ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic Ketoacidosis and the Hyperglycem
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

First-Year Experience of Medical Emergency Care, a New Healthcare Chain for Acute Life-Threatening Medical Conditions at the ED
Research Article Published: 13 Dec, 2018 Journal of Cardiology Forecast First-Year Experience of Medical Emergency Care, a New Healthcare Chain for Acute Life-Threatening Medical Conditions at the ED Bergh N2,3*, Hellberg J1,3, Rehnström K1, Karlsson T4, Ekerstad N5,6 and Karlson BW1,2 1Department of Acute and Internal Medicine, NU (NÄL-Uddevalla) Hospital Group, Trollhättan-Uddevalla- Vänersborg, Sweden 2Department of Molecular and Clinical Medicine, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden 3Department of Cardiology, Sahlgrenska University Hospital, Sahlgrenska, Gothenburg, Sweden 4Health Metrics Unit, Institution of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden 5Department of Cardiology, NU (NÄL-Uddevalla) Hospital Group, Trollhättan-Uddevalla-Vänersborg, Sweden 6Department of Medical and Health Sciences, Division of Health Care Analysis, Linköping University, Linköping, Sweden Abstract Background: There is a high inflow of patients at most medical emergency departments (ED). In 2013 the Medical Emergency Care (MEC) healthcare chain was introduced at the NU-hospital group, Sweden, in order to better identify, alerting and treat the critically ill adult medical patients. Aim: The primary aim of this retrospective study was to characterize medical patients who were judged and handled as critically ill according to the concept of MEC during the first year following its introduction. OPEN ACCESS Methods: This is a single-center, consecutive cohort study of all patients initially taken care of at the ED using the concept of MEC at the NU Hospital group, Västra Götaland health care region, * Correspondence: Sweden, between February 26 2013 and February 28 2014. Niklas Bergh, Department of Molecular and Clinical Medicine, Department Results: A total of 856 patients were registered as MEC patients, representing 3.2% of all adult medical ED patients. -

20Mg Spironolactone I.P…..50Mg
For the use only of a Registered Medical Practitioner or Hospital or a Laboratory. This package insert is continually updated: Please read carefully before using a new pack Frusemide and Spironolactone Tablets Lasilactone® 50 COMPOSITION Each film coated tablet contains Frusemide I.P. …….. 20mg Spironolactone I.P…..50mg THERAPEUTIC INDICATIONS Lasilactone® contains a short-acting diuretic and a long-acting aldosterone antagonist. It is indicated in the treatment of resistant oedema where this is associated with secondary hyperaldosteronism; conditions include chronic congestive cardiac failure and hepatic cirrhosis. Treatment with Lasilactone® should be reserved for cases refractory to a diuretic alone at conventional doses. This fixed ratio combination should only be used if titration with the component drugs separately indicates that this product is appropriate. The use of Lasilactone® in the management of essential hypertension should be restricted to patients with demonstrated hyperaldosteronism. It is recommended that in these patients also, this combination should only be used if titration with the component drugs separately indicates that this product is appropriate. POSOLOGY AND METHOD OF ADMINISTRATION For oral administration. The dose must be the lowest that is sufficient to achieve the desired effect. Adults: 1-4 tablets daily. Children: The product is not suitable for use in children. Elderly: Frusemide and Spironolactone may both be excreted more slowly in the elderly. Tablets are best taken at breakfast and/or lunch with a generous amount of liquid (approx. 1 glass). An evening dose is not recommended, especially during initial treatment, because of the increased nocturnal output of urine to be expected in such cases. -

Hyperosmolar Hyperglycemic State (HHS) Erica Kretchman DO October 19 2018 Speaker for Valeritas, Medtronic, Astrazenica, Boehringer Ingelheim
