Hyperglycemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diabetes Control in Thyroid Disease
In Brief Thyroid disease is commonly found in most types of diabetes. This article defines the prevalence of thyroid disease in diabetes and elucidates through case studies the assessment, diagnosis, and clinical management of thyroid disease in diabetes. Diabetes Control in Thyroid Disease Thyroid disease is a pathological state abnormality. Several studies, including that can adversely affect diabetes con- the Colorado study, have documented trol and has the potential to negative- a higher prevalence of thyroid disease Jennal L. Johnson, MS, RNC, FNP, ly affect patient outcomes. Thyroid in women, with prevalence rates rang- BC-ADM, CDE disease is found commonly in most ing from 4 to 21%, whereas the rate in forms of diabetes and is associated men ranges from 2.8 to 16%.1 with advanced age, particularly in Thyroid disease increases with age. In type 2 diabetes and underlying the Colorado study, the 18-year-olds autoimmune disease in type 1 dia- had a prevalence rate of 3.5% com- betes. This article defines the preva- pared with a rate of 18.5% for those lence of thyroid disease in diabetes, ≥ 65 years of age. discusses normal physiology and The prevalence of thyroid disease in screening recommendations for thy- diabetes has been estimated at 10.8%,2 roid disease, and elucidates through with the majority of cases occurring as case studies the assessment, diagnosis, hypothyroidism (~ 30%) and subclini- and clinical management of thyroid cal hypothyroidism (~ 50%).2 Hyper- disease and its impact on diabetes. thyroidism accounts for 12%, and postpartum thyroiditis accounts for Thyroid Disease Prevalence 11%.2 Of the female patients with The prevalence of thyroid disease in type 1 diabetes, 30% have thyroid dis- the general population is estimated to ease, with a rate of postpartum thy- be 6.6%, with hypothyroidism the roid disease three times that of the most common malady.1 Participants normal population. -

Refractory Hypoglycemia in T-Cell Lymphoma
Open Access Austin Oncology Case Reports Case Report Refractory Hypoglycemia in T-Cell Lymphoma Buyukaydina B1*, Tunca M1, Alayb M2, Kazanciogluc R3 and Reha E3 Abstract 1Bezmialem Vakif University, Department of Internal Hypoglycemia is commonly seen in diabetes mellitus patients; whereas it Medicine, Turkey is rarely seen in a healthy person. In this case, we reported a male patient 2Yuzuncu Yil University, Department of Endocrinology, with a treatment-resistant hypoglycemia. A 53 years old male patient admitted Turkey to our clinic with debility, nausea and vomiting. Physical examination revealed 3Bezmialem Vakif University, Department of Nephology, lymphadenopathies in the left axilla and inguinal regions; and presence of right Turkey upper quadrant tenderness. Biochemical results revealed severe hypoglycemia, *Corresponding author: Banu Buyukaydin, azotemia and elevation of liver enzymes. Histological result of the excisional Bezmialem Vakif University, Department of Internal lymph node biopsy was compatible with peripheral T cell lymphoma. In ward, Medicine, Turkey the patient has repeated recurrent hypoglycemia, which did not resolve with all treatment given. His general condition deteriorated and he died due to sepsis. Received: June 01, 2016; Accepted: July 10, 2016; This case highlighted the need to rule out hematologic malignancies; precisely Published: July 13, 2016 T-cell lymphoma in a patient who presented with resistant hypoglycemia in the presence of lymphadenopathy. Keywords: Hypoglycemia, Lymphoma, IGF-II Introduction approximately fifty percent of proliferation index. CD3 was positive. This finding was compatible to histological diagnosis of peripheral Hypoglycemia is defined as the occurrence of a variety of T-cell lymphoma with partial involvement of lymph ganglia. symptoms in association with plasma glucose concentration of 50mg/dl or less. -

