Diagnosis and Classification of Diabetes Mellitus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter 7: Monogenic Forms of Diabetes
CHAPTER 7 MONOGENIC FORMS OF DIABETES Mark A. Sperling, MD, and Abhimanyu Garg, MD Dr. Mark A. Sperling is Emeritus Professor and Chair, University of Pittsburgh, Department of Pediatrics, Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA. Dr. Abhimanyu Garg is Professor of Internal Medicine and Chief of the Division of Nutrition and Metabolic Diseases at University of Texas Southwestern Medical Center, Dallas, TX. SUMMARY Types 1 and 2 diabetes have multiple and complex genetic influences that interact with environmental triggers, such as viral infections or nutritional excesses, to result in their respective phenotypes: young, lean, and insulin-dependence for type 1 diabetes patients or older, overweight, and often manageable by lifestyle interventions and oral medications for type 2 diabetes patients. A small subset of patients, comprising ~2%–3% of all those diagnosed with diabetes, may have characteristics of either type 1 or type 2 diabetes but have single gene defects that interfere with insulin production, secretion, or action, resulting in clinical diabetes. These types of diabetes are known as MODY, originally defined as maturity-onset diabetes of youth, and severe early-onset forms, such as neonatal diabetes mellitus (NDM). Defects in genes involved in adipocyte development, differentiation, and death pathways cause lipodystrophy syndromes, which are also associated with insulin resistance and diabetes. Although these syndromes are considered rare, more awareness of these disorders and increased availability of genetic testing in clinical and research laboratories, as well as growing use of next generation, whole genome, or exome sequencing for clinically challenging phenotypes, are resulting in increased recognition. A correct diagnosis of MODY, NDM, or lipodystrophy syndromes has profound implications for treatment, genetic counseling, and prognosis. -

DIAGMOL Town, ZIPCODE :…………………………………………………… Director : Prof
Mr. Mrs. (IN UPPER CASE, please) Name:……………………………………………………. Maiden Name:……………………………………. DMGL / Service de Médecine Génétique Centre d’accueil des prélèvements (CAP) First name :………………………………………………… Bâtiment des Laboratoires (BATLab), local 8D-0-850.1 Date of birth : ............ / ........... / …………… 4 rue Gabrielle-Perret-Gentil, 1211 Genève 14 Legal representative (for minors) : father mother Molecular and Genomic Diagnostics Laboratory Name/first name :…………………………………………… Street/N°:……………………………………………………… http://www.hug-ge.ch/feuilles-de-demande DIAGMOL Town, ZIPCODE :…………………………………………………… Director : Prof. Stylianos ANTONARAKIS Hospitalisation Unit: …………… Physician :…………………… Lab managers: N° EdS : …………………………………………………………… Dr J.-L. BLOUIN, Dr Th. NOUSPIKEL, Dr. M. GUIPPONI Invoice address: Patient Prescriptor Insurance [email protected], [email protected], [email protected] Type of case : Disease AI Accident Pregnancy Lab direct or results: Phone/FAX: +41 (0) 22 37 21 826 / 21 860 N° AVS (Mandatory for AI) : ………………………...................... Sample Entrance Center (CAP) : Phone +41 (0) 22 37 21 800 Insurance : ………………… Insured N° : ……………………… PHYSICIAN PHYSICIAN (NAME/First name - Street/N°- Town, ZIPCODE - Phone/FAX. IN UPPER CASES, PLEASE) COPY TO OTHER PHYSICIAN (NAME/First name - Street/N°- Town, ZIPCODE - Phone/FAX. IN UPPER CASES, PLEASE) « The laboratory is granted permission by the Physician/Patient to transmit copies of the report to other physicians» Opposition of the patient to the registration of this request results in the electronic patient record (DPI) of the HUG If the patient belongs to a family already known to the laboratory, please indicate index case NAME: CLINICAL INFORMATIONS given by the physician: Ethnic origins Father Mother Currently pregnant Date of last menses Number of weeks of amenorrhea SAMPLE(S) Most of our tests work from 4 ml of blood in EDTA (children <2 ans : 1 On every and single NAME First name ml : ok) or from purified DNA (some exceptions apply for some tests) tube. -

