Information O from Your Family Doctor Carpal Tunnel Syndrome (continued) symptoms in each part of your hand and wrist. He or she may also test how your nerves and Notes: muscles respond to electrical stimulation. -

6.3.3 Distal Radius and Wrist
6 Specific fractures 6.3 Forearm and hand 6.3.3 Distal radius and wrist 1 Assessment 657 1.1 Biomechanics 657 1.2 Pathomechanics and classification 657 1.3 Imaging 658 1.4 Associated lesions 659 1.5 Decision making 659 2 Surgical anatomy 660 2.1 Anatomy 660 2.2 Radiographic anatomy 660 2.3 Preoperative planning 661 2.4 Surgical approaches 662 2.4.1 Dorsal approach 2.4.2 Palmar approach 3 Management and surgical treatment 665 3.1 Type A—extraarticular fractures 665 3.2 Type B—partial articular fractures 667 3.3 Type C—complete articular fractures 668 3.4 Ulnar column lesions 672 3.4.1 Ulnar styloid fractures 3.4.2 Ulnar head, neck, and distal shaft fractures 3.5 Postoperative care 674 3.6 Complications 676 3.7 Results 676 4 Bibliography 677 5 Acknowledgment 677 656 PFxM2_Section_6_I.indb 656 9/19/11 2:45:49 PM Authors Daniel A Rikli, Doug A Campbell 6.3.3 Distal radius and wrist of this stable pivot. The TFCC allows independent flexion/ 1 Assessment extension, radial/ulnar deviation, and pronation/supination of the wrist. It therefore plays a crucial role in the stability of 1.1 Biomechanics the carpus and forearm. Significant forces are transmitted across the ulnar column, especially while making a tight fist. The three-column concept (Fig 6.3.3-1) [1] is a helpful bio- mechanical model for understanding the pathomechanics of 1.2 Pathomechanics and classification wrist fractures. The radial column includes the radial styloid and scaphoid fossa, the intermediate column consists of the Virtually all types of distal radial fractures, with the exception lunate fossa and sigmoid notch (distal radioulnar joint, DRUJ), of dorsal rim avulsion fractures, can be produced by hyper- and the ulnar column comprises the distal ulna (DRUJ) with extension forces [2]. -

Sustentaculum Lunatum: Appreciation of the Palmar Lunate Facet in Management of Complex Intra-Articular Fractures of the Distal Radius
A Review Paper Sustentaculum Lunatum: Appreciation of the Palmar Lunate Facet in Management of Complex Intra-Articular Fractures of the Distal Radius Ebrahim Paryavi, MD, MPH, Matthew W. Christian, MD, W. Andrew Eglseder, MD, and Raymond A. Pensy, MD key role in restoring the anatomy of the palmar distal radial Abstract metaphysis during internal fixation. This fragment in com- Fracture of the distal radius is the most common wrist minuted fractures was first ascribed special importance by injury. Treatment of complex intra-articular fractures of Melone5 in his description of common fracture patterns. In the distal radius requires an accurate diagnosis of the the present article, we describe the anatomical characteristics fracture pattern and a thoughtful approach to fixation. of the sustentaculum lunatum and the clinical relevance of We propose a new term, sustentaculum lunatum, for this fragment to management of fractures of the distal radius. the palmar lunate facet. The sustentaculum lunatum deserves specific attention because of its importance Classification in load transmission across the radiocarpal joint. It is A variety of classification systems have been proposed to char- acterize and guide treatment of fractures of the distal radius. also key to restoring the anatomy of the palmarAJO distal The earliest descriptions of fracture patterns were presented by radial metaphysis during internal fixation. We provide Castaing6 and Frykman7 in the 1960s. The Frykman classifica- a review of the structure and function of the susten- tion historically has been popular but is limited in accuracy in taculum lunatum and describe fixation techniques. This its characterization of fragments and their displacement and is article is intended to promote awareness of this frag- limited in its ability to guide treatment. -

