Type 2 Diabetes Mellitus in Children and Adolescents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hyperosmolar Hyperglycemic State (HHS) Erica Kretchman DO October 19 2018 Speaker for Valeritas, Medtronic, Astrazenica, Boehringer Ingelheim
Hyperosmolar Hyperglycemic State (HHS) Erica Kretchman DO October 19 2018 Speaker for Valeritas, Medtronic, AstraZenica, Boehringer Ingelheim. These do not influence this presentation Objective • Review and understand diagnosis of Hyperosmolar Hyperglycemic State (HHS) and differentiating from Diabetic Ketoacidosis • Treatment of HHS • Complications of HHS Question 1 • Which of the following is NOT a typical finding in HHS? 1. Blood PH <7.30 2. Dehydration 3. Mental Status Changes 4. Osmotic diuresis Question 2 • Hypertonic fluids, such as 3% saline, are the first line of treatment to correct dehydration in HHS 1. True 2. False Question 3 • Which of the following statements is INCORRECT about Hyperosmolar Hyperglycemic State? 1. HHS occurs mainly in type 2 diabetics. 2. This condition presents without ketones in the urine. 3. Metabolic alkalosis presents in severe HHS. 4. Intravenous Regular insulin is used to treat hyperglycemia. Hyperosmolar Hyperglycemic State (HHS) • HHS and DKA are of two of the most serious complications form Diabetes • Hospital admissions for HHS are lower than the rate for DKA and accounts for less than 1 percent of all primary diabetic admissions • Mortality rate for patients with HHS is between 10 and 20 percent, which is approximately 10 times higher than that for DKA • Declined between 1980 and 2009 • Typically from precipitating illness - rare from HHS itself PRECIPITATING FACTORS • The most common events are infection (often pneumonia or urinary tract infection) and discontinuation of or inadequate insulin -
Copyrighted Material
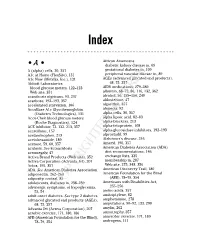
34_568205 bindex.qxd 5/28/04 11:03 AM Page 365 Index African Americans • A • diabetic kidney disease in, 69 A (alpha) cells, 30, 357 gestational diabetes in, 109 A1c at Home (FlexSite), 131 peripheral vascular disease in, 89 A1c Now (Metrika, Inc.), 131 AGEs (advanced glycated end products), Abbott Laboratories 68, 75, 357 blood glucose meters, 122–123 AIDS medications, 279–280 Web site, 351 albumin, 68–72, 86, 116, 132, 362 acanthosis nigricans, 93, 237 alcohol, 56, 155–156, 240 acarbose, 192–193, 357 aldosterone, 47 accelerated starvation, 106 algorithm, 357 AccuBase A1c Glycohemoglobin alopecia, 92 (Diabetes Technologies), 131 alpha cells, 30, 357 Accu-Chek blood glucose meters alpha lipoic acid, 82–83 (Roche Diagnostics), 124 alpha-blockers, 213 ACE inhibitor, 72, 132, 213, 357 alpha-fetoprotein, 108 acesulfame, 157 alpha-glucosidase inhibitors, 192–193 acetaminophen, 213 alprostadil, 99 acetohexamide, 189 Alzheimer’s disease, 246 acetone, 59, 60, 357 Amaryl, 190, 357 acidosis. See ketoacidosis American Diabetes Association (ADA) acromegaly, 47 diet recommendations, 146 Activa Brand Products (Web site), 352 exchange lists, 335 Activa Corporation (Advanta Jet), 207 membership in, 287 Actos, 195, 357 Web site, 275, 348, 356 ADA. See American Diabetes Association American Discovery Trail, 180 adiponectin, 262–263 American Foundation for the Blind adiposity, central, 85 (AFB), 78–79, 354 adolescents, diabetes in, 238–239 Americans with Disabilities Act, adrenergic symptoms,COPYRIGHTED of hypoglycemia, 255–256 MATERIAL 53, 54 amino acids, -