Hyperosmolar Hyperglycemic State (HHS) Erica Kretchman DO October 19 2018 Speaker for Valeritas, Medtronic, Astrazenica, Boehringer Ingelheim
Hyperosmolar Hyperglycemic State (HHS) Erica Kretchman DO October 19 2018 Speaker for Valeritas, Medtronic, AstraZenica, Boehringer Ingelheim. These do not influence this presentation Objective • Review and understand diagnosis of Hyperosmolar Hyperglycemic State (HHS) and differentiating from Diabetic Ketoacidosis • Treatment of HHS • Complications of HHS Question 1 • Which of the following is NOT a typical finding in HHS? 1. Blood PH <7.30 2. Dehydration 3. Mental Status Changes 4. Osmotic diuresis Question 2 • Hypertonic fluids, such as 3% saline, are the first line of treatment to correct dehydration in HHS 1. True 2. False Question 3 • Which of the following statements is INCORRECT about Hyperosmolar Hyperglycemic State? 1. HHS occurs mainly in type 2 diabetics. 2. This condition presents without ketones in the urine. 3. Metabolic alkalosis presents in severe HHS. 4. Intravenous Regular insulin is used to treat hyperglycemia. Hyperosmolar Hyperglycemic State (HHS) • HHS and DKA are of two of the most serious complications form Diabetes • Hospital admissions for HHS are lower than the rate for DKA and accounts for less than 1 percent of all primary diabetic admissions • Mortality rate for patients with HHS is between 10 and 20 percent, which is approximately 10 times higher than that for DKA • Declined between 1980 and 2009 • Typically from precipitating illness - rare from HHS itself PRECIPITATING FACTORS • The most common events are infection (often pneumonia or urinary tract infection) and discontinuation of or inadequate insulin -

Diabetes - High Blood Sugar After Hours Telephone Triage Protocols | Adult | 2019
Diabetes - High Blood Sugar After Hours Telephone Triage Protocols | Adult | 2019 DEFINITION ⦁ Patient with known diabetes mellitus ⦁ Has a high blood sugar (hyperglycemia), defined as a blood glucose > 200 mg/dL (11 mmol/L) ⦁ Has symptoms of high blood sugar ⦁ Has questions regarding high blood sugar SYMPTOMS of High Blood Sugar (Hyperglycemia) include: ⦁ Mild hyperglycemia: Most often patient will have no symptoms. ⦁ Moderate hyperglycemia: polyuria, polydipsia, fatigue, blurred vision. ⦁ Severe hyperglycemia: confusion and coma. ⦁ Diabetic ketoacidosis (DKA): fruity odor on breath, vomiting, rapid breathing, weakness, confusion, and coma. INITIAL ASSESSMENT QUESTIONS 1. BLOOD GLUCOSE: "What is your blood glucose level?" 2. ONSET: "When did you check the blood glucose?" 3. USUAL RANGE: "What is your glucose level usually?" (e.g., usual fasting morning value, usual evening value) 4. KETONES: "Do you check for ketones (urine or blood test strips)?" If yes, ask: "What does the test show now?" 5. TYPE 1 or 2: "Do you know what type of diabetes you have?" (e.g., Type 1, Type 2, Gestational; doesn't know) 6. INSULIN: "Do you take insulin?" "What type of insulin(s) do you use? What is the mode of delivery? (syringe, pen (e.g., injection or pump) 7. DIABETES PILLS: "Do you take any pills for your diabetes?" If yes, ask: "Have you missed taking any pills recently?" 8. OTHER SYMPTOMS: "Do you have any symptoms?" (e.g., fever, frequent urination, difficulty breathing, dizziness, weakness, vomiting) 9. PREGNANCY: "Is there any chance you are pregnant?" -

