Torsade De Pointes' Ventricular Tachycardia NICHOLAS G
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The QT Interval: How Long Is Too Long?
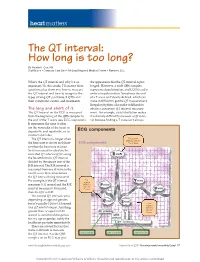
heart matters The QT interval: How long is too long? By Natalie K. Cox, RN Staff Nurse • Coronary Care Unit • McLeod Regional Medical Center • Florence, S.C. What’s the QT interval and why’s it so the appearance that the QT interval is pro- important? In this article, I’ll answer these longed. However, a wide QRS complex questions plus show you how to measure represents depolarization, and LQTS is a dis- the QT interval and how to recognize the order of repolarization. Sometimes the end types of long QT syndrome (LQTS) and of a T wave isn’t clearly defi ned, which can their symptoms, causes, and treatments. make it diffi cult to get the QT measurement. Irregular rhythms also make it diffi cult to The long and short of it obtain a consistent QT interval measure- The QT interval on the ECG is measured ment. For example, atrial fi brillation makes from the beginning of the QRS complex to it extremely diffi cult to measure a QT inter- the end of the T wave (see ECG components). val because fi nding a T wave isn’t always It represents the time it takes for the ventricles of the heart to depolarize and repolarize, or to ECG components contract and relax. The QT interval is longer when First positive deflection after the the heart rate is slower and short- ECG components P or Q wave er when the heart rate is faster. So it’s necessary to calculate the corrected QT interval (QTc) using the Bazett formula: QT interval divided by the square root of the R-R interval. -

Computational Diagnostic Techniques for Electrocardiogram Signal Analysis
sensors Review Computational Diagnostic Techniques for Electrocardiogram Signal Analysis Liping Xie * , Zilong Li, Yihan Zhou, Yiliu He and Jiaxin Zhu College of Medicine and Biological Information Engineering, Northeastern University, Shenyang 110169, China; [email protected] (Z.L.); [email protected] (Y.Z.); [email protected] (Y.H.); [email protected] (J.Z.) * Correspondence: [email protected] Received: 8 September 2020; Accepted: 4 November 2020; Published: 5 November 2020 Abstract: Cardiovascular diseases (CVDs), including asymptomatic myocardial ischemia, angina, myocardial infarction, and ischemic heart failure, are the leading cause of death globally. Early detection and treatment of CVDs significantly contribute to the prevention or delay of cardiovascular death. Electrocardiogram (ECG) records the electrical impulses generated by heart muscles, which reflect regular or irregular beating activity. Computer-aided techniques provide fast and accurate tools to identify CVDs using a patient’s ECG signal, which have achieved great success in recent years. Latest computational diagnostic techniques based on ECG signals for estimating CVDs conditions are summarized here. The procedure of ECG signals analysis is discussed in several subsections, including data preprocessing, feature engineering, classification, and application. In particular, the End-to-End models integrate feature extraction and classification into learning algorithms, which not only greatly simplifies the process of data analysis, but also shows excellent accuracy and robustness. Portable devices enable users to monitor their cardiovascular status at any time, bringing new scenarios as well as challenges to the application of ECG algorithms. Computational diagnostic techniques for ECG signal analysis show great potential for helping health care professionals, and their application in daily life benefits both patients and sub-healthy people. -

Long QT Syndrome: from Channels to Cardiac Arrhythmias
Long QT syndrome: from channels to cardiac arrhythmias Arthur J. Moss, Robert S. Kass J Clin Invest. 2005;115(8):2018-2024. https://doi.org/10.1172/JCI25537. Review Series Long QT syndrome, a rare genetic disorder associated with life-threatening arrhythmias, has provided a wealth of information about fundamental mechanisms underlying human cardiac electrophysiology that has come about because of truly collaborative interactions between clinical and basic scientists. Our understanding of the mechanisms that control the critical plateau and repolarization phases of the human ventricular action potential has been raised to new levels through these studies, which have clarified the manner in which both potassium and sodium channels regulate this critical period of electrical activity. Find the latest version: https://jci.me/25537/pdf Review series Long QT syndrome: from channels to cardiac arrhythmias Arthur J. Moss1 and Robert S. Kass2 1Heart Research Follow-up Program, Department of Medicine, University of Rochester School of Medicine and Dentistry, Rochester, New York, USA. 2Department of Pharmacology, Columbia University Medical Center, New York, New York, USA. Long QT syndrome, a rare genetic disorder associated with life-threatening arrhythmias, has provided a wealth of information about fundamental mechanisms underlying human cardiac electrophysiology that has come about because of truly collaborative interactions between clinical and basic scientists. Our understanding of the mecha- nisms that control the critical plateau and repolarization phases of the human ventricular action potential has been raised to new levels through these studies, which have clarified the manner in which both potassium and sodium channels regulate this critical period of electrical activity. -