Bilirubin As a New Biomarker of Diabetes and Its Microvascular
Analytica & l B y i tr o s c i h m e m e h i Biochemistry & s c t Nishimura, et al., Biochem Anal Biochem 2016, 5:1 o r i y B DOI: 10.4172/2161-1009.1000245 ISSN: 2161-1009 Analytical Biochemistry Commentary Open Access Bilirubin as a New Biomarker of Diabetes and its Microvascular Complications Takeshi Nishimura*, Masami Tanaka, Risa Sekioka and Hiroshi Itoh Department of Internal Medicine, School of Medicine, Keio University, Tokyo, Japan *Corresponding author: Takeshi Nishimura, Department of Internal Medicine, School of Medicine, Keio University 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan, Tel: 81-3-5363-3797; Fax: 81-3-3359-2745; E-mail: [email protected] Rec date: Feb 06, 2016; Acc date: Feb 12, 2016; Pub date: Feb 15, 2016 Copyright: © 2016 Nishimura T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Commentary elucidate the pathophysiological role of bilirubin in type 1 DM, our results should be verified in large-scale, prospective studies. Hyperglycemia is the hallmark of diabetes mellitus [DM]; it activates certain biochemical pathways leading to micro- and macrovascular complications in diabetic patients [1]. Moreover, References hyperglycemia generates oxidative stress and causes free radical- 1. Takayanagi R, Inoguchi T, Ohnaka K (2011) Clinical and experimental mediated lipid peroxidation [2,3]. In turn, the oxidative stress causes evidence for oxidative stress as an exacerbating factor of diabetes mellitus. -

Clinical and Histopathological Features of Renal Maldevelopment in Boxer Dogs: a Retrospective Case Series (1999–2018) †
animals Article Clinical and Histopathological Features of Renal Maldevelopment in Boxer Dogs: A Retrospective Case Series (1999–2018) † Maria Alfonsa Cavalera 1, Floriana Gernone 1, Annamaria Uva 1, Paola D’Ippolito 2, Xavier Roura 3 and Andrea Zatelli 1,* 1 Department of Veterinary Medicine, University of Bari, 70010 Valenzano, Italy; [email protected] (M.A.C.); fl[email protected] (F.G.); [email protected] (A.U.) 2 Veterinary diagnostic Lab ACV Triggiano, 70019 Triggiano, Italy; [email protected] 3 Hospital Clínic Veterinari, Universitat Autònoma de Barcelona, 08193 Bellaterra, Spain; [email protected] * Correspondence: [email protected]; Tel.: +39-080-4679804 † This study was partially presented as oral communication at the 11th ECVIM-CA/ESVIM Congress, Dublin (Ireland) as “Congenital nephrotic syndrome with renal glomerular immaturity in 7 Boxer dogs”. Zatelli, A., Domenech, O., Bussadori, C., Lubas, G., Del Piero, F. Simple Summary: This study describes clinical findings in Boxer dogs with renal maldevelopment and proposes a possible mode of inheritance. Medical records of 9 female Boxer dogs, older than 5 months and with a clinical diagnosis of proteinuric chronic kidney disease prior to one year of age, showed the presence of polyuria and polydipsia, decreased appetite, weight loss, lethargy and weakness in all affected dogs. Common laboratory findings were proteinuria and diluted urine, non- regenerative anemia, azotemia, hyperphosphatemia, hypoalbuminemia and hypercholesterolemia. Citation: Cavalera, M.A.; Gernone, Histopathology of the kidneys identified the presence of immature glomeruli in all dogs. In 7 out F.; Uva, A.; D’Ippolito, P.; Roura, X.; of 9 related dogs, the pedigree analysis showed that a simple autosomal recessive trait may be a Zatelli, A. -