Clinical Practice Guideline for Diagnosis, Treatment and Follow-Up of Diabetes Mellitus and Its Complications - 2019
THE SOCIETY of ENDOCRINOLOGY and METABOLISM of TURKEY (SEMT) Clinical Practice Guideline for Diagnosis, Treatment and Follow-up of Diabetes Mellitus and Its Complications - 2019 English Version of the 12th Edition SEMT Diabetes Mellitus Working Group ISBN: 978-605-4011-39-1 CLINICAL PRACTICE GUIDELINE FOR DIAGNOSIS, TREATMENT, AND FOLLOW-UP OF DIABETES MELLITUS AND ITS COMPLICATIONS-2019 © SEMT -2019 This material has been published and distributed by The Society of Endocrinology and Metabolism of Turkey (SEMT). Whole or part of this guideline cannot be reproduced or used for commercial purposes without permission. THE SOCIETY of ENDOCRINOLOGY and METABOLISM of TURKEY (SEMT) Meşrutiyet Cad., Ali Bey Apt. 29/12, Kızılay 06420, Ankara, Turkey Phone. +90 312 425 2072 http://www.temd.org.tr ISBN: 978-605-4011-39-1 English Version of the 12th Edition Publishing Services BAYT Bilimsel Araştırmalar Basın Yayın ve Tanıtım Ltd. Şti. Ziya Gökalp Cad. 30/31 Kızılay 06420, Ankara, Turkey Phone. +90 312 431 3062 Fax +90 312 431 3602 www.bayt.com.tr Printing Miki Matbaacılık San. ve Tic. Ltd. Şti. Matbaacılar Sanayi Sitesi 1516/1 Sk. No. 27 İvedik, Yenimahalle / Ankara, Turkey Phone. +90 312 395 2128 Print Date: October 23, 2019 “Major achievements and important undertakings are only possible through collaborations” “Büyük işler, mühim teşebbüsler; ancak, müşterek mesai ile kabil-i temindir.” MUSTAFA KEMAL ATATÜRK, 1925 PREFACE Dear colleagues, The prevalence of diabetes has been increasing tremendously in the last few decades. As a result , medical professionals/ specialists from different fields encounter many diabetics in their daily practice. At this point, updated guidelines on diabetes management, which take regional specification into consideration is needed. -

Jeffrey Kleinberger Ph.D. Candidate Molecular Medicine Program, Genome Biology Track Graduate Program in Life Sciences, University of Maryland, Baltimore
Discovery and Analysis of Patients with Monogenic Diabetes in Multiple Cohorts to Guide Future Diagnosis Item Type dissertation Authors Kleinberger, Jeffrey Publication Date 2017 Abstract Monogenic diabetes is hyperglycemia caused by a variant in a single gene, and it accounts for approximately 1-2% of all diabetes cases. A genetic diagnosis of monogenic diabetes is important because the most common gene etiologies can be effectively ... Keywords MODY; monogenic diabetes; screening; Clinical Trial; Diabetes Mellitus, Type 2; Zebrafish Download date 05/10/2021 09:00:42 Link to Item http://hdl.handle.net/10713/7072 Jeffrey Kleinberger Ph.D. Candidate Molecular Medicine Program, Genome Biology Track Graduate Program in Life Sciences, University of Maryland, Baltimore Contact Information Medical School Teaching Facility 357 685 West Baltimore St. Baltimore, MD 21201 [email protected] Education Juniata College Huntingdon, PA August 2004 – May 2008 Cum Laude distinction (GPA: 3.701) Biochemistry major Coursework included: Organic Chemistry, Bioinorganic Chemistry, Analytical Chemistry, Physical Chemistry, Chemistry Research, Biology, Cell Biology, Genetics, Biostatistics, Molecular Techniques, Physiology, Microbiology, Biochemistry and Molecular Biology (I-III), Calculus (I&II), Physics (I&II), Scientific Glassblowing, College Writing Seminar, Art of Public Speaking, Intro to Psychology, Learning & Conditioning, Mod. Knowledge & The Self, United States to 1877, The American Revolution, Survey of Western Art, Modern Architecture, -