Anemia and the QT Interval in Hypertensive Patients
2084 International Journal of Collaborative Research on Internal Medicine & Public Health Anemia and the QT interval in hypertensive patients Ioana Mozos 1*, Corina Serban 2, Rodica Mihaescu 3 1 Department of Functional Sciences, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania 2 Department of Functional Sciences, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania 3 1st Department of Internal Medicine, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania * Corresponding Author ; Email: [email protected] Abstract Introduction: A prolonged ECG QT interval duration and an increased QT dispersion (QTd) are predictors of sudden cardiac death. Anemia is known as a marker of adverse outcome in cardiovascular disease. Objective: The aim was to assess the relationship between anemia and QT intervals in hypertensive patients. Method: A total of 72 hypertensive patients underwent standard 12-lead ECG. QT intervals and QT dispersions were manually measured. Complete blood count was also assessed. Result: Linear regression analysis revealed significant associations between prolonged QTc and increased QTd and anemia and macrocytosis, respectively. Multiple regression analysis revealed a significant association between red cell distribution width (RDW) >15% and prolonged heart rate corrected maximal QT interval duration (QTc) and QT interval in lead DII (QTIIc). The most sensitive and specific predictor of prolonged QTc and QTIIc was anisocytosis. Anemia was the most sensitive predictor of -

Nitric Oxide-Mediated Flow-Dependent Dilation Is Impaired in Coronary Arteries in Patients with Coronary Spastic Angina
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector 920 JACC Vol. 30, No. 4 October 1997:920–6 Nitric Oxide-Mediated Flow-Dependent Dilation Is Impaired in Coronary Arteries in Patients With Coronary Spastic Angina KIYOTAKA KUGIYAMA, MD, MASAMICHI OHGUSHI, MD, TAKESHI MOTOYAMA, MD, SEIGO SUGIYAMA, MD, HISAO OGAWA, MD, MICHIHIRO YOSHIMURA, MD, YOSHITO INOBE, MD, OSAMU HIRASHIMA, MD, HIROAKI KAWANO, MD, HIROFUMI SOEJIMA, MD, HIROFUMI YASUE, MD Kumamoto City, Japan Objectives. This study sought to examine whether flow- Results. Flow-dependent dilation of the proximal LAD was dependent dilation is impaired at the site of coronary artery found to be less in spasm arteries than in control arteries. G spasm in patients with coronary spastic angina. Infusion of N -monomethyl-L-arginine (L-NMMA) in the proxi- Background. Physiologic stimuli such as exercise and exposure mal LAD suppressed flow-dependent dilation in control arteries to cold have been shown to cause an increase in coronary blood but had no significant effect on spasm arteries. The dilator flow, leading to flow-dependent dilation of coronary arteries in response to nitroglycerin was not impaired in spasm coronary normal subjects, but cause coronary constriction in patients with arteries. coronary spastic angina. Conclusions. Our results indicate that flow-dependent coronary Methods. A maximal increase in blood flow was induced dilation is impaired in spasm arteries, partly due to a deficiency in selectively in the left anterior descending coronary artery (LAD) endothelial nitric oxide bioactivity, which in turn may contribute by infusion of adenosine through a Doppler flow catheter tip in the to the increase in coronary tone during physiologic stimuli in midportion of the LAD in 10 patients with coronary spastic patients with coronary spastic angina. -

