Study Guide for the MOC Cognitive Examination: Musculoskeletal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Juvenile Spondyloarthropathies: Inflammation in Disguise
PP.qxd:06/15-2 Ped Perspectives 7/25/08 10:49 AM Page 2 APEDIATRIC Volume 17, Number 2 2008 Juvenile Spondyloarthropathieserspective Inflammation in DisguiseP by Evren Akin, M.D. The spondyloarthropathies are a group of inflammatory conditions that involve the spine (sacroiliitis and spondylitis), joints (asymmetric peripheral Case Study arthropathy) and tendons (enthesopathy). The clinical subsets of spondyloarthropathies constitute a wide spectrum, including: • Ankylosing spondylitis What does spondyloarthropathy • Psoriatic arthritis look like in a child? • Reactive arthritis • Inflammatory bowel disease associated with arthritis A 12-year-old boy is actively involved in sports. • Undifferentiated sacroiliitis When his right toe starts to hurt, overuse injury is Depending on the subtype, extra-articular manifestations might involve the eyes, thought to be the cause. The right toe eventually skin, lungs, gastrointestinal tract and heart. The most commonly accepted swells up, and he is referred to a rheumatologist to classification criteria for spondyloarthropathies are from the European evaluate for possible gout. Over the next few Spondyloarthropathy Study Group (ESSG). See Table 1. weeks, his right knee begins hurting as well. At the rheumatologist’s office, arthritis of the right second The juvenile spondyloarthropathies — which are the focus of this article — toe and the right knee is noted. Family history is might be defined as any spondyloarthropathy subtype that is diagnosed before remarkable for back stiffness in the father, which is age 17. It should be noted, however, that adult and juvenile spondyloar- reported as “due to sports participation.” thropathies exist on a continuum. In other words, many children diagnosed with a type of juvenile spondyloarthropathy will eventually fulfill criteria for Antinuclear antibody (ANA) and rheumatoid factor adult spondyloarthropathy. -

Bone and Soft Tissue Tumors Have Been Treated Separately
EPIDEMIOLOGY z Sarcomas are rare tumors compared to other BONE AND SOFT malignancies: 8,700 new sarcomas in 2001, with TISSUE TUMORS 4,400 deaths. z The incidence of sarcomas is around 3-4/100,000. z Slight male predominance (with some subtypes more common in women). z Majority of soft tissue tumors affect older adults, but important sub-groups occur predominantly or exclusively in children. z Incidence of benign soft tissue tumors not known, but Fabrizio Remotti MD probably outnumber malignant tumors 100:1. BONE AND SOFT TISSUE SOFT TISSUE TUMORS TUMORS z Traditionally bone and soft tissue tumors have been treated separately. z This separation will be maintained in the following presentation. z Soft tissue sarcomas will be treated first and the sarcomas of bone will follow. Nowhere in the picture….. DEFINITION Histological z Soft tissue pathology deals with tumors of the classification connective tissues. of soft tissue z The concept of soft tissue is understood broadly to tumors include non-osseous tumors of extremities, trunk wall, retroperitoneum and mediastinum, and head & neck. z Excluded (with a few exceptions) are organ specific tumors. 1 Histological ETIOLOGY classification of soft tissue tumors tumors z Oncogenic viruses introduce new genomic material in the cell, which encode for oncogenic proteins that disrupt the regulation of cellular proliferation. z Two DNA viruses have been linked to soft tissue sarcomas: – Human herpes virus 8 (HHV8) linked to Kaposi’s sarcoma – Epstein-Barr virus (EBV) linked to subtypes of leiomyosarcoma z In both instances the connection between viral infection and sarcoma is more common in immunosuppressed hosts. -
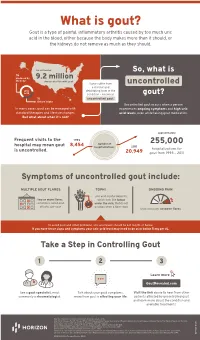
Uncontrolled Gout Fact Sheet
What is gout? Gout is a type of painful, inflammatory arthritis caused by too much uric acid in the blood, either because the body makes more than it should, or the kidneys do not remove as much as they should. An estimated So, what is ⅔ produced by 9.2 million the body Americans live with gout Some suffer from uncontrolled a chronic and uric debilitating form of the acid condition – known as gout? ⅓ uncontrolled gout. dietary intake Uncontrolled gout occurs when a person In many cases, gout can be managed with experiences ongoing symptoms and high uric standard therapies and lifestyle changes. acid levels, even while taking gout medication. But what about when it’s not? approximately Frequent visits to the 1993 number of 255,000 hospital may mean gout 8,454 hospitalizations 2011 is uncontrolled. hospitalizations for 20,949 gout from 1993 – 2011 Symptoms of uncontrolled gout include: MULTIPLE GOUT FLARES TOPHI ONGOING PAIN uric acid crystal deposits, two or more flares, which look like lumps sometimes called gout under the skin, that do not attacks, per year go away when a flare stops that continues between flares To avoid gout and other problems, uric acid levels should be 6.0 mg/dL or below. If you have these signs and symptoms your uric acid level may need to be at or below 5 mg per dL. Take a Step in Controlling Gout 1 2 3 Learn more GoutRevealed.com See a gout specialist, most Talk about your gout symptoms, Visit the link above to hear from other commonly a rheumatologist. -