Hyperosmolar Hyperglycemic State (HHS) Erica Kretchman DO October 19 2018 Speaker for Valeritas, Medtronic, AstraZenica, Boehringer Ingelheim. These do not influence this presentation Objective • Review and understand diagnosis of Hyperosmolar Hyperglycemic State (HHS) and differentiating from Diabetic Ketoacidosis • Treatment of HHS • Complications of HHS Question 1 • Which of the following is NOT a typical finding in HHS? 1. Blood PH <7.30 2. Dehydration 3. Mental Status Changes 4. Osmotic diuresis Question 2 • Hypertonic fluids, such as 3% saline, are the first line of treatment to correct dehydration in HHS 1. True 2. False Question 3 • Which of the following statements is INCORRECT about Hyperosmolar Hyperglycemic State? 1. HHS occurs mainly in type 2 diabetics. 2. This condition presents without ketones in the urine. 3. Metabolic alkalosis presents in severe HHS. 4. Intravenous Regular insulin is used to treat hyperglycemia. Hyperosmolar Hyperglycemic State (HHS) • HHS and DKA are of two of the most serious complications form Diabetes • Hospital admissions for HHS are lower than the rate for DKA and accounts for less than 1 percent of all primary diabetic admissions • Mortality rate for patients with HHS is between 10 and 20 percent, which is approximately 10 times higher than that for DKA • Declined between 1980 and 2009 • Typically from precipitating illness - rare from HHS itself PRECIPITATING FACTORS • The most common events are infection (often pneumonia or urinary tract infection) and discontinuation of or inadequate insulin -

Preserved Physical Fitness Is Associated with Lower 1-Year Mortality in Frail Elderly Patients with a Severe Comorbidity Burden
Journal name: Clinical Interventions in Aging Article Designation: Original Research Year: 2019 Volume: 14 Clinical Interventions in Aging Dovepress Running head verso: Åhlund et al Running head recto: Åhlund et al open access to scientific and medical research DOI: 198591 Open Access Full Text Article ORIGINAL RESEARCH Preserved physical fitness is associated with lower 1-year mortality in frail elderly patients with a severe comorbidity burden This article was published in the following Dove Medical Press journal: Clinical Interventions in Aging Kristina Åhlund1,2 Introduction: Physical deterioration in connection with a care episode is common. The aim Niklas Ekerstad3,4 of this study was, in frail elderly patients with a severe comorbidity burden, to analyze 1) the Maria Bäck2,5 association between physical fitness measurements and 1-year mortality and 2) the association Björn W Karlson6,7 between preserved physical fitness during the first three months after discharge from emergency Birgitta Öberg2 hospital care and 1-year prognosis. Methods: Frail elderly patients ($75 years) in need of inpatient emergency medical care were 1Department of Physiotherapy, NU included. Aerobic capacity (six-minute walk test, 6MWT) and muscle strength (handgrip strength Hospital Group, Trollhättan, Sweden; 2Department of Medical and Health test, HS) were assessed during the hospital stay and at a three-month follow-up. The results Sciences, Division of Physiotherapy, were analyzed using multivariate Cox regression; 1) 0–12-month analysis and 2) 0–3-month Linköping University, Linköping, For personal use only. Sweden; 3Department of Research and change in physical fitness in relation to 1-year mortality. The analyses were adjusted for age, Development, NU Hospital Group, gender, comorbidity and frailty. -

Are Frail Elderly Patients Treated in a CGA Unit More Satisfied with Their Hospital Care Than Those Treated in Conventional Acute Medical Care?
Journal name: Patient Preference and Adherence Article Designation: Original Research Year: 2018 Volume: 12 Patient Preference and Adherence Dovepress Running head verso: Ekerstad et al Running head recto: Comparison of acute treatment in CGA units and in conventional wards open access to scientific and medical research DOI: http://dx.doi.org/10.2147/PPA.S154658 Open Access Full Text Article ORIGINAL RESEARCH Are frail elderly patients treated in a CGA unit more satisfied with their hospital care than those treated in conventional acute medical care? Niklas Ekerstad1,2 Objectives: Our aim was to study whether the acute care of frail elderly patients directly Göran Östberg3 admitted to a comprehensive geriatric assessment (CGA) unit is superior to the care in a con- Maria Johansson3 ventional acute medical care unit in terms of patient satisfaction. Björn W Karlson3,4 Design: TREEE (Is the TReatment of frail Elderly patients Effective in an Elderly care unit?) is a clinical, prospective, controlled, one-center intervention trial comparing acute treatment in 1Department of Cardiology, NU (NÄL-Uddevalla) Hospital Group, CGA units and in conventional wards. Trollhättan-Uddevalla-Vänersborg, Setting: This study was conducted in the NÄL-Uddevalla county hospital in western Sweden. 2 Department of Medical and Health Participants: In this follow-up to the TREEE study, 229 frail patients, aged $75 years, in need Sciences, Division of Health Care Analysis, Linköping University, of acute in-hospital treatment, were eligible. Of these patients, 139 patients were included in 3 For personal use only. Linköping, Division of Internal and the analysis, 72 allocated to the CGA unit group and 67 to the conventional care group. -