Young Adults. Look for ST Elevation, Tall QRS Voltage, "Fishhook" Deformity at the J Point, and Prominent T Waves
EKG Abnormalities I. Early repolarization abnormality: A. A normal variant. Early repolarization is most often seen in healthy young adults. Look for ST elevation, tall QRS voltage, "fishhook" deformity at the J point, and prominent T waves. ST segment elevation is maximal in leads with tallest R waves. Note high take off of the ST segment in leads V4-6; the ST elevation in V2-3 is generally seen in most normal ECG's; the ST elevation in V2- 6 is concave upwards, another characteristic of this normal variant. Characteristics’ of early repolarization • notching or slurring of the terminal portion of the QRS wave • symmetric concordant T waves of large amplitude • relative temporal stability • most commonly presents in the precordial leads but often associated with it is less pronounced ST segment elevation in the limb leads To differentiate from anterior MI • the initial part of the ST segment is usually flat or convex upward in AMI • reciprocal ST depression may be present in AMI but not in early repolarization • ST segments in early repolarization are usually <2 mm (but have been reported up to 4 mm) To differentiate from pericarditis • the ST changes are more widespread in pericarditis • the T wave is normal in pericarditis • the ratio of the degree of ST elevation (measured using the PR segment as the baseline) to the height of the T wave is greater than 0.25 in V6 in pericarditis. 1 II. Acute Pericarditis: Stage 1 Pericarditis Changes A. Timing 1. Onset: Day 2-3 2. Duration: Up to 2 weeks B. Findings 1. -

The Relation Between Arterial Blood Pressure Variables and Ventricular Repolarization Parameters
860 International Journal of Collaborative Research on Internal Medicine & Public Health The relation between arterial blood pressure variables and ventricular repolarization parameters Ioana Mozos 1*, Corina Serban 2, Rodica Mihaescu 3 1 Department of Functional Sciences, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania, [email protected] 2 Department of Functional Sciences, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania 3 Department of Medical Semiology, “Victor Babes” University of Medicine and Pharmacy Timisoara, Romania ABSTRACT Introduction: Ventricular arrhythmia and sudden cardiac death risk are associated with prolonged electrocardiographic (ECG) QT and Tpeak-Tend intervals. Objective: To evaluate the influence of blood pressure variables on ventricular repolarization parameters, especially QT and Tpeak-Tend intervals. Method: Two groups of patients were enrolled in the study. The firs group included 77 patients, with essential hypertension, aged 62±12 years, 40% males. The control group included 56 patients, age and sex matched, with optimal, normal and high normal blood pressure. They underwent 12-lead ECG and ventricular repolarization parameters were assessed. QT intervals: QTmax (maximal QT interval duration), QTc (heart rate corrected QTmax), QTm (mean QT interval duration in all leads), QTIIc (heart rate corrected QT interval duration in lead DII), and T wave variables: T0e (maximal T wave duration), Tpe (maximal Tpeak-Tend interval) and Ta (maximal T wave amplitude) were manually measured. Arterial blood pressure variables: systolic (SBP), diastolic (DBP), mean arterial (MAP) and pulse pressure (PP), were recorded. Result: SBP was 139±24 mmHg, DBP 86±13 mmHg, MAP 103±15 mmHg, PP 53±16 mmHg, QTmax 430±51 ms, QTc 474±48 ms and Tpe 100±26 ms in the hypertensive group. -

Review Article Management of Atrial Fibrillation in Critically Ill Patients
Hindawi Publishing Corporation Critical Care Research and Practice Volume 2014, Article ID 840615, 10 pages http://dx.doi.org/10.1155/2014/840615 Review Article Management of Atrial Fibrillation in Critically Ill Patients Mattia Arrigo, Dominique Bettex, and Alain Rudiger Cardiosurgical Intensive Care Unit, Institute of Anesthesiology, University Hospital Zurich, Raemistraße 100, 8091 Zurich, Switzerland Correspondence should be addressed to Alain Rudiger; [email protected] Received 29 September 2013; Revised 24 December 2013; Accepted 24 December 2013; Published 16 January 2014 AcademicEditor:MarcusJ.Schultz Copyright © 2014 Mattia Arrigo et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Atrial fibrillation (AF) is common in ICU patients and is associated with a two- to fivefold increase in mortality. This paper provides a reappraisal of the management of AF with a special focus on critically ill patients with haemodynamic instability. AF can cause hypotension and heart failure with subsequent organ dysfunction. The underlying mechanisms are the loss of atrial contraction and the high ventricular rate. In unstable patients, sinus rhythm must be rapidly restored by synchronised electrical cardioversion (ECV). If pharmacological treatment is indicated, clinicians can choose between the rate control and the rhythm control strategy. The optimal substance should be selected depending on its potential adverse effects. A beta-1 antagonist with a very short half-life (e.g., esmolol) is an advantage for ICU patients because the effect of beta-blockade on cardiovascular stability is unpredictable in those patients. -

