Musculoskeletal Radiology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Rare Bone Tumor
OPEN ACCESS L E T T E R T O T H E E D I T O R Periosteal Desmoplastic Fibroma of Radius: A Rare Bone Tumor Aniqua Saleem1,* Hira Saleem2 1 Radiology Department, District Head Quarters Hospital, Rawalpindi Medical University, Rawalpindi 2 Department of Surgery, Shifa International Hospital, Islamabad. Correspondence*: Dr. Aniqua Saleem, Radiology Department, District Head Quarters Hospital, Rawalpindi Medical University, Rawalpindi E-mail: [email protected] © 2019, Saleem et al, Submitted: 05-04-2019 Accepted: 09-06-2019 Conflict of Interest: None Source of Support: Nil This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. DEAR SIR Desmoplastic fibroma is an extremely rare tumor of enhancement on post contrast images and with adjacent bone with a reported incidence of 0.11 % of all primary bone involvement as was evident by focal cortical inter- bone tumors. The most common site of involvement is ruption, mild endosteal thickening and irregularity and mandible (reported incidence 22% of all Desmoplastic also mild ulnar shaft remodeling (Fig. 3a, 3b). To further fibroma cases) followed by metaphysis of long bones. characterize the lesion, Tc99 MDP (methylene diphos- Involvement of forearm especially involving periosteum phonate) bone scan was also performed which showed is seldom reported. Prompt diagnosis and adequate active bone involvement in left distal radial shaft. management is important for limb salvage and restora- tion of limb function. [1-3] An 11-year-old boy presented with painful mild swelling of left forearm for a month, with no significant past med- ical history or any history of trauma. -

A Rare Cause of Lytic Lesion: the Brown Tumors
MOJ Orthopedics & Rheumatology Case Report Open Access A rare cause of lytic lesion: the brown tumors Abstract Volume 11 Issue 6 - 2019 Introduction: Brown tumor is a tumor-like lesion that represents the terminal stage of the bone remodeling process in prolonged hyperparathyroidism and has an overall incidence of Maroua Khaloui, Fatma Daoud, Imène Rachdi, 3%. It may not be distinguishable from other osteolytic lesions of malignancy. We illustrate Mehdi Somai, Hana Zoubeidi, Zohra Aydi, a case of primary hyperparathyroidism with brown tumour which was initially mistaken for Nedia Hammami, Wided Hizem, Besma Ben malignant disease. Dhaou, Fatma Boussema Department of Internal medicine, Habib Thameur Hospital, Tunis Case report: A 64-year-old female patient with a medical history of dyslipidemia repeated El Manar University, Tunisia acute pancreatitis and retrobulbar neuritis was referred to our department for evaluation of hypercalcemia. The association with a hypogammaglobulinemia gave rise to the initial Correspondence: Imène Rachdi, Department of Internal diagnosis of humoral hypercalcemia of multiple myeloma. The radiological evaluation medicine, Habib Thameur Hospital, Tunis El Manar University, Ali of the skeleton showed an isolated lytic lesion on the humerus. No electrophoretic signs Ben Ayed Street, 1089 Tunis, Tunisia, of monoclonal secretion in the blood or urine were found. Nevertheless, laboratory Email investigations revealed a constellation of primary hyperparathyroidism. Computed tomography localized a right parathyroid adenoma, which was surgically removed. Also, Received: October 25, 2019 | Published: November 15, 2019 we concluded that the humeral lesion was in fact a Brown tumor. Conclusion: This case reinforces the need to consider brown tumor of hyperparathyroidism in the differential diagnosis of an osteolytic lesion with hypercalcemia. -
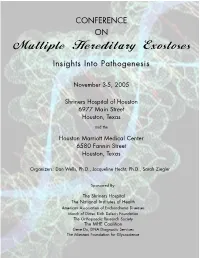
Multiple Hereditary Exostoses Abstract Book, 2005
CONFERENCE ON Multiple Hereditary Exostoses InsightsInsights IntoInto PathogenesisPathogenesis November 3-5, 2005 Shriners Hospital of Houston 6977 Main Street Houston, Texas and the Houston Marriott Medical Center 6580 Fannin Street Houston, Texas Organizers: Dan Wells, Ph.D., Jacqueline Hecht, Ph.D., Sarah Ziegler Sponsored By: The Shriners Hospital The National Institutes of Health American Association of Enchondroma Diseases March of Dimes Birth Defects Foundation The Orthopaedic Research Society The MHE Coalition Gene Dx, DNA Diagnostic Services The Mizutani Foundation for Glycoscience HME: Insights into Pathogenesis. Schedule of Events Thursday November 3, 2005 8:30-9:00 Arrive at Shriners (Coffee and Pastries) 9:00-9:10 Dan Wells, Ph.D. Welcome to conference 9:10-9:30 Jacqueline Hecht, Ph.D. Introduction to genetics and natural history MHE ORTHOPAEDICS AND CLINICAL GENETICS (Christine Alvarez) 9:30-10:10 Christine Alvarez, M.D. Introduction of orthopaedics and defining severity of Hereditary Multiple Exostosis 10:10-10:40 Luca Sangiorgi, M.D., Ph.D. Mutational analysis and clinical expression of disease in patients with HME. 10:40-11:00 BREAK 11:00-11:30 Wim Wuyts, Ph.D. Mutation detection strategies for molecular screening in patients with HME. 11:30-12:00 George Thompson, M.D. Clinical treatments and surgical procedures. 12:00-1:15 LUNCH BONE DEVELOPMENT (Dan Wells) 1:15-1:45 John R. Hassell, Ph.D. FGF binding to percelan isolated from the growth plate. 1:45-2:15 David Ornitz, M.D., Ph.D. FGF that regulate growth plate development. 2:15-2:45 Maurizio Pacifici, M.D., Ph.D. -