Hyperosmolar Hyperglycemic State (HHS) Is the Most Serious Acute Hypergly- Cemic Emergency in Patients with Type 2 Diabetes
3124 Diabetes Care Volume 37, November 2014 Francisco J. Pasquel and Hyperosmolar Hyperglycemic Guillermo E. Umpierrez State: A Historic Review of the Clinical Presentation, Diagnosis, and Treatment Diabetes Care 2014;37:3124–3131 | DOI: 10.2337/dc14-0984 The hyperosmolar hyperglycemic state (HHS) is the most serious acute hypergly- cemic emergency in patients with type 2 diabetes. von Frerichs and Dreschfeld described the first cases of HHS in the 1880s in patients with an “unusual diabetic coma” characterized by severe hyperglycemia and glycosuria in the absence of Kussmaul breathing, with a fruity breath odor or positive acetone test in the urine. Current diagnostic HHS criteria include a plasma glucose level >600 mg/dL and increased effective plasma osmolality >320 mOsm/kg in the absence of ketoacidosis. The incidence of HHS is estimated to be <1% of hospital admissions of patients with diabetes. The reported mortality is between 10 and 20%, which is about 10 times higher than the mortality rate in patients with diabetic ketoacidosis (DKA). Despite the severity of this condition, no prospective, randomized studies have determined best REVIEW treatment strategies in patients with HHS, and its management has largely been extrapolated from studies of patients with DKA. There are many unresolved questions that need to be addressed in prospective clinical trials regarding the pathogenesis and treatment of pediatric and adult patients with HHS. The hyperosmolar hyperglycemic state (HHS) is a syndrome characterized by severe hyperglycemia, hyperosmolality, and dehydration in the absence of ketoacidosis. The exact incidence of HHS is not known, but it is estimated to account for ,1% of hospital admissions in patients with diabetes (1). -

ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic Ketoacidosis and the Hyperglycem
Received: 11 April 2018 Accepted: 31 May 2018 DOI: 10.1111/pedi.12701 ISPAD CLINICAL PRACTICE CONSENSUS GUIDELINES ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic ketoacidosis and the hyperglycemic hyperosmolar state Joseph I. Wolfsdorf1 | Nicole Glaser2 | Michael Agus1,3 | Maria Fritsch4 | Ragnar Hanas5 | Arleta Rewers6 | Mark A. Sperling7 | Ethel Codner8 1Division of Endocrinology, Boston Children's Hospital, Boston, Massachusetts 2Department of Pediatrics, Section of Endocrinology, University of California, Davis School of Medicine, Sacramento, California 3Division of Critical Care Medicine, Boston Children's Hospital, Boston, Massachusetts 4Department of Pediatric and Adolescent Medicine, Medical University of Vienna, Vienna, Austria 5Department of Pediatrics, NU Hospital Group, Uddevalla and Sahlgrenska Academy, Gothenburg University, Uddevalla, Sweden 6Department of Pediatrics, School of Medicine, University of Colorado, Aurora, Colorado 7Division of Endocrinology, Diabetes and Metabolism, Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, New York 8Institute of Maternal and Child Research, School of Medicine, University of Chile, Santiago, Chile Correspondence Joseph I. Wolfsdorf, Division of Endocrinology, Boston Children's Hospital, 300 Longwood Avenue, Boston, MA. Email: [email protected] 1 | SUMMARY OF WHAT IS Risk factors for DKA in newly diagnosed patients include younger NEW/DIFFERENT age, delayed diagnosis, lower socioeconomic status, and residence in a country with a low prevalence of type 1 diabetes mellitus (T1DM). Recommendations concerning fluid management have been modified Risk factors for DKA in patients with known diabetes include to reflect recent findings from a randomized controlled clinical trial omission of insulin for various reasons, limited access to medical ser- showing no difference in cerebral injury in patients rehydrated at dif- vices, and unrecognized interruption of insulin delivery in patients ferent rates with either 0.45% or 0.9% saline. -
Perioperative Glycaemic Control for Preterm Infant with Transient
Rattana‑arpa et al. BMC Res Notes (2016) 9:140 DOI 10.1186/s13104-016-1957-y BMC Research Notes CASE REPORT Open Access Perioperative glycaemic control for preterm infant with transient neonatal hyperglycaemia and gastroschisis Sirirat Rattana‑arpa, Saowaphak Lapmahapaisan and Arunotai Siriussawakul* Abstract Background: Neonatal hyperglycaemia is a rare metabolic disorder. There are no reports of an association between neonatal hyperglycaemia and gastroschisis. Case presentation: This report presents preoperative and intraoperative management of blood sugar in a low birth weight Thai preterm neonate with gastroschisis and a diagnosis of neonatal hyperglycaemia. The patient underwent an emergency, multi-staged, surgical repair under general anaesthesia. Conclusion: Anaesthesiologists should be aware of possible perioperative dysglycaemic conditions in these patients. Proper timing of surgery and appropriate preanaesthetic preparation are necessary to reduce the morbidity and mor‑ tality related to hyperglycaemia and gastroschisis. Consent: The patient’s guardian has given consent for the case report to be published. Keywords: Abdominal wall defect, High blood sugar, Prematurity Background fluid loss and infection [3]. Nevertheless, the timing of Dysglycaemia frequently occurs in very low birth weight the surgical correction of the gastroschisis in this par- preterm infants. Deficiency of glycogen stores at birth ticular case was somewhat controversial. This report and defective counter-regulatory hormone responses are demonstrates the challenge of decision-making by a mul- common in prematurity, making hypoglycaemia a more tidisciplinary team that analysed the risks and benefits of frequent occurrence than hyperglycaemia [1]. The inci- promptly going to surgery versus waiting to optimize the dence of neonatal hyperglycaemia has not been clearly patient’s condition. -

Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar Syndrome
In Brief Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic syndrome (HHS) are two acute complications of diabetes that can result in increased morbidity and mortality if not efficiently and effectively treated. Mortality rates are 2–5% for DKA and 15% for HHS, and mortality is usually a conse- quence of the underlying precipitating cause(s) rather than a result of the metabolic changes of hyperglycemia. Effective standardized treatment proto- cols, as well as prompt identification and treatment of the precipitating cause, are important factors affecting outcome. Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar Syndrome The two most common life-threaten- having type 2 diabetes because 29% ing complications of diabetes mellitus of patients were obese, had measur- include diabetic ketoacidosis (DKA) able insulin secretion, and had a low Guillermo E. Umpierrez, MD, FACP; and hyperglycemic hyperosmolar syn- prevalence of autoimmune markers of Mary Beth Murphy, RN, MS, CDE, drome (HHS). Although there are -cell destruction.4 MBA; and Abbas E. Kitabchi, PhD, important differences in their patho- Treatment of patients with DKA MD, FACP, FACE genesis, the basic underlying mecha- and HHS utilizes significant health nism for both disorders is a reduction care resources. Recently, it was esti- in the net effective concentration of mated that treatment of DKA episodes circulating insulin coupled with a accounts for more than one of every concomitant elevation of counterreg- four health care dollars spent on direct ulatory hormones (glucagon, cate- medical care for adults with type 1 cholamines, cortisol, and growth hor- diabetes, and for one of every two dol- mone). lars for those patients experiencing These hyperglycemic emergencies multiple episodes of DKA.5 continue to be important causes of Despite major advances in their morbidity and mortality among management, recent series have patients with diabetes. -

Perioperative Management of Diabetes Mellitus: a Review
Perioperative management of Diabetes Mellitus: A review. Dissertação de Mestrado Integrado em Medicina Instituto de Ciências Biomédicas Abel Salazar, Universidade do Porto Junho de 2019 Autora: Mariana Raquel Moreira Azevedo Estudante do 6º ano do Mestrado Integrado em Medicina, Instituto de Ciências Biomédicas Abel Salazar, Universidade do Porto; Número de aluna: 201303092; Endereço eletrónico: [email protected]. Orientador: Prof. Doutor Humberto José da Silva Machado Assistente Hospitalar Graduado Sénior de Anestesiologia do CHUP; Diretor do Serviço de Anestesiologia do CHUP; Adjunto da Direção Clínica do CHUP; Professor Associado Convidado do ICBAS; Endereço eletrónico: [email protected]. ABSTRACT Introduction: Diabetes Mellitus is frequently observed in surgical patients and relates to an increase in perioperative morbidity and mortality. Disease, anesthesia and surgery result in dysglycemia (hypo and/or hyperglycemia), which is one of the worse prognostic factors. The objective of this work is to review the specific needs of the diabetic surgical patient in the perioperative period, gathering the latest information regarding its optimization. Materials and Methods: This dissertation was elaborated from scientific articles obtained through PubMed, Google Scholar and Google, published between 2008 and 2018 and written in English or Portuguese. In the end, eighty-nine articles were used. Results: Some measures have been proposed in order to reduce perioperative complications in the diabetic. Preoperative period: an -