Preventing Dehydration
State of New Jersey Department of Human Services Division of Developmental Disabilities DDDDDD PREVENTIONPREVENTION BULLETINBULLETIN Dehydration Dehydration is a loss of too much fluid from the body. The body needs water in order to maintain normal functioning. If your body loses too much fluid - more than you are getting from your food and liquids - your body loses electrolytes. Electrolytes include important nutrients like sodium and potassium which your body needs to work normally. A person can be at risk for dehydration in any season, not just the summer months. It is also important to know that elderly individuals are at heightened risk for dehydration because their bodies have a lower water content than younger people. Why people with Common Causes and a developmental Risk Factors for disability may be Dehydration: at a higher risk for dehydration. v Diarrhea v Vomiting v People with physical limitations may v Excessive sweating not be able to get something to drink on their own and will need the assistance of v Fever others. v Burns v People who cannot speak or whose v Diabetes when blood sugar is too high speech is hard to understand may have a v hard time telling their support staff that Increased urination (undiagnosed diabetes) they are thirsty. v Not drinking enough water, especially on warm and hot days v Some people may have difficulty swal- lowing their food or drinks and may v Not drinking enough during or after exercise refuse to eat or drink. This can make v Some medications (diuretics, blood pressure them more susceptible to becoming meds, certain psychotropic and anticonvul- dehydrated. -
The Effect of Dehydration, Hyperthermia, and Fatigue on Landing Error Scoring System Scores
ABSTRACT THE EFFECT OF DEHYDRATION, HYPERTHERMIA, AND FATIGUE ON LANDING ERROR SCORING SYSTEM SCORES Purpose: To examine the effects of exercise-induced dehydration, hyperthermia, and fatigue on Landing Error Scoring System (LESS) scores during a jump-landing task, and the effectiveness of a personalized hydration plan. Methods: Five recreationally active heat-acclimatized males 25.4 y (SD=5.7) completed two trials: with fluid replacement, (EXP) and without fluid (CON), in a counterbalanced, randomized, cross-over fashion. Exercise was terminated when gastrointestinal temperature (Tgi) = 39.5°C and fatigue ≥ 7/10, or 90 min of exercise. Percent dehydration was determined by body mass change from pre- exercise (PRE) and post-exercise (POST). Tgi, heart rate (HR), and perceived fatigue were measured PRE, during exercise, and POST. Three jump-landing tasks were filmed in the frontal and sagittal planes. An experienced grader evaluated jump-landing tasks using the LESS. Statistical Analysis: Repeated measures ANOVA assessed primary dependent and independent variables while a priori dependent t-tests evaluated pairwise comparisons. Results: No interaction, group, or time main effects were observed for LESS scores (p=0.437). POST dehydration (%) was greater in CON (M=2.59, SD=0.52) vs. EXP (M=0.92, SD=0.41; p<0.001), whereas hyperthermia (°C) (CON, M=39.29, SD=0.31, EXP, M=39.03, SD=0.61; p=0.425), and fatigue (CON, M=9, SD=1, EXP, M=9, SD=2; p=0.424) were similar. Conclusion: LESS scores were not affected by exercise-induced dehydration, hyperthermia, and fatigue, nor by a personal hydration plan. -
A Roadmap for Improving Wikipedia 29/08 2017