Interpreting CVP Waveforms Summary EK
INTERPRETING CENTRAL VENOUS PRESSURE WAVEFORMS IN TERPRETING CEN TRAL VEN OUS PRESSURE W AVEFORMS INTRODUCTION A central venous pressure waveform provides important information about the hemodynamic state of the patient and compliance of the syste m. - CENTRAL VEN OUS PRESSURE (CVP) W AVEFORMS • Measures pressure in the central venous circulation • Obtained by using a central venous catheter ideally placed at the junction of the superior vena cava (SVC) and the right atrium • Depends on: 1. Compliance of the cardiovascular system 2. Overall volume status Figure 1: Central venou s catheter placement at the SV C-RA junction INTERPRETING CVP W AVEFORMS Remember that the waveform represents atrial pressure which is the relationship between atrial compliance and volume. One CVP Waveform represents one complete beat of the heart. • a-wave: atrial contraction • Corresponds with timing of P wave on ECG • Noncompliant right atrium: = large a-wave • c-wave: movement of the tric uspid valve into the right atrium • Corresponds with timing of R wave on ECG • Transient decrease in atrial compliance/increase in atrial pressure • c-wave and a-wave can be difficult to differentiate when patient is ta tachycardic • x-descent: atrial relaxation • Corresponds with timing of QRS complex on ECG Figure 2: The different parts of a central venous • Tricuspid valve descends towards the apex of the right ventricle pressure waveform causing a decrease in right atrial pressure • v-wave: atrial filling • Corresponds with timing of T wave on ECG • A large v-wave may indicate tricuspid regurgitation QRS • If right atrium is very compliant, tricuspid regurgitation is possible complex without generation of large v-wave • y-descent: atrial emptying • Corresponds with timing just prior to P wave on ECG P wave T wave Figure 3: ECG showing timing of CVP waveform components This document is meant to be used as an educational resource for physicians and other healthcare professionals. -

Ventricular Repolarization Components on the Electrocardiogram Cellular Basis and Clinical Significance Gan-Xin Yan, MD, PHD, Ramarao S
View metadata, citation and similar papers at core.ac.uk brought to you by CORE Journal of the American College of Cardiology providedVol. by Elsevier 42, No. - 3,Publisher 2003 Connector © 2003 by the American College of Cardiology Foundation ISSN 0735-1097/03/$30.00 Published by Elsevier Inc. doi:10.1016/S0735-1097(03)00713-7 STATE-OF-THE-ART PAPER Ventricular Repolarization Components on the Electrocardiogram Cellular Basis and Clinical Significance Gan-Xin Yan, MD, PHD, Ramarao S. Lankipalli, MD, James F. Burke, MD, FACC, Simone Musco, MD, Peter R. Kowey, MD, FACC Wynnewood, Pennsylvania Ventricular repolarization components on the surface electrocardiogram (ECG) include J (Osborn) waves, ST-segments, and T- and U-waves, which dynamically change in morphol- ogy under various pathophysiologic conditions and play an important role in the development of ventricular arrhythmias. Our primary objective in this review is to identify the ionic and cellular basis for ventricular repolarization components on the body surface ECG under normal and pathologic conditions, including a discussion of their clinical significance. A specific attempt to combine typical clinical ECG tracings with transmembrane electrical recordings is made to illustrate their logical linkage. A transmural voltage gradient during initial ventricular repolarization, which results from the presence of a prominent transient ϩ outward K current (Ito)-mediated action potential (AP) notch in the epicardium, but not endocardium, manifests as a J-wave on the ECG. The J-wave is associated with the early repolarization syndrome and Brugada syndrome. ST-segment elevation, as seen in Brugada syndrome and acute myocardial ischemia, cannot be fully explained by using the classic concept of an “injury current” that flows from injured to uninjured myocardium. -