Hyperosmolar Hyperglycemic State (HHS) Erica Kretchman DO October 19 2018 Speaker for Valeritas, Medtronic, Astrazenica, Boehringer Ingelheim
Hyperosmolar Hyperglycemic State (HHS) Erica Kretchman DO October 19 2018 Speaker for Valeritas, Medtronic, AstraZenica, Boehringer Ingelheim. These do not influence this presentation Objective • Review and understand diagnosis of Hyperosmolar Hyperglycemic State (HHS) and differentiating from Diabetic Ketoacidosis • Treatment of HHS • Complications of HHS Question 1 • Which of the following is NOT a typical finding in HHS? 1. Blood PH <7.30 2. Dehydration 3. Mental Status Changes 4. Osmotic diuresis Question 2 • Hypertonic fluids, such as 3% saline, are the first line of treatment to correct dehydration in HHS 1. True 2. False Question 3 • Which of the following statements is INCORRECT about Hyperosmolar Hyperglycemic State? 1. HHS occurs mainly in type 2 diabetics. 2. This condition presents without ketones in the urine. 3. Metabolic alkalosis presents in severe HHS. 4. Intravenous Regular insulin is used to treat hyperglycemia. Hyperosmolar Hyperglycemic State (HHS) • HHS and DKA are of two of the most serious complications form Diabetes • Hospital admissions for HHS are lower than the rate for DKA and accounts for less than 1 percent of all primary diabetic admissions • Mortality rate for patients with HHS is between 10 and 20 percent, which is approximately 10 times higher than that for DKA • Declined between 1980 and 2009 • Typically from precipitating illness - rare from HHS itself PRECIPITATING FACTORS • The most common events are infection (often pneumonia or urinary tract infection) and discontinuation of or inadequate insulin -

SIRS Is Valid in Discriminating Between Severe and Moderate Diabetic Foot Infections
Pathophysiology/Complications ORIGINAL ARTICLE SIRS Is Valid in Discriminating Between Severe and Moderate Diabetic Foot Infections 1 2 DANE K. WUKICH, MD KATHERINE MARIE RASPOVIC, DPM best of our knowledge, the use of SIRS 2 3 KIMBERLEE B. HOBIZAL, DPM BEDDA L. ROSARIO, PHD has not yet been validated as a method of discriminating between moderate and severe DFI. OBJECTIVEdThis retrospective, single-center study was designed to distinguish severe di- The aim of this study was to classify abetic foot infection (DFI) from moderate DFI based on the presence or absence of systemic fl infectionseverityinagroupofhospital- in ammatory response syndrome (SIRS). ized diabetic patients based on the pres- RESEARCH DESIGN AND METHODSdThe database of a single academic foot and ence or absence of SIRS. The reason for ankle program was reviewed and 119 patients were identified. Severe DFI was defined as local hospitalization in this group of patients infection associated with manifestation of two or more objective findings of systemic toxicity was their DFI. Our hypotheses are that using SIRS criteria. patients with DFI who manifest SIRS (i.e., severe infection) will have longer hospital RESULTSdPatients with severe DFI experienced a 2.55-fold higher risk of any amputation – – stays and higher rates of major amputa- (95% CI 1.21 5.36) and a 7.12-fold higher risk of major amputation (1.83 41.05) than patients tion than patients who don’tmanifest with moderate DFI. The risk of minor amputations was not significantly different between the two groups (odds ratio 1.02 [95% CI 0.51–2.28]). The odds of having a severe DFI was 7.82 SIRS (i.e., moderate infection). -

Type 2 Diabetes Mellitus in Children and Adolescents