Hyperglycaemic Hyperosmolar State in an Obese Prepubertal Girl with Type
Mohn et al. Italian Journal of Pediatrics (2021) 47:38 https://doi.org/10.1186/s13052-021-00983-z CASE REPORT Open Access Hyperglycaemic hyperosmolar state in an obese prepubertal girl with type 2 diabetes: case report and critical approach to diagnosis and therapy Angelika Mohn* , Nella Polidori, Valeria Castorani, Laura Comegna, Cosimo Giannini, Francesco Chiarelli and Annalisa Blasetti Abstract Introduction: Isolated Hyperosmolar Hyperglycaemic Syndrome (HHS) is a life-threatening condition characterized by elevated serum glucose concentrations and hyperosmolality without significant ketosis. It is often described in obese adults with unknown Type 2 Diabetes (T2D), rarely in youth. In childhood the most common cause of metabolic glucose related derangement is Diabetic Ketoacidosis (DKA) in Type 1 Diabetes (T1D). Interestingly, both components can be combined with each other, thus the prevalent condition needs to be recognised implying a different therapeutic approach. Case presentation: In this case, we report a prepubertal Caucasian obese girl admitted for two episodes of combined HHS/DKA in order to elucidate her clinical course taking into account the current pediatric recommendations based on adult guidelines for HHS. Conclusions: The treatment of HHS and even more of HHS/DKA in youth is still controversial as no specific guidelines for children are available especially during the prepubertal age. The description of our case might be helpful and offer relevant points for future consensus. Keywords: Hyperglycaemic hyperosmolar state, Obese children, Type 2 Diabetes, Diabetic Ketoacidosis, Case Report Introduction complications associated with HHS, it is imperative to Recent trends indicate a rising in the incidence of Type distinguish HHS from the most common Diabetic 2 Diabetes (T2D) in children, with a significant increase Ketoacidosis (DKA) in childhood since erroneous clin- in morbidity and its related complications [1–3]. -

CLASSIFICATION of DIABETES MELLITUS 2019 Classification of Diabetes Mellitus ISBN 978-92-4-151570-2
CLASSIFICATION OF DIABETES MELLITUS 2019 Classification of diabetes mellitus ISBN 978-92-4-151570-2 © World Health Organization 2019 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. Classification of diabetes mellitus. Geneva: World Health Organization; 2019. Licence:CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. To submit requests for commercial use and queries on rights and licensing, see http://www.who.int/about/licensing. -

COVID-19 and Diabetic Ketoacidosis: Report of Eight Cases
Open Access Original Article DOI: 10.7759/cureus.14223 COVID-19 and Diabetic Ketoacidosis: Report of Eight Cases Balraj Singh 1 , Prem Patel 2 , Parminder Kaur 2 , Nicole Majachani 3 , Michael Maroules 4 1. Hematology/Oncology, Saint Joseph's University Medical Center, Paterson, USA 2. Cardiology, Saint Joseph's University Medical Center, Paterson, USA 3. Internal Medicine, Saint Joseph's University Medical Center, Paterson, USA 4. Hematology and Oncology, Saint Joseph's University Medical Center, Paterson, USA Corresponding author: Balraj Singh, [email protected] Abstract Aim To describe the clinical characteristics and outcome of hospitalized COVID-19 patients with diabetic ketoacidosis (DKA). Methods We report eight cases of diabetic ketoacidosis in COVID-19 who presented to our institution in New Jersey, USA. COVID-19 was diagnosed by nasopharyngeal swab reverse transcription polymerase chain reaction (RT- PCR). The patients' electronic medical records were reviewed. Data on patients' age, sex, ethnicity, laboratory values, glycosylated hemoglobin level, oral antihyperglycemic agents (OHAs), insulin, and clinical outcomes were collected. Results The median age of the patient was 42.5 years, and seven were males and one was female. Out of eight patients, five had type 2 diabetes mellitus (DM), two had undiagnosed DM, and one had type 1 DM. Median value of initial glucose on presentation was 454 mg/dL. Median value of HbA1c on presentation was 11.4% and of anion gap was 26.5 mEq/L. Four patients had large ketonemia, one patient had moderate ketonemia, and three patients had small ketonemia. All the patients were started on standard treatment protocol for DKA with intravenous fluids and IV insulin infusion. -