一般演題(口演)/Oral Sessions
一般演題(口演)!Oral Sessions ご ! 案 第 60 回大会賞候補セッション(口演) Oral Presentation Award Session 内 日 時:10 月 16 日(金)11:25~12:20 第 2 会場(南館 4 階 錦) 座 長:稲澤 譲治(東京医科歯科大学難治疾患研究所ゲノム応用医学研究部門(分子細胞遺伝)) 田中 敏博(東京医科歯科大学疾患バイオリソースセンター) Date:Oct. 16 (Fri.) 11:25~12:20 Room 2(Nishiki, South Tower 4F) Chairs:Johji Inazawa(Tokyo Medical and Dental University) Toshihiro Tanaka(Tokyo Medical and Dental University) プ ロ BO-1 ゲノムワイド関連解析(GWAS)データを活用した in silico 解析による新規抗パーキンソン病薬 グ の探索 ラ In silico drug discovery for Parkinson’s disease by using genome!wide association study ム (GWAS)data ○上中 健 1(Takeshi Uenaka)、佐竹 渉 1(Wataru Satake)、謝 珮琴 1(Pei"Chieng Cha)、 岡田 随象 2(Yukinori Okada)、戸田 達史 1(Tatsushi Toda) 1 神戸大学大学院医学研究科神経内科!分子脳科学 指 (Division of Neurology, Kobe University Graduate School of Medicine, Kobe, Japan) 定 2 東京医科歯科大学大学院医歯学総合研究科疾患多様性遺伝学分野 演 (Department of Human Genetics and Disease Diversity, Graduate School of Medical and Dental Sciences, 題 Tokyo Medical and Dental University, Tokyo, Japan) 抄 録 BO-2 MIRAGE 症候群:機能亢進型 SAMD9 変異を原因とする新規症候群の発見 MIRAGE syndrome:New genetic syndrome caused by activating SAMD9 mutations ○鳴海 覚志 1(Satoshi Narumi)、天野 直子 1(Naoko Amano)、石井 智弘 1(Tomohiro Ishii)、 一 勝又 規行 2(Noriyuki Katsumata)、福澤 龍二 3(Ryuji Fukuzawa)、芝田 晋介 4(Shinsuke Shibata)、 般 4 5 6 演 岡野 栄之 (Hideyuki Okano)、清水 厚志 (Atsushi Shimizu)、三宅 紀子 (Noriko Miyake)、 題 松本 直通 6(Naomichi Matsumoto)、長谷川 奉延 1(Tomonobu Hasegawa) ( 1 慶應義塾大学医学部小児科 口 (Department of Pediatrics, Keio University School of Medicine, Tokyo, Japan) 演 ) 2 国立成育医療研究センター研究所分子内分泌研究部 抄 (Department of Molecular Endocrinology, National Research -

Type 2 Diabetes Mellitus in Children and Adolescents
CLINICAL Type 2 diabetes mellitus in children and adolescents Kung-Ting Kao, Matthew A Sabin Background ype 2 diabetes mellitus (T2DM), and obesity. Furthermore, treatment previously known as non-insulin options are limited by the lack of licenced The incidence of type 2 diabetes mellitus T dependent diabetes or adult- treatment modalities in the paediatric (T2DM) in children and adolescents is onset diabetes, is a disorder arising from population, and adherence, psychosocial increasing, mirroring the epidemic of insulin resistance and relative (rather than health and wellbeing are often poor.7 paediatric obesity. Early-onset T2DM is absolute) insulin deficiency in the absence Early-onset T2DM is associated with associated with poor long-term outcomes. of autoimmune beta-cell destruction.1 It is significant long-term morbidity and Objectives a polygenic disorder involving interactions mortality. Adolescents diagnosed with between genetic and environmental T2DM are predicted to lose 15 years from In this article, we describe the growing risk factors that result in the underlying their remaining life expectancy when problem of early-onset T2DM in Australia, pathophysiology of hepatic and muscle compared with their peers who do not explore the difference between early- insulin resistance, and subsequent beta-cell have T2DM.8 Complications of diabetes onset and adult-onset T2DM, and review failure.2 Most patients with this disorder are also common and present even earlier the management of T2DM in children and are obese, and T2DM often remains than in adolescents with type 1 diabetes adolescents. undiagnosed for many years while the mellitus (T1DM).9,10 A long-term study patient progresses symptom-free through in Japan found that over a period of 20 Discussion the earlier stages of hyperglycaemia known years, 24% of the 1063 participants were 11 T2DM is difficult to differentiate from the as ‘pre-diabetes’. -
