Fructosamine Interpretive Summary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
MEDICAL DIRECTIVE Point of Care Glucose Meter Testing And
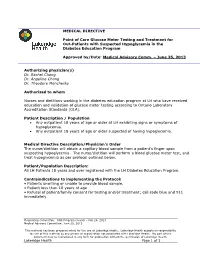
MEDICAL DIRECTIVE Point of Care Glucose Meter Testing and Treatment for Out-Patients with Suspected Hypoglycemia in the Diabetes Education Program Approved by/Date: Medical Advisory Comm. – June 25, 2013 Authorizing physician(s) Dr. Rachel Chong Dr. Angeline Chong Dr. Theodore Monchesky Authorized to whom Nurses and dietitians working in the diabetes education program at LH who have received education and validation of glucose meter testing according to Ontario Laboratory Accreditation Standards (OLA). Patient Description / Population Any outpatient 18 years of age or older at LH exhibiting signs or symptoms of hypoglycemia. Any outpatient 18 years of age or older suspected of having hypoglycemia. Medical Directive Description/Physician’s Order The nurse/dietitian will obtain a capillary blood sample from a patient’s finger upon suspecting hypoglycemia. The nurse/dietitian will perform a blood glucose meter test, and treat hypoglycemia as per protocol outlined below. Patient/Population Description: All LH Patients 18 years and over registered with the LH Diabetes Education Program. Contraindications to implementing the Protocol: • Patients unwilling or unable to provide blood sample. • Patient less than 18 years of age • Refusal of patient/family consent for testing and/or treatment; call code blue and 911 immediately Originating Committee: RNS Program Council – Feb 26, 2013 Medical Advisory Committee: June 25, 2013 This material has been prepared solely for the use at Lakeridge Health. Lakeridge Health accepts no responsibility for use of this material by any person or organization not associated with Lakeridge Health. No part of this document may be reproduced in any form for publication without the permission of Lakeridge Health. -

Diabetes Control in Thyroid Disease
In Brief Thyroid disease is commonly found in most types of diabetes. This article defines the prevalence of thyroid disease in diabetes and elucidates through case studies the assessment, diagnosis, and clinical management of thyroid disease in diabetes. Diabetes Control in Thyroid Disease Thyroid disease is a pathological state abnormality. Several studies, including that can adversely affect diabetes con- the Colorado study, have documented trol and has the potential to negative- a higher prevalence of thyroid disease Jennal L. Johnson, MS, RNC, FNP, ly affect patient outcomes. Thyroid in women, with prevalence rates rang- BC-ADM, CDE disease is found commonly in most ing from 4 to 21%, whereas the rate in forms of diabetes and is associated men ranges from 2.8 to 16%.1 with advanced age, particularly in Thyroid disease increases with age. In type 2 diabetes and underlying the Colorado study, the 18-year-olds autoimmune disease in type 1 dia- had a prevalence rate of 3.5% com- betes. This article defines the preva- pared with a rate of 18.5% for those lence of thyroid disease in diabetes, ≥ 65 years of age. discusses normal physiology and The prevalence of thyroid disease in screening recommendations for thy- diabetes has been estimated at 10.8%,2 roid disease, and elucidates through with the majority of cases occurring as case studies the assessment, diagnosis, hypothyroidism (~ 30%) and subclini- and clinical management of thyroid cal hypothyroidism (~ 50%).2 Hyper- disease and its impact on diabetes. thyroidism accounts for 12%, and postpartum thyroiditis accounts for Thyroid Disease Prevalence 11%.2 Of the female patients with The prevalence of thyroid disease in type 1 diabetes, 30% have thyroid dis- the general population is estimated to ease, with a rate of postpartum thy- be 6.6%, with hypothyroidism the roid disease three times that of the most common malady.1 Participants normal population. -