CLINICAL Type 2 diabetes mellitus in children and adolescents Kung-Ting Kao, Matthew A Sabin Background ype 2 diabetes mellitus (T2DM), and obesity. Furthermore, treatment previously known as non-insulin options are limited by the lack of licenced The incidence of type 2 diabetes mellitus T dependent diabetes or adult- treatment modalities in the paediatric (T2DM) in children and adolescents is onset diabetes, is a disorder arising from population, and adherence, psychosocial increasing, mirroring the epidemic of insulin resistance and relative (rather than health and wellbeing are often poor.7 paediatric obesity. Early-onset T2DM is absolute) insulin deficiency in the absence Early-onset T2DM is associated with associated with poor long-term outcomes. of autoimmune beta-cell destruction.1 It is significant long-term morbidity and Objectives a polygenic disorder involving interactions mortality. Adolescents diagnosed with between genetic and environmental T2DM are predicted to lose 15 years from In this article, we describe the growing risk factors that result in the underlying their remaining life expectancy when problem of early-onset T2DM in Australia, pathophysiology of hepatic and muscle compared with their peers who do not explore the difference between early- insulin resistance, and subsequent beta-cell have T2DM.8 Complications of diabetes onset and adult-onset T2DM, and review failure.2 Most patients with this disorder are also common and present even earlier the management of T2DM in children and are obese, and T2DM often remains than in adolescents with type 1 diabetes adolescents. undiagnosed for many years while the mellitus (T1DM).9,10 A long-term study patient progresses symptom-free through in Japan found that over a period of 20 Discussion the earlier stages of hyperglycaemia known years, 24% of the 1063 participants were 11 T2DM is difficult to differentiate from the as ‘pre-diabetes’. -

Correlation Between Glycated Hemoglobin and Venous Blood Sugar in Diabetic Patients Monitored in Abidjan
Vol. 14(4), pp. 135-141, October-December 2020 DOI: 10.5897/AJBR2020.1102 Article Number: CD65C6E65033 ISSN 1996-0778 Copyright © 2020 Author(s) retain the copyright of this article African Journal of Biochemistry Research http://www.academicjournals.org/AJBR Full Length Research Paper Correlation between glycated hemoglobin and venous blood sugar in diabetic patients monitored in Abidjan MONDE Aké Absalome1*, CAMARA-CISSE Massara2, KOFFI Konan Gervais2, DIALLO Issiagha3, AKE AKE Alexandre4, YAPO-AKE Bénédicte4, ECRABEY Yann Christian3, KOUAKOU Francisk3, BENE YAO Roger Espérance4 and TIAHOU Georges5 1Félix HOUPHOUËT-BOIGNY University, Cocody, Abidjan, Côte d’Ivoire. 2Biochemistry Laboratory, Abidjan Medical School, Félix HOUPHOUËT BOIGNY University, Côte D'ivoire. 3Biochemistry Laboratory, University Hospital Center of Treichville, Côte D'ivoire. 4Laboratory of Medical Biochemistry, Faculty of Medical Sciences, Félix HOUPHOUËT-BOIGNY University, Côte D'ivoire. 5Laboratory of Medical Biochemistry, Faculty of Medical Sciences, Alassane OUATTARA University, Bouaké, Côte D'ivoire. Received 23 August, 2020; Accepted 2 October, 2020 The aim of this study was to determine the correlation between glycated hemoglobin and blood sugar levels in diabetic subjects carried out in Abidjan. This cross-sectional study included 100 patients with diabetes monitored, for three months, for whom glycated blood glucose and hemoglobin were performed, this after informed consent of the patients. Pearson and Spearman correlation tests were used, at the 5% threshold. The patients with normal HbA1C and normal blood glucose accounted for 55.34 and 32%, respectively. A sedentary lifestyle and body mass index > 25 kg/m² were associated with a significant increase in the risk of increased blood glucose and HbA1C. -