Copyrighted Material
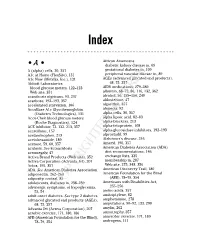
34_568205 bindex.qxd 5/28/04 11:03 AM Page 365 Index African Americans • A • diabetic kidney disease in, 69 A (alpha) cells, 30, 357 gestational diabetes in, 109 A1c at Home (FlexSite), 131 peripheral vascular disease in, 89 A1c Now (Metrika, Inc.), 131 AGEs (advanced glycated end products), Abbott Laboratories 68, 75, 357 blood glucose meters, 122–123 AIDS medications, 279–280 Web site, 351 albumin, 68–72, 86, 116, 132, 362 acanthosis nigricans, 93, 237 alcohol, 56, 155–156, 240 acarbose, 192–193, 357 aldosterone, 47 accelerated starvation, 106 algorithm, 357 AccuBase A1c Glycohemoglobin alopecia, 92 (Diabetes Technologies), 131 alpha cells, 30, 357 Accu-Chek blood glucose meters alpha lipoic acid, 82–83 (Roche Diagnostics), 124 alpha-blockers, 213 ACE inhibitor, 72, 132, 213, 357 alpha-fetoprotein, 108 acesulfame, 157 alpha-glucosidase inhibitors, 192–193 acetaminophen, 213 alprostadil, 99 acetohexamide, 189 Alzheimer’s disease, 246 acetone, 59, 60, 357 Amaryl, 190, 357 acidosis. See ketoacidosis American Diabetes Association (ADA) acromegaly, 47 diet recommendations, 146 Activa Brand Products (Web site), 352 exchange lists, 335 Activa Corporation (Advanta Jet), 207 membership in, 287 Actos, 195, 357 Web site, 275, 348, 356 ADA. See American Diabetes Association American Discovery Trail, 180 adiponectin, 262–263 American Foundation for the Blind adiposity, central, 85 (AFB), 78–79, 354 adolescents, diabetes in, 238–239 Americans with Disabilities Act, adrenergic symptoms,COPYRIGHTED of hypoglycemia, 255–256 MATERIAL 53, 54 amino acids, -

Hyperosmolar Hyperglycemic State (HHS) Is the Most Serious Acute Hypergly- Cemic Emergency in Patients with Type 2 Diabetes
3124 Diabetes Care Volume 37, November 2014 Francisco J. Pasquel and Hyperosmolar Hyperglycemic Guillermo E. Umpierrez State: A Historic Review of the Clinical Presentation, Diagnosis, and Treatment Diabetes Care 2014;37:3124–3131 | DOI: 10.2337/dc14-0984 The hyperosmolar hyperglycemic state (HHS) is the most serious acute hypergly- cemic emergency in patients with type 2 diabetes. von Frerichs and Dreschfeld described the first cases of HHS in the 1880s in patients with an “unusual diabetic coma” characterized by severe hyperglycemia and glycosuria in the absence of Kussmaul breathing, with a fruity breath odor or positive acetone test in the urine. Current diagnostic HHS criteria include a plasma glucose level >600 mg/dL and increased effective plasma osmolality >320 mOsm/kg in the absence of ketoacidosis. The incidence of HHS is estimated to be <1% of hospital admissions of patients with diabetes. The reported mortality is between 10 and 20%, which is about 10 times higher than the mortality rate in patients with diabetic ketoacidosis (DKA). Despite the severity of this condition, no prospective, randomized studies have determined best REVIEW treatment strategies in patients with HHS, and its management has largely been extrapolated from studies of patients with DKA. There are many unresolved questions that need to be addressed in prospective clinical trials regarding the pathogenesis and treatment of pediatric and adult patients with HHS. The hyperosmolar hyperglycemic state (HHS) is a syndrome characterized by severe hyperglycemia, hyperosmolality, and dehydration in the absence of ketoacidosis. The exact incidence of HHS is not known, but it is estimated to account for ,1% of hospital admissions in patients with diabetes (1). -