Arthritis (Overview)
ARTHRITIS Having arthritis can significantly affect your comfort & ability to walk and move with confidence. This is because it affects your joints, which are responsible for keeping you steady and moving efficiently. Your symptoms and causes will depend on the type of arthritis that you have. At Masterton Foot Clinic, our podiatrists work closely with patients with four types of arthritis. OSTEOARTHRITIS Osteoarthritis is the wear and tear arthritis that develops slowly over time as the cartilage that covers your bone ends wears down. The cause is largely from natural use over many years, though injuries, alignment issues within the joint and other diseases may result in it developing at a faster rate. We work with patients that want to feel more comfortable on their feet, despite having arthritis in their hip, knee, ankle and foot joints. RHEUMATOID ARTHRITIS Rheumatoid arthritis is an autoimmune disease that affects the joints. It occurs when your body’s immune system attacks the joints and causes damage, inflammation and pain. If the effects of rheumatoid arthritis remain uncontrolled, it can cause permanent changes in the appearance of the joints, especially at the feet and hands. We work with patients to help them manage the discomfort associated with rheumatoid arthritis, offloading prominent and painful areas that have developed due to changes in the joints. GOUT Gout is an inflammatory arthritis that results from a high concentration of uric acid in the blood. It is associated with a high intake of purine-containing foods like red meats, shellfish and red wine, hence it was previously referred to as the rich man’s disease. -

Exostoses, Enchondromatosis and Metachondromatosis; Diagnosis and Management
Acta Orthop. Belg., 2016, 82, 102-105 ORIGINAL STUDY Exostoses, enchondromatosis and metachondromatosis; diagnosis and management John MCFARLANE, Tim KNIGHT, Anubha SINHA, Trevor COLE, Nigel KIELY, Rob FREEMAN From the Department of Orthopaedics, Robert Jones Agnes Hunt Hospital, Oswestry, UK We describe a 5 years old girl who presented to the region of long bones and are composed of a carti- multidisciplinary skeletal dysplasia clinic following lage lump outside the bone which may be peduncu- excision of two bony lumps from her fingers. Based on lated or sessile, the knee is the most common clinical examination, radiolographs and histological site (1,10). An isolated exostosis is a common inci- results an initial diagnosis of hereditary multiple dental finding rarely requiring treatment. Disorders exostosis (HME) was made. Four years later she developed further lumps which had the radiological associated with exostoses include HME, Langer- appearance of enchondromas. The appearance of Giedion syndrome, Gardner syndrome and meta- both exostoses and enchondromas suggested a possi- chondromatosis. ble diagnosis of metachondromatosis. Genetic testing Enchondroma are the second most common be- revealed a splice site mutation at the end of exon 11 on nign bone tumour characterised by the formation of the PTPN11 gene, confirming the diagnosis of meta- hyaline cartilage in the medulla of a bone. It occurs chondromatosis. While both single or multiple exosto- most frequently in the hand (60%) and then the feet. ses and enchondromas occur relatively commonly on The typical radiological features are of a well- their own, the appearance of multiple exostoses and defined lucent defect with endosteal scalloping and enchondromas together is rare and should raise the differential diagnosis of metachondromatosis. -