Bone and Soft Tissue Tumors Have Been Treated Separately
EPIDEMIOLOGY z Sarcomas are rare tumors compared to other BONE AND SOFT malignancies: 8,700 new sarcomas in 2001, with TISSUE TUMORS 4,400 deaths. z The incidence of sarcomas is around 3-4/100,000. z Slight male predominance (with some subtypes more common in women). z Majority of soft tissue tumors affect older adults, but important sub-groups occur predominantly or exclusively in children. z Incidence of benign soft tissue tumors not known, but Fabrizio Remotti MD probably outnumber malignant tumors 100:1. BONE AND SOFT TISSUE SOFT TISSUE TUMORS TUMORS z Traditionally bone and soft tissue tumors have been treated separately. z This separation will be maintained in the following presentation. z Soft tissue sarcomas will be treated first and the sarcomas of bone will follow. Nowhere in the picture….. DEFINITION Histological z Soft tissue pathology deals with tumors of the classification connective tissues. of soft tissue z The concept of soft tissue is understood broadly to tumors include non-osseous tumors of extremities, trunk wall, retroperitoneum and mediastinum, and head & neck. z Excluded (with a few exceptions) are organ specific tumors. 1 Histological ETIOLOGY classification of soft tissue tumors tumors z Oncogenic viruses introduce new genomic material in the cell, which encode for oncogenic proteins that disrupt the regulation of cellular proliferation. z Two DNA viruses have been linked to soft tissue sarcomas: – Human herpes virus 8 (HHV8) linked to Kaposi’s sarcoma – Epstein-Barr virus (EBV) linked to subtypes of leiomyosarcoma z In both instances the connection between viral infection and sarcoma is more common in immunosuppressed hosts. -

Percutaneous Injection of Calcium Phosphate Composite in Pediatric Unicameral Bone Cysts: a Minimum 5-Year Follow-Up Study
Sport Sciences for Health (2019) 15:207–213 https://doi.org/10.1007/s11332-018-0513-7 ORIGINAL ARTICLE Percutaneous injection of calcium phosphate composite in pediatric unicameral bone cysts: a minimum 5-year follow-up study Marco Turati1,2 · Marco Bigoni2,3 · Lilia Brahim1 · Emeline Bourgeois1 · Giovanni Zatti2,3 · Ahmad Eid1 · Jacques Griffet1 · Aurélien Courvoisier1 Received: 4 September 2018 / Accepted: 9 November 2018 / Published online: 24 November 2018 © Springer-Verlag Italia S.r.l., part of Springer Nature 2018 Abstract Background Unicameral bone cyst (UBC) is a common lesion in skeletally immature patients. Multiple treatments are pro- posed as curettage and autologous bone graft, percutaneous local corticoids injections, decompression with internal fixation, and injection of bioresorbable cement. Decompression, curettage, and percutaneous bioresorbable cement injection showed interesting results, but until now, no long-term follow-up was reported in pediatric patients with UBC. Methods We retrospectively evaluated 13 pediatric patients with UBC treated with curettage, decompression, and injection of a calcium phosphate composite (CPC) at a single institution with an average F-U of 5.46 years (range 5–7 years). Func- tional outcomes were evaluated according to the Musculoskeletal Tumour Society (MSTS) Score. Radiographic healing was assessed with the modified Neer Outcome Rating System. Complications were recorded. Results The mean MSTS score was 29.61 (range 28–30). No joint limitation or any pain was recorded. All patients returned to their previous level of activity. Complete healed cysts were observed in 76.9% of patients (10 of 13) and partially healed in 23.1% (3 of 13). Three fractures of the humerus occurred without any further consequence. -