Assessing Blood Glucose Regulation
Functional Medicine University’s Functional Diagnostic Medicine Training Program Mod 4 * FDMT533B Primary and Advanced Testing: Assessing Blood Glucose Regulation By Wayne L. Sodano, D.C., D.A.B.C.I., & Ron Grisanti, D.C., D.A.B.C.O., M.S. http://www.FunctionalMedicineUniversity.com Limits of Liability & Disclaimer of Warranty We have designed this book to provide information in regard to the subject matter covered. It is made available with the understanding that the authors are not liable for the misconceptions or misuse of information provided. The purpose of this book is to educate. It is not meant to be a comprehensive source for the topic covered, and is not intended as a substitute for medical diagnosis or treatment, or intended as a substitute for medical counseling. Information contained in this book should not be construed as a claim or representation that any treatment, process or interpretation mentioned constitutes a cure, palliative, or ameliorative. The information covered is intended to supplement the practitioner’s knowledge of their patient. It should be considered as adjunctive and support to other diagnostic medical procedures. This material contains elements protected under International and Federal Copyright laws and treaties. Any unauthorized reprint or use of this material is prohibited. Functional Medicine University; Functional Diagnostic Medicine Training Program/Insider’s Guide Module 4: FDMT 533B: Primary and Advanced Testing: Assessing Blood Glucose Regulation Copyright © 2010 Functional Medicine University, All Rights Reserved Functional Medicine University’s Functional Diagnostic Medicine Training Program Module 4: FDMT 533B: Primary and Advanced Testing: Assessing Blood Glucose Regulation By Wayne L. -

Hyperglycemia – Prediabetes
North Dakota Family Planning Program Clinical Protocol Manual Health Maintenance – HM 8 Hyperglycemia – Prediabetes DEFINITION Hyperglycemia is an excess of glucose in the blood. Prediabetes is a condition when blood glucose levels are higher than normal but not yet high enough to be diagnosed as diabetes. (Prediabetes is also known as Impaired Glucose Tolerance (IGT) or Impaired Fasting Glucose (IFG) depending on which test was used to detect it. IGT uses the oral glucose tolerance test and IFG uses the fasting plasma glucose test.) SUBJECTIVE May include: 1. No symptoms 2. Family history of diabetes 3. Weight changes 4. Fatigue, blurred vision, recurrent vulvovaginal candidiasis 5. History of gestational diabetes or birth weight of newborn 9 lbs. or greater 6. Polydipsia, polyphagia, or polyuria 7. 20% over ideal body weight; sedentary lifestyle 8. Decreased wound healing 9. Race (higher incidence of diabetes among American Indian, Hispanic, and African American population) 10. History of hypertension 11. History of decreased HDL and increased triglycerides 12. History of Polycystic Ovarian Syndrome or Metabolic Syndrome 13. History of antipsychotic medication therapy OBJECTIVE May include: 1. Blood pressure 2. Height and weight 3. Complete physical exam. Acanthosis Nigricans may be noted in axillae, groin, and/or neck LABORATORY May refer for: 1. Hyperglycemia a. lab of choice may include one or more of the following: i. Fasting plasma glucose (FPG) a) Prediabetes: FPG between 100 mg/dl to 125 mg/dl b) Diabetes: FPG is > 126 mg/dl ii. Oral Glucose Tolerance Test (OGTT) a) Prediabetes: OGTT 140mg/dl to 199 mg/dl b) Diabetes: OGTT 200mg/dl or higher iii.