Refractory Hypoglycemia in T-Cell Lymphoma
Open Access Austin Oncology Case Reports Case Report Refractory Hypoglycemia in T-Cell Lymphoma Buyukaydina B1*, Tunca M1, Alayb M2, Kazanciogluc R3 and Reha E3 Abstract 1Bezmialem Vakif University, Department of Internal Hypoglycemia is commonly seen in diabetes mellitus patients; whereas it Medicine, Turkey is rarely seen in a healthy person. In this case, we reported a male patient 2Yuzuncu Yil University, Department of Endocrinology, with a treatment-resistant hypoglycemia. A 53 years old male patient admitted Turkey to our clinic with debility, nausea and vomiting. Physical examination revealed 3Bezmialem Vakif University, Department of Nephology, lymphadenopathies in the left axilla and inguinal regions; and presence of right Turkey upper quadrant tenderness. Biochemical results revealed severe hypoglycemia, *Corresponding author: Banu Buyukaydin, azotemia and elevation of liver enzymes. Histological result of the excisional Bezmialem Vakif University, Department of Internal lymph node biopsy was compatible with peripheral T cell lymphoma. In ward, Medicine, Turkey the patient has repeated recurrent hypoglycemia, which did not resolve with all treatment given. His general condition deteriorated and he died due to sepsis. Received: June 01, 2016; Accepted: July 10, 2016; This case highlighted the need to rule out hematologic malignancies; precisely Published: July 13, 2016 T-cell lymphoma in a patient who presented with resistant hypoglycemia in the presence of lymphadenopathy. Keywords: Hypoglycemia, Lymphoma, IGF-II Introduction approximately fifty percent of proliferation index. CD3 was positive. This finding was compatible to histological diagnosis of peripheral Hypoglycemia is defined as the occurrence of a variety of T-cell lymphoma with partial involvement of lymph ganglia. symptoms in association with plasma glucose concentration of 50mg/dl or less. -

CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E
Peer Reviewed PRACTICAL ONCOLOGY CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E. Burgess, DVM, Diplomate ACVIM (Oncology) Tufts University An insulinoma is a malignant pancreatic tumor that DIAGNOSIS inappropriately secretes excessive insulin, resulting in Aside from a histologic confirmation of insulinoma, profound hypoglycemia.1 no currently available diagnostic test provides a de- Pancreatic tumors are classified as: finitive diagnosis of insulinoma. Existing techniques • Exocrine, which includes adenocarcinomas of may help increase suspicion for an insulin-secreting ductular or acinar origin tumor but, with most diagnostic testing, it is im- • Endocrine, which arise from the islets of perative to interpret all results in the context of the Langerhans. coexisting clinical signs. Insulinomas are functional neuroendocrine tumors that originate in the beta cells of the islets Differential Diagnosis of Langerhans.1 A complete work-up, including careful patient history, physical examination, bloodwork, and PRESENTATION diagnostic imaging tests, should be performed to Signalment rule out other causes of hypoglycemia, such as Any breed of dog can be affected, but large sepsis, hepatic failure, adrenal cortical insufficiency, breeds tend to be overrepresented.1 While, in toxin ingestion, and other forms of neoplasia. humans, insulinomas affect females far more frequently than males, there is no apparent sex Laboratory Tests predilection in dogs.1-3 Dogs also commonly Blood Glucose present with a malignant variant, while humans A simple fasting blood glucose level of less than often have a benign adenoma (80%).1 Insulino- 40 mg/dL can suggest hyperinsulinemia, although ma is rare in cats.4 careful monitoring of a fasted dog with suspected insulinoma is strongly recommended due to high Clinical Signs risk for seizure activity. -

Bilirubin As a New Biomarker of Diabetes and Its Microvascular
Analytica & l B y i tr o s c i h m e m e h i Biochemistry & s c t Nishimura, et al., Biochem Anal Biochem 2016, 5:1 o r i y B DOI: 10.4172/2161-1009.1000245 ISSN: 2161-1009 Analytical Biochemistry Commentary Open Access Bilirubin as a New Biomarker of Diabetes and its Microvascular Complications Takeshi Nishimura*, Masami Tanaka, Risa Sekioka and Hiroshi Itoh Department of Internal Medicine, School of Medicine, Keio University, Tokyo, Japan *Corresponding author: Takeshi Nishimura, Department of Internal Medicine, School of Medicine, Keio University 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan, Tel: 81-3-5363-3797; Fax: 81-3-3359-2745; E-mail: [email protected] Rec date: Feb 06, 2016; Acc date: Feb 12, 2016; Pub date: Feb 15, 2016 Copyright: © 2016 Nishimura T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Commentary elucidate the pathophysiological role of bilirubin in type 1 DM, our results should be verified in large-scale, prospective studies. Hyperglycemia is the hallmark of diabetes mellitus [DM]; it activates certain biochemical pathways leading to micro- and macrovascular complications in diabetic patients [1]. Moreover, References hyperglycemia generates oxidative stress and causes free radical- 1. Takayanagi R, Inoguchi T, Ohnaka K (2011) Clinical and experimental mediated lipid peroxidation [2,3]. In turn, the oxidative stress causes evidence for oxidative stress as an exacerbating factor of diabetes mellitus. -