Determinants of Myocardial Lactate Production During Acetylcholine
ORIGINAL RESEARCH Determinants of Myocardial Lactate Production During Acetylcholine Provocation Test in Patients With Coronary Spasm Koichi Kaikita, MD, PhD; Masanobu Ishii, MD; Koji Sato, MD, PhD; Masafumi Nakayama, MD, PhD; Yuichiro Arima, MD, PhD; Tomoko Tanaka, MD, PhD; Koichi Sugamura, MD, PhD; Kenji Sakamoto, MD, PhD; Yasuhiro Izumiya, MD, PhD; Eiichiro Yamamoto, MD, PhD; Kenichi Tsujita, MD, PhD; Megumi Yamamuro, MD, PhD; Sunao Kojima, MD, PhD; Hirofumi Soejima, MD, PhD; Seiji Hokimoto, MD, PhD; Kunihiko Matsui, MD, MPH; Hisao Ogawa, MD, PhD Background-—Myocardial lactate production in the coronary circulation during acetylcholine (ACh)-provocation test (abbreviated as lactate production) provides supporting evidence for coronary spasm–induced myocardial ischemia. The purpose of this study was to examine the clinical features, predictive factors, and prognosis of patients with coronary vasospastic angina (VSA) and lactate production. Methods and Results-—We examined all 712 patients who underwent both myocardial lactate measurement during ACh- provocation test in the left coronary artery and genetic screening test of a –786T/C polymorphism in the 50-flanking region of the endothelial nitric oxide synthase (eNOS) gene between January 1991 and December 2010. Lactate production was observed in 252 of the 712 patients and in 219 of 356 VSA patients diagnosed by ACh-provocation test. Compared with lactate production– negative VSA patients, the lactate production–positive counterparts were more likely to be nonsmoker female diabetics with – 786T/C eNOS polymorphism (61% vs 31%, P<0.001, 62% vs 34%, P<0.001, 24% vs 14%, P=0.016, and 25% vs 15%, P=0.018, respectively). Multivariable logistic regression analysis identified female sex, diabetes mellitus, and –786T/C eNOS polymorphism to correlate with lactate production (odds ratio 3.51, 95% CI 2.16 to 5.70, P<0.001; odds ratio 2.53, 95% CI 1.38 to 4.65, P=0.003; and odds ratio 1.85, 95% CI 1.02 to 3.35, P=0.044, respectively). -

Tively Assess Myocardial Function: New Hypothesis and Validation Experiment Regarding the U Wave
Journal of ISSN:2378-6914 Heart and Cardiology OPEN ACCESS Research Article DOI: 10.15436/2378-6914.20.2813 Changing Electrocardiogram Waveforms to Quantita- tively Assess Myocardial function: New Hypothesis and Validation Experiment regarding the U Wave Kenneth Tsan He1*, Helena Ai He2 1Princeton International School of Mathematics and Science, 11th grade student, 19 Lambert Drive, Princeton 2Princeton International School of Mathematics and Science, 10th grade student, 19 Lambert Drive, Princeton *Corresponding author: Kenneth Tsan He, Princeton International School of Mathematics and Science, 11th grade student, 19 Lambert Drive, Princeton, NJ, Tel: 08540; 1-732-705-0282; Email: [email protected] Abstract A hypothesis regarding the U wave is proposed, where the collision of the heart apex and chest wall causes delayed repolar- ization of some myocardial cells due to compression and deformation, leading to the presence of the U wave on ECG. Under normal conditions, the stronger the myocardial contractility, the greater the mass of the heart, the closer the distance to the chest wall, the more intense the apex beat, the more cells deformed and repolarization delayed, and the longer the delay time. To test the hypothesis, 41 high school student volunteers participated in a clinical trial. The results showed that when the position was changed from the supine position to the left lateral position, the U wave increased significantly (0.24±0.095×0.1 mv, a=99%), the T wave significantly decreased (-1.3±0.74×0.1 mv, a=99%), the time difference between the two peaks significantly increased (0.38±0.12×40 ms, a= 99%), indicating a strong co-rrelation between those three values ( r= 0.87 and 0.39).