SKELETAL DYSPLASIA Dr Vasu Pai
SKELETAL DYSPLASIA Dr Vasu Pai Skeletal dysplasia are the result of a defective growth and development of the skeleton. Dysplastic conditions are suspected on the basis of abnormal stature, disproportion, dysmorphism, or deformity. Diagnosis requires Simple measurement of height and calculation of proportionality [<60 inches: consideration of dysplasia is appropriate] Dysmorphic features of the face, hands, feet or deformity A complete physical examination Radiographs: Extremities and spine, skull, Pelvis, Hand Genetics: the risk of the recurrence of the condition in the family; Family evaluation. Dwarf: Proportional: constitutional or endocrine or malnutrition Disproportion [Trunk: Extremity] a. Height < 42” Diastrophic Dwarfism < 48” Achondroplasia 52” Hypochondroplasia b. Trunk-extremity ratio May have a normal trunk and short limbs (achondroplasia), Short trunk and limbs of normal length (e.g., spondylo-epiphyseal dysplasia tarda) Long trunk and long limbs (e.g., Marfan’s syndrome). c. Limb-segment ratio Normal: Radius-Humerus ratio 75% Tibia-Femur 82% Rhizomelia [short proximal segments as in Achondroplastics] Mesomelia: Dynschondrosteosis] Acromelia [short hands and feet] RUBIN CLASSIFICATION 1. Hypoplastic epiphysis ACHONDROPLASTIC Autosomal Dominant: 80%; 0.5-1.5/10000 births Most common disproportionate dwarfism. Prenatal diagnosis: 18 weeks by measuring femoral and humeral lengths. Abnormal endochondral bone formation: zone of hypertrophy. Gene defect FGFR fibroblast growth factor receptor 3 . chromosome 4 Rhizomelic pattern, with the humerus and femur affected more than the distal extremities; Facies: Frontal bossing; Macrocephaly; Saddle nose Maxillary hypoplasia, Mandibular prognathism Spine: Lumbar lordosis and Thoracolumbar kyphosis Progressive genu varum and coxa valga Wedge shaped gaps between 3rd and 4th fingers (trident hands) Trident hand 50%, joint laxity Pathology Lack of columnation Bony plate from lack of growth Disorganized metaphysis Orthopaedics 1. -

Paleopathological Analysis of a Sub-Adult Allosaurus Fragilis (MOR
Paleopathological analysis of a sub-adult Allosaurus fragilis (MOR 693) from the Upper Jurassic Morrison Formation with multiple injuries and infections by Rebecca Rochelle Laws A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science in Earth Sciences Montana State University © Copyright by Rebecca Rochelle Laws (1996) Abstract: A sub-adult Allosaurus fragilis (Museum of the Rockies specimen number 693 or MOR 693; "Big Al") with nineteen abnormal skeletal elements was discovered in 1991 in the Upper Jurassic Morrison Formation in Big Horn County, Wyoming at what became known as the "Big Al" site. This site is 300 meters northeast of the Howe Quarry, excavated in 1934 by Barnum Brown. The opisthotonic position of the allosaur indicated that rigor mortis occurred before burial. Although the skeleton was found within a fluvially-deposited sandstone, the presence of mud chips in the sandstone matrix and virtual completeness of the skeleton showed that the skeleton was not transported very far, if at all. The specific goals of this study are to: 1) provide a complete description and analysis of the abnormal bones of the sub-adult, male, A. fragilis, 2) develop a better understanding of how the bones of this allosaur reacted to infection and trauma, and 3) contribute to the pathological bone database so that future comparative studies are possible, and the hypothesis that certain abnormalities characterize taxa may be evaluated. The morphology of each of the 19 abnormal bones is described and each disfigurement is classified as to its cause: 5 trauma-induced; 2 infection-induced; 1 trauma- and infection-induced; 4 trauma-induced or aberrant, specific origin unknown; 4 aberrant; and 3 aberrant, specific origin unknown. -