Glycation of Fetal Hemoglobin Reflects Hyperglycemia Exposure
2830 Diabetes Care Volume 37, October 2014 Felix O. Dupont,1 Marie-France Hivert,1,2,3 Glycation of Fetal Hemoglobin Catherine Allard,1 Julie Menard,´ 1 Patrice Perron,1,2 Luigi Bouchard,1,4,5 Reflects Hyperglycemia Exposure Julie Robitaille,6 Jean-Charles Pasquier,1,7 Christiane Auray-Blais,1,8 and In Utero Jean-Luc Ardilouze1,2 Diabetes Care 2014;37:2830–2833 | DOI: 10.2337/dc14-0549 OBJECTIVE The lifetime risk of metabolic diseases in offspring of women with gestational diabetes mellitus (GDM) depends, at least in part, on the impact of glycemic fetal programming. To quantify this impact, we have developed and validated a unique mass spectrometry method to measure the percentage of glycated hemoglobin in cord blood. RESEARCH DESIGN AND METHODS This case-control study includes 37 GDM women and 30 pregnant women with normal glucose tolerance (NGT). RESULTS Glycation of the a-chain (Gla) was higher in neonates from GDM (2.32 vs. 2.20%, P < 0.01). Gla strongly correlated with maternal A1C measured at delivery in the r P < r P < overall cohort ( =0.67, 0.0001) as well as in each group (GDM: = 0.66, 1 r P Centre de Recherche du Centre Hospitalier Uni- 0.0001; NGT: = 0.50, = 0.01). versitaire de Sherbrooke, Sherbrooke, QC, Canada 2Endocrine Division, Universite´ de Sherbrooke, CONCLUSIONS Sherbrooke, QC, Canada Thus, Gla may reflect hyperglycemic exposure during the last weeks of fetal de- 3Harvard Pilgrim Health Care Institute, Depart- velopment. Future studies will confirm Gla is a predictive biomarker of prenatally ment of Population Medicine, Harvard Medical School, Boston, MA programmed lifetime metabolic health and disease. -

Glucose Metabolism Before and After Radioiodine Therapy of a Patient with Graves' Disease: Assessment by Continuous Glucose Monitoring
BIOMEDICAL REPORTS 7: 183-187, 2017 Glucose metabolism before and after radioiodine therapy of a patient with Graves' disease: Assessment by continuous glucose monitoring YUN HU, GU GAO, RENG-NA YAN, FENG-FEI LI, XIAO-FEI SU and JIAN-HUA MA Department of Endocrinology, Nanjing First Hospital, Nanjing Medical University, Nanjing, Jiangsu 210012, P.R. China Received March 17, 2017; Accepted June 7, 2017 DOI: 10.3892/br.2017.932 Abstract. Hyperthyroidism causes impaired glucose toler- as well as a diagnostic test for diabetes mellitus. However, ance, insulin resistance (IR) and insulin secretion. However, previous studies identified that HbA1c is not a reliable diag- the glucose variability affected by thyroid dysfunction remains nostic test for diabetes in the presence of hyperthyroidism or unclear. Glucose variability was assessed by continuous hypothyroidism (9,10). glucose monitoring (CGM) in a non-diabetic patient with The prevalent use of continuous glucose monitoring Graves' disease (GD), to the best of our knowledge, for the (CGM) has provided details on glycemic variation that were first time. A 28‑year‑old man with GD, who had been taking otherwise not possible with HbA1c or self-monitoring of methimazole for 4 years, was treated with radioiodine on blood glucose (SMBG). Torimoto et al (11) reported the use August 17th 2016. Although the patient exhibited normal of CGM in a patient with Graves' disease (GD) complicated glycated hemoglobin (HbA1c; 5.3%) and blood glucose values by diabetes mellitus. The authors demonstrated that hyper- during the oral glucose tolerance test (OGTT; fasting and thyroidism induces elevation of postprandial blood glucose 120 min blood glucose were 5.38 and 6.39 mmol/l, respec- (PBG) and fasting blood glucose (FBG) levels due to the dawn tively) before radioiodine therapy, CGM exhibited high 24 h phenomenon, and that glycemic variation is alleviated with mean glucose and nocturnal hyperglycemia. -