Table 9-10 Ligaments of the Wrist and Their Function
Function and Movement of the Hand 283 Table 9-10 Ligaments of the Wrist and Their Function Extrinsic Ligaments Function Palmar radiocarpal Volarly stabilizes radius to carpal bones; limits excessive wrist extension Dorsal radiocarpal Dorsally stabilizes radius to carpal bones; limits excessive wrist flexion Ulnar collateral Provides lateral stability of ulnar side of wrist between ulna and carpals Radial collateral Provides lateral stability of radial side of wrist between radius and carpals Ulnocarpal complex and articular Stabilizes and helps glide the ulnar side of wrist; stabilizes distal disk (or triangular fibrocartilage radioulnar joint complex) Intrinsic Ligaments Palmar midcarpal Forms and stabilizes the proximal and distal rows of carpal bones Dorsal midcarpal Forms and stabilizes the proximal and distal rows of carpal bones Interosseous Intervenes between each carpal bone contained within its proximal or distal row Accessory Ligament Transverse carpal Stabilizes carpal arch and contents of the carpal tunnel Adapted from Hertling, D., & Kessler, R. (2006). Management of common musculoskeletal disorders: Physical therapy principles and methods. Philadelphia, PA: Lippincott, Williams & Wilkins.; Oatis, C. A. (2004). Kinesiology: The mechanics and pathomechanics of human movement. Philadelphia, PA: Lippincott, Williams & Wilkins.; Weiss, S., & Falkenstein, N. (2005). Hand rehabilitation: A quick reference guide and review. St. Louis, MO: Mosby Elsevier. The radial and ulnar collateral ligaments provide lateral and medial support, respectively, to the wrist joint. The ulnocarpal complex is more likely to be referred to as the triangular fibro- cartilage complex (TFCC) and includes the articular disk of the wrist. The TFCC is the major stabilizer of the distal radioulnar joint (DRUJ) and can tear after direct compressive force such as a fall on an outstretched hand. -

REVIEW ARTICLE Osteoarthritis of the Wrist
REVIEW ARTICLE Osteoarthritis of the Wrist Krista E. Weiss, Craig M. Rodner, MD From Harvard College, Cambridge, MA and Department of Orthopaedic Surgery, University of Connecticut Health Center, Farmington, CT. Osteoarthritis of the wrist is one of the most common conditions encountered by hand surgeons. It may result from a nonunited or malunited fracture of the scaphoid or distal radius; disruption of the intercarpal, radiocarpal, radioulnar, or ulnocarpal ligaments; avascular necrosis of the carpus; or a developmental abnormality. Whatever the cause, subsequent abnormal joint loading produces a spectrum of symptoms, from mild swelling to considerable pain and limitations of motion as the involved joints degenerate. A meticulous clinical and radiographic evaluation is required so that the pain-generating articulation(s) can be identi- fied and eliminated. This article reviews common causes of wrist osteoarthritis and their surgical treatment alternatives. (J Hand Surg 2007;32A:725–746. Copyright © 2007 by the American Society for Surgery of the Hand.) Key words: Wrist, osteoarthritis, arthrodesis, carpectomy, SLAC. here are several different causes, both idio- of events is analogous to SLAC wrist and has pathic and traumatic, of wrist osteoarthritis. been termed scaphoid nonunion advanced collapse Untreated cases of idiopathic carpal avascular (SNAC). Wrist osteoarthritis can also occur second- T 1 2 necrosis, as in Kienböck’s or Preiser’s disease, may ary to an intra-articular fracture of the distal radius or result in radiocarpal arthritis. Congenital wrist abnor- ulna or from an extra-articular fracture resulting in malities, such as Madelung’s deformity,3,4 can lead malunion and abnormal joint loading. -