Benign Fibro-Osseous Lesions Plus…
“Vision is the art of seeing things invisible.” Jonathan Swift 1667 - 1745 Benign Fibro-osseous Lesions Plus… Steven R. Singer, DDS [email protected] 212.305.5674 Benign Fibro-osseous Lesions Fibrous Dysplasia A group of lesions in which normal bone is Localized change in bone metabolism replaced initially by fibrous connective tissue Normal cancellous bone is replaced by Over time, the lesion is infiltrated by osteoid fibrous connective tissue and cementoid tissue The connective tissue contains varying amounts of abnormal bone with irregular This is a benign and idiopathic process trabeculae Trabeculae are randomly oriented. (Remember that normal trabeculae are aligned to respond to stress) Fibrous Dysplasia Fibrous Dysplasia Lesions may be solitary (monostotic) or Fibrous dysplasia is non-hereditary involve more than one bone (polyostotic) Caused by a mutation in a somatic cell. Monostotic form accounts for 70% of all Extent of lesions depends on the timing of cases the mutation. Polyostotic form is more common in the first If the mutation occurs earlier, the disease decade will be more widespread throughout the M=F except in McCune-Albright syndrome, body. An example is McCune-Albright which is almost exclusively found in females Syndrome 1 Fibrous Dysplasia Fibrous Dysplasia McCune-Albright Syndrome • Monostotic and polyostotic forms usually -Almost exclusively begins in the second decade of life females -Polyostotic fibrous • Slow, painless expansion of the jaws dysplasia • Patients may complain of swelling or have -

Sclerodactyly and Digital Osteosclerosis
Postgrad Med J: first published as 10.1136/pgmj.44.513.553 on 1 July 1968. Downloaded from Case reports 553 drain with side holes may be more effective in Acknowledgments allowing access for air than the usual corrugated My thanks are due to Dr I. Howard, Medical Superin- drain. tendent of the Alfred Hospital, Mr R. S. Lawson and Mr (4) The wound should be inspected daily. K. Bradley for permission to publish these case reports. (5) An hourly pulse chart should be kept and any sustained rise immediately reported. It is emphasized that this was the first sign in both References the above patients. BRUMMELKAMP, W.H., BOEREMA, I. & HOOGENDYK, L. (1963) Treatment of clostridial infections with hyperbaric oxygen If gas infection is suspected, vigorous treat- drenching. Lancet, i, 235. ment should be instituted: GYE, R. ROUNTREE, P.M. & LOWENTHAL, J. (1961) Infection (1) The wound should be widely opened and of surgical wounds with Clostridium welchii. Med. J. Aust. a swab taken for bacteriological examination. i, 761. HAM, J.M., MACKENZIE, D.C. & LOWENTHAL, J. (1964) The (2) Blood transfusion should be commenced immediate results of lower limb amputation for atheros- as soon as possible as these patients all have clerosis obliterans. Aust. N.Z. J. Surg. 34, 97. some degree of haemolysis. KARASEWICK, E.G., HARPER, E.M., SHARP, N.C.C., SHIELDS, (3) Penicillin should be given as above. R.S., SMITH, G. & MCDOWALL, D.G. (1964) Hyperbaric (4) Hyperbaric oxygen can be life-saving oxygen in clostridial infections. Clinical Application of Boerema Hyperbaric Oxygen (Ed. -