Hypoglycemia, Hepatic Dysfunction, Muscle Weakness, Cardiomyopathy
Pediatr. Res. 17: 319-326 (1983) Hypoglycemia, Hepatic Dysfunction, Muscle Weakness, Cardiomyopathy, Free Carnitine Deficiency and Long-Chain Acylcarnitine Excess Responsive to Medium Chain Triglyceride Diet ALLEN M. GLASGOW,'~~'ANDREW G. ENGEL, DENNIS M. BIER, LOWELL W. PERRY, MARY DICKIE, JANE TODARO, BARBARA I. BROWN, AND MERTON F. UTTER Departments of Endocrinology and Metabolism [A.M.G.], Gastroenterology [J. TI, Cardiology [L. W.P.] and Dietary [M.B.], Children's Hospital National Medical Center, Washington, D.C.; Department of Neurology, and the Neuromuscular Research Laboratory [A. G.E.], Mayo Clinic and Mayo Foundation, Rochester, Minnesota USA; Departments of Medicine and Pediatrics [D. M. B.] and Biochemistry [B. I. B.], Washington University, School of Medicine, St. Louis, Missouri, USA; and Department of Biochemistry [MI U.],Case Western Reserve, Cleveland, Ohio, USA Summary Hepatic long-chain acyl CoA carnitine transferase deficiency (4), multiple acyl CoA dehydrogenase deficiency (glutaric aciduria Fraternal twins who had fasting hypoglycemia, hypoketonemia, type 11) (18), and systemic carnitine deficiency (3,9, 12, 17, 24, 37, muscle weakness, and hepatic dysfunction are reported. The he- 43), all of which are associated with impaired fatty acid oxidation, patic dysfunction occurred only during periods of caloric depriva- have hypoglycemia as a major clinical manifestation. tion. The surviving patient developed a cardiomyopathy. In this The purpose of this paper is twofold: (1) to report fraternal sibling, muscle weakness and cardiomyopathy were markedly im- proved by a diet high in medium chain triglycerides. There was a twins with free carnitine deficiency and long-chain acylcarnitine marked deficiency of muscle total carnitine and a mild deficiency excess in whom hypoglycemia, hepatic dysfunction, muscle weak- of hepatic total carnitine. -

Comparative Evaluation of Fructosamine and Hba1c As a Marker of Glycemic Control in Type 2 Diabetes: a Hospital Based Study
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Original Research Article Comparative Evaluation of Fructosamine and HbA1c as a Marker of Glycemic Control in Type 2 Diabetes: A Hospital Based Study Dr. Jyoti Goyal1, Dr. Nibhriti Das2, Dr. Navin Kumar3, Ms. Seema Raghav4, Dr. Paramjeet Singh Bhatia5, Dr. Karunesh Prasad Singh6, Dr. Sabari Das7 1DNB, Department of Internal Medicine, Nayati Healthcare and Research Centre, Mathura, India- 281003, 2Ex-Director of Laboratory services and Additional Dean Research and Academics, Nayati Healthcare and Research Centre, Mathura, India- 281003, 3Ph.D, Biostatistitian, Department of Biostatistics, Nayati Healthcare and Research Centre, Mathura, India-281003. 4M.Sc., Certified Diabetes Educator, Department of Internal Medicine, Nayati Healthcare and Research Centre, Mathura, India-281003. 5MD, Department of Internal Medicine, Nayati Healthcare and Research Centre, Mathura, India-281003. 6MD Physician, Department of Internal Medicine, Nayati Healthcare and Research Centre, Mathura, India-281003. 7Department of Laboratory Medicine, Nayati Healthcare and Research Centre, Mathura, India- 281003, Corresponding Author: Dr. Jyoti Goyal ABSTRACT Introduction: Management of type 2 diabetes revolves around achievement of target glycemic control with the help of antidiabetic drugs or insulin. There are various markers for measurement of glyceamic control like HbA1c, Mean Blood Glucose and fructosamine levels. Though HbA1c is a well validated standard method for assessment of glycemic control but it has also got certain limitations. Fructosamine, a less explored method may be used as an alternative marker for an assessment of glycemic control in cases where HbA1c is unreliable or unavailable. The objective of this study is to compare the fructosamine levels with HbA1c in assessment of glycemic control in type 2 diabetics so as to assess the utility of fructosamine as an alternative marker for evaluation of glucose control. -