Readingsample
Color Atlas of Human Anatomy Vol. 1: Locomotor System Bearbeitet von Werner Platzer 6. durchges. Auflage 2008. Buch. ca. 480 S. ISBN 978 3 13 533306 9 Zu Inhaltsverzeichnis schnell und portofrei erhältlich bei Die Online-Fachbuchhandlung beck-shop.de ist spezialisiert auf Fachbücher, insbesondere Recht, Steuern und Wirtschaft. Im Sortiment finden Sie alle Medien (Bücher, Zeitschriften, CDs, eBooks, etc.) aller Verlage. Ergänzt wird das Programm durch Services wie Neuerscheinungsdienst oder Zusammenstellungen von Büchern zu Sonderpreisen. Der Shop führt mehr als 8 Millionen Produkte. 130 Upper Limb: Bones, Ligaments, Joints Radiocarpal and Midcarpal Joints Ligaments in the Region of the Wrist (A–E) (A–E) Four groups of ligaments can be distin- The radiocarpal or wrist joint is an ellip- guished: soid joint formed on one side by the radius (1) and the articular disk (2) and on the Ligaments which unite the forearm bones with other by the proximal row of carpal bones.Not the carpal bones (violet). These include the all the carpal bones of the proximal row are ulnar collateral ligament (8), the radial col- in continual contact with the socket- lateral ligament (9), the palmar radiocarpal shaped articular facet of the radius and the ligament (10), the dorsal radiocarpal liga- disk. The triquetrum (3), only makes close ment (11), and the palmar ulnocarpal liga- contact with the disk during ulnar abduc- ment (12). tion and loses contact on radial abduction. Ligaments which unite the carpal bones with The capsule of the wrist joint is lax, dorsally one another,orintercarpal ligaments (red). These comprise the radiate carpal ligament Upper Limb relatively thin, and is reinforced by numer- ous ligaments. -

Musculoskeletal Ultrasound Technical Guidelines III. Wrist
European Society of MusculoSkeletal Radiology Musculoskeletal Ultrasound Technical Guidelines III. Wrist Ian Beggs, UK Stefano Bianchi, Switzerland Angel Bueno, Spain Michel Cohen, France Michel Court-Payen, Denmark Andrew Grainger, UK Franz Kainberger, Austria Andrea Klauser, Austria Carlo Martinoli, Italy Eugene McNally, UK Philip J. O’Connor, UK Philippe Peetrons, Belgium Monique Reijnierse, The Netherlands Philipp Remplik, Germany Enzo Silvestri, Italy Wrist Note The standard US examination of the wrist begins with evaluation of its dorsal aspect, followed by the palmar one. Depending on the specific clinical presentation, US images can be obtained in different position of the wrist (flexion and extension, radial and ulnar deviation, pronation and supination), with the patient seated in front of the examiner. 1 DORSAL WRIST: compartments of extensor tendons Place the transducer on a transverse plane over the dorsal aspect of the wrist to allow proper identification of the extensor tendons. In general, one should first recognize a given tendon and then follow it on short-axis planes down to the distal insertion. Long- axis US images of the extensor tendons are less useful: they may help to evaluate the integrity of tendons and assess their dynamic motion in detail. Dynamic scanning of the extensor tendons can be performed by placing the hand on a gel tube with the fingers hanging outside its edge to allow easy fingers movements. Legend: APL, abductor pollicis longus; EPB, extensor pollicis brevis; ECRL, extensor carpi radialis longus; EPCB, extensor carpi radialis brevis; EPL, extensor pollicis longus; EIP, extensor indicis proprius; EDC, extensor digitorum longus; EDQ, extensor digiti quinti proprius; ECU, extensor carpi ulnaris 2 first compartment Keeping the patient’s wrist halfway between pronation and supination, place the probe over the lateral aspect of the radial styloid to examine the first compartment of the extensor tendons - abductor pollicis longus (ventral) and extensor pollicis brevis (dorsal). -

Bones and Joints of the Upper Limb: Forearm and Hand
Unit 4: Bones and joints of the upper limb: forearm and hand Chapter 6 (Upper limb) GENERAL OBJECTIVES: - recognize, name and correctly orient forearm and hand bones - understand movements in elbow, wrist and hand joints SPECIFIC OBJECTIVES: Bones of the forearm and hand Identify the bony features on each part of the following bones: RADIUS - Upper End - Shaft - Lower End ULNA - Upper End - Shaft - Lower End Deduce (from the shape of the articular surfaces) the movements at (i) the elbow joint and (ii) the radioulnar joints. Indicate the bony attachments of the major ligaments which help to maintain the stability of these joints (while allowing their mobility). Identify the following bones CARPALS - Proximal Row - Distal Row METACARPALS PHALANGES Identify the attachments of the Flexor Retinaculum and define the "Carpal Tunnel". Deduce (from the shape of the articular surfaces) the movements at (i) the wrist joint (ii) the carpometacarpal joint of the thumb (iii) metacarpophalangeal joints (iv) interphalangeal joints Indicate the bony attachments of the major ligaments which help to maintain the stability of these joints (while allowing their mobility). Joints of the forearm and hand Elbow Joint Articular Surfaces (Humeroulnar & Humeroradial) Fibrous Capsule & Joint Cavity Synovial Membrane Collateral Ligaments ( Medial & Lateral) Special Structures: Olecranon Bursa Other Bursae, Pads of Fat Movements at the Elbow Joint: Flexion/Extension Stability Carrying Angle Radioulnar Joints Proximal Radioulnar Joint Annular Ligament Distal Radioulnar -