Treatment of Aneurysmal Bone Cysts with Titanium Elastic Nails in Children
Treatment of Aneurysmal Bone Cysts with Titanium Elastic Nails in Children Yi-chen Wang Children's Hospital of Shanghai Xing Jia Children's Hospital of Shanghai Yang Shen Children's Hospital of Shanghai Sun Wang Children's Hospital of Shanghai Liang-chao Dong Children's Hospital of Shanghai Jing Ren Children's Hospital of Shanghai Li-hua Zhao ( [email protected] ) Research Keywords: Primary aneurysmal bone cyst, Titanium Elastic Nails, recurrence, ecacy Posted Date: July 6th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-38776/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/16 Abstract Background: The main treatment method of the primary aneurysmal bone cyst (ABC) is to curettage and bone grafts with high-speed burring, radiotherapy, sclerotherapy, arterial embolism and hormone therapy can be used for the lesions whose location cannot be easily exposed by the surgery. Regardless of the method, high recurrence rates are a common problem. The purpose of this study was to evaluate retrospectively the use of titanium elastic nails as a internal xation in the treatment of aneurysmal bone cysts in children. Methods: Children with histological primary aneurysmal bone cyst were evaluated between 2010 to 2017. The patients were divided into 2 groups according to the treatment plan. Patients in the study group operated with curettage and bone grafts with high-speed burring + internal xation of titanium elastic nails (TEN), and patients in the control group operated with curettage and bone grafts with high-speed burring. The curative effect of the children in the 2 groups were analyzed statistically according to the imaging results (Neer grading) and MSTS functional evaluation. -

Case Report Chondroblastoma of The
CASE REPORT CHONDROBLASTOMA OF THE PATELLA ASSOCIATED WITH AN ANEURYSMAL BONE CYST R. TREBŠE1, A. ROTTER2,V. PIŠOT1 Chondroblastoma is a rare, benign tumor of bone, cartilage germ cells, and they redefined the tumor accounting for about 1% of all bone tumor cases. It as “benign chondroblastoma”. tends to affect the epiphyseal ends of long bones, Chondroblastoma is rare, representing about 1% most often in males during the first and second of all primary bone tumors (1, 5, 9). It is typically decades of life. It has well-characterized radio- centered in an epiphysis. Although it occurs most graphic and histologic features but despite its histo- often in the end of a long tubular bone, it can logically benign appearance a few cases of metastases appear in any secondary center of ossification. It is have been reported. Local recurrences after curet- tage and bone grafting occur in 11% to 25% of cases. most probably a tumor of cartilaginous origin and The features of a patellar chondroblastoma are the is more common in males by a ratio of about 2-to- same as for other locations. In reviewing the litera- 1 (1, 5, 9). Seventy percent of chondroblastomas ture we found an unusually high male-to-female occur during active epiphyseal plate growth, and ratio. It is interesting that the usual treatment of the about two-thirds of the patients are in the second patellar chondroblastoma has been patellectomy, decade of life (5). whereas curettage and bone grafting has predomi- Local pain of several months’ duration and nated in the other locations. -

University of Bradford Ethesis
University of Bradford eThesis This thesis is hosted in Bradford Scholars – The University of Bradford Open Access repository. Visit the repository for full metadata or to contact the repository team © University of Bradford. This work is licenced for reuse under a Creative Commons Licence. THE IDENTIFICATION OF BOVINE TUBERCULOSIS IN ZOOARCHAEOLOGICAL ASSEMBLAGES VOLUME 1 (1 OF 2) J. E. WOODING PhD UNIVERSITY OF BRADFORD 2010 THE IDENTIFICATION OF BOVINE TUBERCULOSIS IN ZOOARCHAEOLOGICAL ASSEMBLAGES Working towards differential diagnostic criteria Volume 1 (1 of 2) Jeanette Eve WOODING Submitted for the degree of Doctor of Philosophy School of Life Sciences Division of Archaeological, Geographical and Environmental Sciences University of Bradford 2010 Jeanette Eve WOODING The identification of bovine tuberculosis in zooarchaeological assemblages. Working towards differential diagnostic criteria. Keywords: Palaeopathology, zooarchaeology, human osteoarchaeology, zoonosis, Iron Age, Viking Age, Iceland, Orkney, England ABSTRACT The study of human palaeopathology has developed considerably in the last three decades resulting in a structured and standardised framework of practice, based upon skeletal lesion patterning and differential diagnosis. By comparison, disarticulated zooarchaeological assemblages have precluded the observation of lesion distributions, resulting in a dearth of information regarding differential diagnosis and a lack of standard palaeopathological recording methods. Therefore, zoopalaeopathology has been restricted to the analysis of localised pathologies and ‘interesting specimens’. Under present circumstances, researchers can draw little confidence that the routine recording of palaeopathological lesions, their description or differential diagnosis will ever form a standard part of zooarchaeological analysis. This has impeded the understanding of animal disease in past society and, in particular, has restricted the study of systemic disease. -