Embargo Tuesday 29th August at 00:05 [UK time] Press release 29/08 A roadmap for improving Wikipedia The evolution of Wikipedia’s medical content: past, present and future 2017 Shafee T, Masukume G, Kipersztok L, Das D, Häggström M, Heilman J. (2017) Journal of Epidemiology & Community Health 71(10) Wikipedia is a key source of public health information Wikipedia needs expert input Health professionals need Wikipedia’s reach Image: Blausen medical CC BY-SA, via WikiJournal of Medicine (full res version) doi:10.15347/wjm/2014.010. Given its prominence as a source of scientific and medical information, improving Wikipedia is a public health “Wikipedia has over 44 million necessity. How can the medical and scientific community articles across 295 languages work towards enhancing the quality and quantity of its and climbing, but contributor medical articles? An international group of doctors and numbers are pretty flat.” researchers have outlined their recommendations in the Journal of Epidemiology and Community Health. The encyclopedia’s content, community and collaborations have changed a lot over the last 16 years. Now is also the time to plan improvements for its future. The Wikimedia Foundation, the charity that supports Wikipedia, is currently updating their strategy through to 2030. It’s therefore an ideal “At 16 years old, Wikipedia is opportunity for those with an interest in disseminating a teenager, and going through biomedical information to become involved in some changes.” Wikipedia. The authors identify four main areas that can be used to improve the encyclopedia. doi.org/10.1136/jech-2016-208601 Embargo Tuesday 29th August at 00:05 [UK time] Individual Wikipedia is built entirely by volunteers. -

Polymyalgia Rheumatica Mimicking an Iliopsoas Abscess
Central Annals of Orthopedics & Rheumatology Case Report *Corresponding author Lennart Dimberg, Department of Public Health and Community Medicine, the Sahlgrenska Academy, University of Gothenburg, Box 454, SE-405 30 Polymyalgia Rheumatica Gothenburg, Sweden, Email: [email protected] Submitted: 30 November 2020 Mimicking an Iliopsoas Abscess Accepted: 12 December 2020 Published: 15 December 2020 Lennart Dimberg1* and Fredrik Wennerberg2 Copyright 1Department of Public Health and Community Medicine, the Sahlgrenska Academy, © 2020 Dimberg L, et al. University of Gothenburg, Sweden OPEN ACCESS 2Radiology Resident Physician/MD, NU Hospital Group/NU-sjukvården, Sweden Keywords • Case report Abstract • Polymyalgia rheumatic Background: Polymyalgia Rheumatica (PMR) is a clinical condition characterized • Iliopsoas abscess by pain and stiffness of proximal muscles of shoulders and hips. We here present an unusual case initially believed to be an abscess of the iliopsoas muscle. Case presentation: An elderly man visited our clinic with symptoms of left hip pain and stiffness and an elevated erythrocyte sedimentation rate (ESR) at 96 mm/h, but no fever. An MRI of the left hip and proximal femur suggested an iliopsoas abscess, which was aspirated with clear yellow fluid and no bacteria. A few weeks later, additional pain and stiffness of the muscles of both shoulders made a diagnosis of PMR suspicious. A prompt response to high doses of Prednisolone confirmed the diagnosis. Conclusion: PMR may present with hip-pain due to a unilateral iliopsoas bursitis. BACKGROUND An iliopsoas abscess is a rare condition, often appearing with vague clinical features. In a review article by Lee et al, during 1988-1998 a major Taiwanese hospital registered about one case per year Lee et al, [1] The affected individual typically presents with fever, back-pain and limp. -

Type 2 Diabetes Mellitus in Children and Adolescents
CLINICAL Type 2 diabetes mellitus in children and adolescents Kung-Ting Kao, Matthew A Sabin Background ype 2 diabetes mellitus (T2DM), and obesity. Furthermore, treatment previously known as non-insulin options are limited by the lack of licenced The incidence of type 2 diabetes mellitus T dependent diabetes or adult- treatment modalities in the paediatric (T2DM) in children and adolescents is onset diabetes, is a disorder arising from population, and adherence, psychosocial increasing, mirroring the epidemic of insulin resistance and relative (rather than health and wellbeing are often poor.7 paediatric obesity. Early-onset T2DM is absolute) insulin deficiency in the absence Early-onset T2DM is associated with associated with poor long-term outcomes. of autoimmune beta-cell destruction.1 It is significant long-term morbidity and Objectives a polygenic disorder involving interactions mortality. Adolescents diagnosed with between genetic and environmental T2DM are predicted to lose 15 years from In this article, we describe the growing risk factors that result in the underlying their remaining life expectancy when problem of early-onset T2DM in