Palmar Plating of Distal Radius Fractures – Pearls and Pitfalls
Palmar Plating of Distal Radius Fractures – Pearls and Pitfalls Michael S. Bednar, M.D. Chief, Hand Surgery Professor, Dept. of Ortho Surgery & Rehab Loyola University – Chicago Disclosure n Consultant – Biomet/Zimmer Evolution in Treatment of Distal Radius Fractures 1 External Fixation and Percutaneous Pinning External Fixation and Percutaneous Pinning External Fixation 2 Percutaneous Pinning Percutaneous Pinning Old ORIF concept: n Dorsally displaced = Dorsal plate n Palmarly displaced = Palmar plate 3 Goals of Treatment n ORIF n Indications n Displaced palmar intra and extra- articular fractures ORIF n Palmar Barton and Smith Fractures n ORIF is accepted form of treatment n Palmar plate is well tolerated n Exposure radial to FCR has low morbidity 4 Cohort Studies Volar Fixed Angle n Orbay, J. L., Fernandez, D.L. (2002). 31 partients n Kamano, M., Y. Honda, et al. (2002). 33 patients Follows the contour of the subchondral bone Pegs and screw locked into plate support articular surface when placed directed under the subchondral bone. 5 Distally angled pegs neutralize dorsal forces Joint Reaction Force §.Volar buttress neutralizes volar forces Volar locking plating indications • Dorsal or palmar angulation • Intra-articular fractures • Comminuted fractures • Osteopenia Volar locking plating indications • Dorsal or palmar angulation • Intra-articular fractures • Comminuted fractures • Osteopenia 6 3 Months Post OP Wrist Fractures = ORIF 7 ORIF 8 No metal over radial styloid, causes tendon ruputure Complications – Wrong Fracture Type n -

Nerve Transfer Techniques in Injuries from the Upper Limb
THIEME Update Article | Artículo de Actualización 57 Nerve Transfer Techniques in Injuries from the Upper Limb Técnicas de transferencia nerviosa en lesiones del miembro superior Francisco Martínez Martínez1 B. Ñíguez Sevilla2 J. García García2 A. García López3 1 FEA (field medcial expert), Orthopaedics and Traumatology Surgery, Address for correspondence Francisco Martínez Martínez, C/ Canovas Hospital Clínico Universitario Virgen de la Arrixaca. Murcia, Spain del Castillo n°7- 4°a. 30003-Murcia, Spain 2 Resident, Orthopaedics and Traumatology Surgery, Hospital Clínico (e-mail: [email protected]). Universitario Virgen de la Arrixaca, Murcia, Spain 3 FEA (field medcial expert), Orthopaedics and Traumatology Surgery, Hospital General de Alicante, Alicante, Spain Rev Iberam Cir Mano 2017;45:57–67. Abstract Proximal nerve injuries from the upper limb or the braquial plexus are associated with a poor prognosis, even with prompt repair. In the last few decades an increase in nerve transfer techniques has occurred, by which a denervated peripheral nerve is reinner- vated by a healthy donor nerve. Nerve transfers are indicated in proximal brachial plexus injuries where grafting is not possible or in proximal injuries of peripheral nerves with long reinnervation distances. Nerve transfers represent a revolution in peripheral nerve surgery and offer the potential for superior functional recovery in severe nerve injuries. In complete brachial plexus injuries, there are being studied the existence of nerve roots (intraplexual transfers). If they do not exist, the transference of nerves out of the plexus are used Keywords (extraplexual transfers) as the spinal accessory nerve, the phrenic nerve, the intercostal ► nerve transfers nerves, etc. ► brachial plexus In this update paper, the different motor intra and extraplexual nerve transfer ► nerve injury techniques are going to be reviewed.