Gout and Monoarthritis
Gout and Monoarthritis Acute monoarthritis has numerous causes, but most commonly is related to crystals (gout and pseudogout), trauma and infection. Early diagnosis is critical in order to identify and treat septic arthritis, which can lead to rapid joint destruction. Joint aspiration is the gold standard method of diagnosis. For many reasons, managing gout, both acutely and as a chronic disease, is challenging. Registrars need to develop a systematic approach to assessing monoarthritis, and be familiar with the management of gout and other crystal arthropathies. TEACHING AND • Aetiology of acute monoarthritis LEARNING AREAS • Risk factors for gout and septic arthritis • Clinical features and stages of gout • Investigation of monoarthritis (bloods, imaging, synovial fluid analysis) • Joint aspiration techniques • Interpretation of synovial fluid analysis • Management of hyperuricaemia and gout (acute and chronic), including indications and targets for urate-lowering therapy • Adverse effects of medications for gout, including Steven-Johnson syndrome • Indications and pathway for referral PRE- SESSION • Read the AAFP article - Diagnosing Acute Monoarthritis in Adults: A Practical Approach for the Family ACTIVITIES Physician TEACHING TIPS • Monoarthritis may be the first symptom of an inflammatory polyarthritis AND TRAPS • Consider gonococcal infection in younger patients with monoarthritis • Fever may be absent in patients with septic arthritis, and present in gout • Fleeting monoarthritis suggests gonococcal arthritis or rheumatic fever -

WHO Manual of Diagnostic Imaging Radiographic Anatomy and Interpretation of the Musculoskeletal System
The WHO manual of diagnostic imaging Radiographic Anatomy and Interpretation of the Musculoskeletal System Editors Harald Ostensen M.D. Holger Pettersson M.D. Authors A. Mark Davies M.D. Holger Pettersson M.D. In collaboration with F. Arredondo M.D., M.R. El Meligi M.D., R. Guenther M.D., G.K. Ikundu M.D., L. Leong M.D., P. Palmer M.D., P. Scally M.D. Published by the World Health Organization in collaboration with the International Society of Radiology WHO Library Cataloguing-in-Publication Data Davies, A. Mark Radiography of the musculoskeletal system / authors : A. Mark Davies, Holger Pettersson; in collaboration with F. Arredondo . [et al.] WHO manuals of diagnostic imaging / editors : Harald Ostensen, Holger Pettersson; vol. 2 Published by the World Health Organization in collaboration with the International Society of Radiology 1.Musculoskeletal system – radiography 2.Musculoskeletal diseases – radiography 3.Musculoskeletal abnormalities – radiography 4.Manuals I.Pettersson, Holger II.Arredondo, F. III.Series editor: Ostensen, Harald ISBN 92 4 154555 0 (NLM Classification: WE 141) The World Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in full. Applications and enquiries should be addressed to the Office of Publications, World Health Organization, CH-1211 Geneva 27, Switzerland, which will be glad to provide the latest information on any changes made to the text, plans for new editions, and reprints and translations already available. © World Health Organization 2002 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. -

(Ollier Disease, Maffucci Syndrome) Is Not Caused by the PTHR1 Mutation
Enchondromatosis (Ollier Disease, Maffucci Syndrome) Is Not Caused by the PTHR1 Mutation p.R150C Bovée, J.V.M.G.; Rozeman, L.B.; Sangiorgi, L.; Briaire-de Bruijn, I.H.; Mainil-Varlet, P.; Bertoni, F.; ... ; Hogendoorn, P.C.W. Citation Bovée, J. V. M. G., Rozeman, L. B., Sangiorgi, L., Briaire-de Bruijn, I. H., Mainil-Varlet, P., Bertoni, F., … Hogendoorn, P. C. W. (2004). Enchondromatosis (Ollier Disease, Maffucci Syndrome) Is Not Caused by the PTHR1 Mutation p.R150C. Human Mutation, 24, 466-473. Retrieved from https://hdl.handle.net/1887/8144 Version: Not Applicable (or Unknown) License: Downloaded from: https://hdl.handle.net/1887/8144 Note: To cite this publication please use the final published version (if applicable). HUMAN MUTATION 24:466^473 (2004) RAPID COMMUNICATION Enchondromatosis (Ollier Disease, Maffucci Syndrome) Is Not Caused by the PTHR1 Mutation p.R150C Leida B. Rozeman,1 Luca Sangiorgi,2 Inge H. Briaire-de Bruijn,1 Pierre Mainil-Varlet,3 F. Bertoni,4 Anne Marie Cleton-Jansen,1 Pancras C.W. Hogendoorn,1 and Judith V.M.G. Bove´e1* 1Department of Pathology, Leiden University Medical Center, Leiden, The Netherlands; 2Laboratory of Oncology Research, Rizzoli Orthopedic Institute, Bologna, Italy; 3Institute of Pathology, University of Bern, Bern, Switzerland; 4Department of Pathology, Rizzoli Orthopedic Institute, Bologna, Italy Communicated by Arnold Munnich Enchondromatosis (Ollier disease, Maffucci syndrome) is a rare developmental disorder characterized by multiple enchondromas. Not much is known about its molecular genetic background. Recently, an activating mutation in the parathyroid hormone receptor type 1 (PTHR1) gene, c.448C>T (p.R150C), was reported in two of six patients with enchondromatosis. -