Bone Grafting in Brodie's Absc Rafting in Brodie's Abscess
Case Report Bone Grafting in Brodie’s Abscess Athar Ahemad Department of Orthopaedics, Indian Institute of Medical Sciences and Research, Warudi, Tq. Badnapur, Jalna, Maharashtra, INDIA. Email: [email protected] Abstract Brodie’s abscess is a localized infection of the bone manifesting on radiographs as an osteolytic lesion limited by sclerotic bone. It was first described by Sir Benjamin Brodie 1in the year 1832 as a localized abscess in the tibia seen in an amputation stump. It is most commonly seen in proximal tibia follo wed by femur and then in humerus. Various treatments have been described in the literature ranging from antibiotics alone to debridement alone to curettage and filling of defect by bone graft or cement 2,3,4. Here, we report 2 cases of Brodie’s abscess tre ated successfully by surgical debridement and bone grafting. Address for Correspondence Dr. Athar Ahemad, Department of Orthopaedics, Indian Institute of Medical Sciences and Research, Warudi, Tq. Badnapur, Jalna, Maharashtra, INDIA. Email: [email protected] Received Date: 13/09/2014 Accepted Date: 17 /0 9/2014 hydrogen peroxide. The cavity was debrided till there was Access this article online bleeding bone all around. Since the bone defect was large (5x3x3cm), fresh cancellous autograft from ipsilateral Quick Response Code: Website: iliac crest was used to fill the defect. Muscle flap st itched www.medpulse.in over the window as a local flap. A long knee brace was given to prevent pathological fracture. DOI: 18 September 2014 INTRODUCTION Case 1 A 24 year old male manual laborer presented to us with complaints of throbbing pain in the upper part of leg on Photo 1: Cavity of the abscess being debrided with a curette which and off since last 4 years especially at night. -

Orthopedic-Conditions-Treated.Pdf
Orthopedic and Orthopedic Surgery Conditions Treated Accessory navicular bone Achondroplasia ACL injury Acromioclavicular (AC) joint Acromioclavicular (AC) joint Adamantinoma arthritis sprain Aneurysmal bone cyst Angiosarcoma Ankle arthritis Apophysitis Arthrogryposis Aseptic necrosis Askin tumor Avascular necrosis Benign bone tumor Biceps tear Biceps tendinitis Blount’s disease Bone cancer Bone metastasis Bowlegged deformity Brachial plexus injury Brittle bone disease Broken ankle/broken foot Broken arm Broken collarbone Broken leg Broken wrist/broken hand Bunions Carpal tunnel syndrome Cavovarus foot deformity Cavus foot Cerebral palsy Cervical myelopathy Cervical radiculopathy Charcot-Marie-Tooth disease Chondrosarcoma Chordoma Chronic regional multifocal osteomyelitis Clubfoot Congenital hand deformities Congenital myasthenic syndromes Congenital pseudoarthrosis Contractures Desmoid tumors Discoid meniscus Dislocated elbow Dislocated shoulder Dislocation Dislocation – hip Dislocation – knee Dupuytren's contracture Early-onset scoliosis Ehlers-Danlos syndrome Elbow fracture Elbow impingement Elbow instability Elbow loose body Eosinophilic granuloma Epiphyseal dysplasia Ewing sarcoma Extra finger/toes Failed total hip replacement Failed total knee replacement Femoral nonunion Fibrosarcoma Fibrous dysplasia Fibular hemimelia Flatfeet Foot deformities Foot injuries Ganglion cyst Genu valgum Genu varum Giant cell tumor Golfer's elbow Gorham’s disease Growth plate arrest Growth plate fractures Hammertoe and mallet toe Heel cord contracture