Kuldeep Et Al. International Journal of Innovative Science and Technology ISSN: 2455 - 9946
Kuldeep et al. International Journal of Innovative Science and Technology ISSN: 2455 - 9946 Recent classification of diabetes mellitus Available online at www.ijistweb.com RESEARCH ARTICLE Kuldeep Tiwari, Dinesh Kumar Sri Satya Sai University of Technology & Medical Sciences, Sehore-466001 *Corresponding Author’s E-mail: [email protected] ABSTRACT The right classification for diabetes mellitus (DM) allows a more adequate treatment and comprises four categories: type 1 DM, type 2 DM, other types, and gestational diabetes. Assigning a type of diabetes to an individual often depends on the circumstances present at the time of diagnosis, and many diabetic individuals do not easily fit into a single class. Diabetes mellitus and lesser forms of glucose intolerance, particularly impaired glucose tolerance, can now be found in almost every population in the world and epidemiological evidence suggests that, without effective prevention and control programmes, diabetes will likely continue to increase globally. These findings were confirmed in a similar study in India, in which the FPG and 2-h PG were each strongly and equally associated with retinopathy. For both the FPG and the 2-h PG, the prevalence of retinopathy was markedly higher above the point of intersection of the two components of the bimodal frequency distribution (FPG = 129 mg/dl [7.2 mmol/l] and 2- h PG = 207 mg/dl [11.5 mmol/l]). In the NHANES III, 2,821 individuals aged 40-74 years received an OGTT, a measurement of HbAlc, and an assessment of retinopathy by fundus photography. Keywords: diabetes mellitus, diagnosis, retinopathy 1. Introduction Diabetes mellitus (DM) is a group of be present for a long time before the diagnosis diseases characterized by high levels of blood is made (4). -

Perioperative Management of Diabetes
a & hesi C st lin e ic n a Azevedo and Machado, J Anesth Clin Res 2019, A l f R o e Journal of Anesthesia & Clinical 10:5 l s e a a n r r c u h o J Research ISSN: 2155-6148 Review Article Open Access Perioperative Management of Diabetes Mellitus: A Review Mariana Raquel Moreira Azevedo1 and Humberto S Machado2,3* 1Department of Anesthesiology, Abel Salazar Institute of Biomedical Sciences, University of Porto, Portugal 2Department of Anesthesiology, University Hospital Center of Porto, Porto, Portugal 3Center for Clinical Research in Anesthesiology, University Hospital Center of Porto, Porto, Portugal *Corresponding author: Dr Humberto S Machado, Department of Anesthesiology, University Hospital Center of Porto, Portugal Largo Professor Abel Salazar, 4099-001 Porto, Portugal, Tel: +351.935848475; E-mail: [email protected] Received date: April 19, 2019; Accepted date: May 24, 2019; Published date: May 31, 2019 Copyright: © 2019 Azevedo MRM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Introduction: Diabetes Mellitus (DM) is frequently observed in surgical patients and relates to an increase in perioperative morbidity and mortality. Disease, anesthesia and surgery result in dysglycemia (hypo and/or hyperglycemia), which is one of the worse prognostic factors. The objective of this study is to review the specific needs of the diabetic surgical patient in the perioperative period, regarding its optimization. Methods: Scientific studies (n=89) were obtained through PubMed, Google Scholar and Google, between 2008 and 2018.