Diabetes Is a Disease in Which the Body's Ability to Produce Or Respond
Early Signs and Symptoms of diabetes: Early symptoms of diabetes, especially type 2 diabetes, can be subtle or seemingly harmless. Over time, however, you may Diabetes is a disease in which the develop diabetes complications, even if you body’s ability to produce or respond to haven't had diabetes symptoms. In the the hormone insulin is impaired, United States alone, more than 8 million resulting in abnormal metabolism of people have undiagnosed diabetes, Treatments: carbohydrates and elevated levels of according to the American Diabetes Association. Understanding possible glucose (sugar) in the blood. • Insulin therapy diabetes symptoms can lead to early • Oral medications diagnosis and treatment and a lifetime of Diabetes can be broken down into • better health. If you're experiencing any of Diet changes two types, Type 1 and Type 2. Type 1 • Exercise diabetes involves the the following diabetes signs and symptoms, see your doctor. body attacking itself by The medications you take vary by mistake, this then the type of diabetes and how well the causes the body to stop making insulin. With medicine controls you blood glucose levels. Type 2 diabetes the Type 1 diabetics must have insulin. Type 2 body does not respond may or may not include insulin and may just like it should to the be controlled with diet and exercise alone. insulin the pancreas is If you notice any of these changes notify making. Your body tells the pancreas that it needs to make more insulin since the your health care provider. The earlier • insulin that is already there is not working. -

SIRS Is Valid in Discriminating Between Severe and Moderate Diabetic Foot Infections
Pathophysiology/Complications ORIGINAL ARTICLE SIRS Is Valid in Discriminating Between Severe and Moderate Diabetic Foot Infections 1 2 DANE K. WUKICH, MD KATHERINE MARIE RASPOVIC, DPM best of our knowledge, the use of SIRS 2 3 KIMBERLEE B. HOBIZAL, DPM BEDDA L. ROSARIO, PHD has not yet been validated as a method of discriminating between moderate and severe DFI. OBJECTIVEdThis retrospective, single-center study was designed to distinguish severe di- The aim of this study was to classify abetic foot infection (DFI) from moderate DFI based on the presence or absence of systemic fl infectionseverityinagroupofhospital- in ammatory response syndrome (SIRS). ized diabetic patients based on the pres- RESEARCH DESIGN AND METHODSdThe database of a single academic foot and ence or absence of SIRS. The reason for ankle program was reviewed and 119 patients were identified. Severe DFI was defined as local hospitalization in this group of patients infection associated with manifestation of two or more objective findings of systemic toxicity was their DFI. Our hypotheses are that using SIRS criteria. patients with DFI who manifest SIRS (i.e., severe infection) will have longer hospital RESULTSdPatients with severe DFI experienced a 2.55-fold higher risk of any amputation – – stays and higher rates of major amputa- (95% CI 1.21 5.36) and a 7.12-fold higher risk of major amputation (1.83 41.05) than patients tion than patients who don’tmanifest with moderate DFI. The risk of minor amputations was not significantly different between the two groups (odds ratio 1.02 [95% CI 0.51–2.28]). The odds of having a severe DFI was 7.82 SIRS (i.e., moderate infection). -

Prediabetes: What Is It and What Can I Do?
Prediabetes: What Is It and What Can I Do? What is prediabetes? Weight loss can delay or prevent diabetes. Prediabetes is a condition that comes before Reaching a healthy weight can help you a lot. diabetes. It means your blood glucose levels are If you’re overweight, any weight loss, even higher than normal but aren’t high enough to be 7 percent of your weight (for example, losing called diabetes. about 15 pounds if you weigh 200), may lower your risk for diabetes. There are no clear symptoms of prediabetes. You can have it and not know it. If I have prediabetes, what does it mean? It means you might get type 2 diabetes soon or down the road. You are also more likely to get heart disease or have a stroke. The good news is that you can take steps to delay or prevent type 2 diabetes. How can I delay or prevent type 2 diabetes? You may be able to delay or prevent type 2 diabetes with: Daily physical activity, such as walking. Weight loss, if needed. Losing even a few pounds will help. Medication, if your doctor prescribes it. If you have prediabetes, these steps may bring your blood glucose to a normal range. But you are still at a higher risk for type 2 diabetes. Regular physical activity can delay or prevent diabetes. Being active is one of the best ways to delay or prevent type 2 diabetes. It can also lower your weight and blood pressure, and improve cholesterol levels. Ask your health care team about activities that are safe for you. -