Australia, pathophysiology of hepatic and muscle compared with their peers who do not explore the difference between early- insulin resistance, and subsequent beta-cell have T2DM.8 Complications of diabetes onset and adult-onset T2DM, and review failure.2 Most patients with this disorder are also common and present even earlier the management of T2DM in children and are obese, and T2DM often remains than in adolescents with type 1 diabetes adolescents. undiagnosed for many years while the mellitus (T1DM).9,10 A long-term study patient progresses symptom-free through in Japan found that over a period of 20 Discussion the earlier stages of hyperglycaemia known years, 24% of the 1063 participants were 11 T2DM is difficult to differentiate from the as ‘pre-diabetes’. -
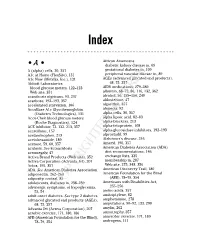
Copyrighted Material
34_568205 bindex.qxd 5/28/04 11:03 AM Page 365 Index African Americans • A • diabetic kidney disease in, 69 A (alpha) cells, 30, 357 gestational diabetes in, 109 A1c at Home (FlexSite), 131 peripheral vascular disease in, 89 A1c Now (Metrika, Inc.), 131 AGEs (advanced glycated end products), Abbott Laboratories 68, 75, 357 blood glucose meters, 122–123 AIDS medications, 279–280 Web site, 351 albumin, 68–72, 86, 116, 132, 362 acanthosis nigricans, 93, 237 alcohol, 56, 155–156, 240 acarbose, 192–193, 357 aldosterone, 47 accelerated starvation, 106 algorithm, 357 AccuBase A1c Glycohemoglobin alopecia, 92 (Diabetes Technologies), 131 alpha cells, 30, 357 Accu-Chek blood glucose meters alpha lipoic acid, 82–83 (Roche Diagnostics), 124 alpha-blockers, 213 ACE inhibitor, 72, 132, 213, 357 alpha-fetoprotein, 108 acesulfame, 157 alpha-glucosidase inhibitors, 192–193 acetaminophen, 213 alprostadil, 99 acetohexamide, 189 Alzheimer’s disease, 246 acetone, 59, 60, 357 Amaryl, 190, 357 acidosis. See ketoacidosis American Diabetes Association (ADA) acromegaly, 47 diet recommendations, 146 Activa Brand Products (Web site), 352 exchange lists, 335 Activa Corporation (Advanta Jet), 207 membership in, 287 Actos, 195, 357 Web site, 275, 348, 356 ADA. See American Diabetes Association American Discovery Trail, 180 adiponectin, 262–263 American Foundation for the Blind adiposity, central, 85 (AFB), 78–79, 354 adolescents, diabetes in, 238–239 Americans with Disabilities Act, adrenergic symptoms,COPYRIGHTED of hypoglycemia, 255–256 MATERIAL 53, 54 amino acids, -

Body Fluid Compartments Dr Sunita Mittal
Body fluid compartments Dr Sunita Mittal Learning Objectives To learn: ▪ Composition of body fluid compartments. ▪ Differences of various body fluid compartments. ▪Molarity, Equivalence,Osmolarity-Osmolality, Osmotic pressure and Tonicity of substances ▪ Effect of dehydration and overhydration on body fluids Why is this knowledge important? ▪To understand various changes in body fluid compartments, we should understand normal configuration of body fluids. Total Body Water (TBW) Water is 60% by body weight (42 L in an adult of 70 kg - a major part of body). Water content varies in different body organs & tissues, Distribution of TBW in various fluid compartments Total Body Water (TBW) Volume (60% bw) ________________________________________________________________ Intracellular Fluid Compartment Extracellular Fluid Compartment (40%) (20%) _______________________________________ Extra Vascular Comp Intra Vascular Comp (15%) (Plasma ) (05%) Electrolytes distribution in body fluid compartments Intracellular fluid comp.mEq/L Extracellular fluid comp.mEq/L Major Anions Major Cation Major Anions + HPO4- - Major Cation K Cl- Proteins - Na+ HCO3- A set ‘Terminology’ is required to understand change of volume &/or ionic conc of various body fluid compartments. Molarity Definition Example Equivalence Osmolarity Osmolarity is total no. of osmotically active solute particles (the particles which attract water to it) per 1 L of solvent - Osm/L. Example- Osmolarity and Osmolality? Osmolarity is total no. of osmotically active solute particles per 1 L of solvent - Osm/L Osmolality is total no. of osmotically active solute particles per 1 Kg of solvent - Osm/Kg Osmosis Tendency of water to move passively, across a semi-permeable membrane, separating two fluids of different osmolarity is referred to as ‘Osmosis’. Osmotic Pressure Osmotic pressure is the pressure, applied to stop the flow of solvent molecules from low osmolarity to a compartment of high osmolarity, separated through a semi-permeable membrane.