Blueprint Genetics Comprehensive Growth Disorders / Skeletal
Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel Test code: MA4301 Is a 374 gene panel that includes assessment of non-coding variants. This panel covers the majority of the genes listed in the Nosology 2015 (PMID: 26394607) and all genes in our Malformation category that cause growth retardation, short stature or skeletal dysplasia and is therefore a powerful diagnostic tool. It is ideal for patients suspected to have a syndromic or an isolated growth disorder or a skeletal dysplasia. About Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders This panel covers a broad spectrum of diseases associated with growth retardation, short stature or skeletal dysplasia. Many of these conditions have overlapping features which can make clinical diagnosis a challenge. Genetic diagnostics is therefore the most efficient way to subtype the diseases and enable individualized treatment and management decisions. Moreover, detection of causative mutations establishes the mode of inheritance in the family which is essential for informed genetic counseling. For additional information regarding the conditions tested on this panel, please refer to the National Organization for Rare Disorders and / or GeneReviews. Availability 4 weeks Gene Set Description Genes in the Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ACAN# Spondyloepimetaphyseal dysplasia, aggrecan type, AD/AR 20 56 Spondyloepiphyseal dysplasia, Kimberley -

Osteochondrosis – Primary Epiphyseal (Articular/Subchondral) Lesion Can Heal Or Can Progress
60 120 180 1 distal humeral condyles 2 medial epicondyle 3 proximal radial epiphysis 4 anconeal process Lab Ret study N=1018 . Normal . Affected . Total 688 (67.6%) . Total 330 (32.4%) . Male 230 (62.2%) . Male 140 (37.8%) . Female 458 (70.7%) . Female 190 (29.3%) Affected dogs N=330 1affected site - 250 (75.7%) 2 affected sites - 68 (20.6%) 3 affected sites - 12 (3.6%) immature skeletal diseases denis novak technique for skeletal radiography tissue < 12 cm “non-grid” (“table-top”) technique “high detail” system radiation safety diagnosis X – rays examination Ultrasound CT bilateral lesions - clinical signs ? unilateral present > one type of lesion 2ry arthrosis Common Osteochondrosis – primary epiphyseal (articular/subchondral) lesion can heal or can progress Osteochondritis dissecans – free articular fragment will progress Arthrosis Osteochondrosis talus / tarsus Lumbosacral OCD Lumbosacral OCD Inflammatory diseases Panosteitis – non infectious Hypertrophic osteodystrophy (HOD) – perhaps infectious Osteomyelitis - infectious Panosteitis New medullary bone Polyostotic Multiple lesions in one bone Symmetrical or nonsymmetrical Sclerotic pattern B I L A T E R A L periosteal new bone forms with chronicity Cross sections of a tibia different locations Hypertrophic osteodystrophy (HOD) Dogs are systemically ill, febrile, anorectic, reluctant to walk most will recover Radiographic changes of HOD . Polyostotic . Metaphyseal . Symmetrical . Changes of lesion Early Mid Late lytic “plates” in acute case HOD - 4 m ret – lesions are present