Correlation Between Glycated Hemoglobin and Venous Blood Sugar in Diabetic Patients Monitored in Abidjan
Vol. 14(4), pp. 135-141, October-December 2020 DOI: 10.5897/AJBR2020.1102 Article Number: CD65C6E65033 ISSN 1996-0778 Copyright © 2020 Author(s) retain the copyright of this article African Journal of Biochemistry Research http://www.academicjournals.org/AJBR Full Length Research Paper Correlation between glycated hemoglobin and venous blood sugar in diabetic patients monitored in Abidjan MONDE Aké Absalome1*, CAMARA-CISSE Massara2, KOFFI Konan Gervais2, DIALLO Issiagha3, AKE AKE Alexandre4, YAPO-AKE Bénédicte4, ECRABEY Yann Christian3, KOUAKOU Francisk3, BENE YAO Roger Espérance4 and TIAHOU Georges5 1Félix HOUPHOUËT-BOIGNY University, Cocody, Abidjan, Côte d’Ivoire. 2Biochemistry Laboratory, Abidjan Medical School, Félix HOUPHOUËT BOIGNY University, Côte D'ivoire. 3Biochemistry Laboratory, University Hospital Center of Treichville, Côte D'ivoire. 4Laboratory of Medical Biochemistry, Faculty of Medical Sciences, Félix HOUPHOUËT-BOIGNY University, Côte D'ivoire. 5Laboratory of Medical Biochemistry, Faculty of Medical Sciences, Alassane OUATTARA University, Bouaké, Côte D'ivoire. Received 23 August, 2020; Accepted 2 October, 2020 The aim of this study was to determine the correlation between glycated hemoglobin and blood sugar levels in diabetic subjects carried out in Abidjan. This cross-sectional study included 100 patients with diabetes monitored, for three months, for whom glycated blood glucose and hemoglobin were performed, this after informed consent of the patients. Pearson and Spearman correlation tests were used, at the 5% threshold. The patients with normal HbA1C and normal blood glucose accounted for 55.34 and 32%, respectively. A sedentary lifestyle and body mass index > 25 kg/m² were associated with a significant increase in the risk of increased blood glucose and HbA1C. -

Glycation of Fetal Hemoglobin Reflects Hyperglycemia Exposure
2830 Diabetes Care Volume 37, October 2014 Felix O. Dupont,1 Marie-France Hivert,1,2,3 Glycation of Fetal Hemoglobin Catherine Allard,1 Julie Menard,´ 1 Patrice Perron,1,2 Luigi Bouchard,1,4,5 Reflects Hyperglycemia Exposure Julie Robitaille,6 Jean-Charles Pasquier,1,7 Christiane Auray-Blais,1,8 and In Utero Jean-Luc Ardilouze1,2 Diabetes Care 2014;37:2830–2833 | DOI: 10.2337/dc14-0549 OBJECTIVE The lifetime risk of metabolic diseases in offspring of women with gestational diabetes mellitus (GDM) depends, at least in part, on the impact of glycemic fetal programming. To quantify this impact, we have developed and validated a unique mass spectrometry method to measure the percentage of glycated hemoglobin in cord blood. RESEARCH DESIGN AND METHODS This case-control study includes 37 GDM women and 30 pregnant women with normal glucose tolerance (NGT). RESULTS Glycation of the a-chain (Gla) was higher in neonates from GDM (2.32 vs. 2.20%, P < 0.01). Gla strongly correlated with maternal A1C measured at delivery in the r P < r P < overall cohort ( =0.67, 0.0001) as well as in each group (GDM: = 0.66, 1 r P Centre de Recherche du Centre Hospitalier Uni- 0.0001; NGT: = 0.50, = 0.01). versitaire de Sherbrooke, Sherbrooke, QC, Canada 2Endocrine Division, Universite´ de Sherbrooke, CONCLUSIONS Sherbrooke, QC, Canada Thus, Gla may reflect hyperglycemic exposure during the last weeks of fetal de- 3Harvard Pilgrim Health Care Institute, Depart- velopment. Future studies will confirm Gla is a predictive biomarker of prenatally ment of Population Medicine, Harvard Medical School, Boston, MA programmed lifetime metabolic health and disease.