Copyrighted Material
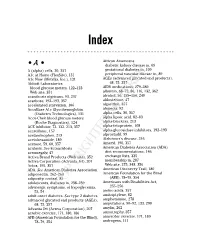
34_568205 bindex.qxd 5/28/04 11:03 AM Page 365 Index African Americans • A • diabetic kidney disease in, 69 A (alpha) cells, 30, 357 gestational diabetes in, 109 A1c at Home (FlexSite), 131 peripheral vascular disease in, 89 A1c Now (Metrika, Inc.), 131 AGEs (advanced glycated end products), Abbott Laboratories 68, 75, 357 blood glucose meters, 122–123 AIDS medications, 279–280 Web site, 351 albumin, 68–72, 86, 116, 132, 362 acanthosis nigricans, 93, 237 alcohol, 56, 155–156, 240 acarbose, 192–193, 357 aldosterone, 47 accelerated starvation, 106 algorithm, 357 AccuBase A1c Glycohemoglobin alopecia, 92 (Diabetes Technologies), 131 alpha cells, 30, 357 Accu-Chek blood glucose meters alpha lipoic acid, 82–83 (Roche Diagnostics), 124 alpha-blockers, 213 ACE inhibitor, 72, 132, 213, 357 alpha-fetoprotein, 108 acesulfame, 157 alpha-glucosidase inhibitors, 192–193 acetaminophen, 213 alprostadil, 99 acetohexamide, 189 Alzheimer’s disease, 246 acetone, 59, 60, 357 Amaryl, 190, 357 acidosis. See ketoacidosis American Diabetes Association (ADA) acromegaly, 47 diet recommendations, 146 Activa Brand Products (Web site), 352 exchange lists, 335 Activa Corporation (Advanta Jet), 207 membership in, 287 Actos, 195, 357 Web site, 275, 348, 356 ADA. See American Diabetes Association American Discovery Trail, 180 adiponectin, 262–263 American Foundation for the Blind adiposity, central, 85 (AFB), 78–79, 354 adolescents, diabetes in, 238–239 Americans with Disabilities Act, adrenergic symptoms,COPYRIGHTED of hypoglycemia, 255–256 MATERIAL 53, 54 amino acids, -

Hyperosmolar Hyperglycemic State (HHS) Is the Most Serious Acute Hypergly- Cemic Emergency in Patients with Type 2 Diabetes
3124 Diabetes Care Volume 37, November 2014 Francisco J. Pasquel and Hyperosmolar Hyperglycemic Guillermo E. Umpierrez State: A Historic Review of the Clinical Presentation, Diagnosis, and Treatment Diabetes Care 2014;37:3124–3131 | DOI: 10.2337/dc14-0984 The hyperosmolar hyperglycemic state (HHS) is the most serious acute hypergly- cemic emergency in patients with type 2 diabetes. von Frerichs and Dreschfeld described the first cases of HHS in the 1880s in patients with an “unusual diabetic coma” characterized by severe hyperglycemia and glycosuria in the absence of Kussmaul breathing, with a fruity breath odor or positive acetone test in the urine. Current diagnostic HHS criteria include a plasma glucose level >600 mg/dL and increased effective plasma osmolality >320 mOsm/kg in the absence of ketoacidosis. The incidence of HHS is estimated to be <1% of hospital admissions of patients with diabetes. The reported mortality is between 10 and 20%, which is about 10 times higher than the mortality rate in patients with diabetic ketoacidosis (DKA). Despite the severity of this condition, no prospective, randomized studies have determined best REVIEW treatment strategies in patients with HHS, and its management has largely been extrapolated from studies of patients with DKA. There are many unresolved questions that need to be addressed in prospective clinical trials regarding the pathogenesis and treatment of pediatric and adult patients with HHS. The hyperosmolar hyperglycemic state (HHS) is a syndrome characterized by severe hyperglycemia, hyperosmolality, and dehydration in the absence of ketoacidosis. The exact incidence of HHS is not known, but it is estimated to account for ,1% of hospital admissions in patients with diabetes (1).