National Coverage Determination Procedure Code: 82977 Gamma Glutamyl Transferase CMS Policy Number: 190.32 Back to NCD List
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
MEDICAL DIRECTIVE Point of Care Glucose Meter Testing And
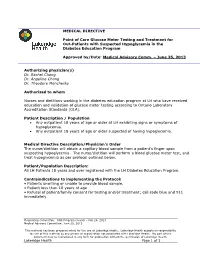
MEDICAL DIRECTIVE Point of Care Glucose Meter Testing and Treatment for Out-Patients with Suspected Hypoglycemia in the Diabetes Education Program Approved by/Date: Medical Advisory Comm. – June 25, 2013 Authorizing physician(s) Dr. Rachel Chong Dr. Angeline Chong Dr. Theodore Monchesky Authorized to whom Nurses and dietitians working in the diabetes education program at LH who have received education and validation of glucose meter testing according to Ontario Laboratory Accreditation Standards (OLA). Patient Description / Population Any outpatient 18 years of age or older at LH exhibiting signs or symptoms of hypoglycemia. Any outpatient 18 years of age or older suspected of having hypoglycemia. Medical Directive Description/Physician’s Order The nurse/dietitian will obtain a capillary blood sample from a patient’s finger upon suspecting hypoglycemia. The nurse/dietitian will perform a blood glucose meter test, and treat hypoglycemia as per protocol outlined below. Patient/Population Description: All LH Patients 18 years and over registered with the LH Diabetes Education Program. Contraindications to implementing the Protocol: • Patients unwilling or unable to provide blood sample. • Patient less than 18 years of age • Refusal of patient/family consent for testing and/or treatment; call code blue and 911 immediately Originating Committee: RNS Program Council – Feb 26, 2013 Medical Advisory Committee: June 25, 2013 This material has been prepared solely for the use at Lakeridge Health. Lakeridge Health accepts no responsibility for use of this material by any person or organization not associated with Lakeridge Health. No part of this document may be reproduced in any form for publication without the permission of Lakeridge Health. -

Diabetes Control in Thyroid Disease
In Brief Thyroid disease is commonly found in most types of diabetes. This article defines the prevalence of thyroid disease in diabetes and elucidates through case studies the assessment, diagnosis, and clinical management of thyroid disease in diabetes. Diabetes Control in Thyroid Disease Thyroid disease is a pathological state abnormality. Several studies, including that can adversely affect diabetes con- the Colorado study, have documented trol and has the potential to negative- a higher prevalence of thyroid disease Jennal L. Johnson, MS, RNC, FNP, ly affect patient outcomes. Thyroid in women, with prevalence rates rang- BC-ADM, CDE disease is found commonly in most ing from 4 to 21%, whereas the rate in forms of diabetes and is associated men ranges from 2.8 to 16%.1 with advanced age, particularly in Thyroid disease increases with age. In type 2 diabetes and underlying the Colorado study, the 18-year-olds autoimmune disease in type 1 dia- had a prevalence rate of 3.5% com- betes. This article defines the preva- pared with a rate of 18.5% for those lence of thyroid disease in diabetes, ≥ 65 years of age. discusses normal physiology and The prevalence of thyroid disease in screening recommendations for thy- diabetes has been estimated at 10.8%,2 roid disease, and elucidates through with the majority of cases occurring as case studies the assessment, diagnosis, hypothyroidism (~ 30%) and subclini- and clinical management of thyroid cal hypothyroidism (~ 50%).2 Hyper- disease and its impact on diabetes. thyroidism accounts for 12%, and postpartum thyroiditis accounts for Thyroid Disease Prevalence 11%.2 Of the female patients with The prevalence of thyroid disease in type 1 diabetes, 30% have thyroid dis- the general population is estimated to ease, with a rate of postpartum thy- be 6.6%, with hypothyroidism the roid disease three times that of the most common malady.1 Participants normal population. -

Refractory Hypoglycemia in T-Cell Lymphoma
Open Access Austin Oncology Case Reports Case Report Refractory Hypoglycemia in T-Cell Lymphoma Buyukaydina B1*, Tunca M1, Alayb M2, Kazanciogluc R3 and Reha E3 Abstract 1Bezmialem Vakif University, Department of Internal Hypoglycemia is commonly seen in diabetes mellitus patients; whereas it Medicine, Turkey is rarely seen in a healthy person. In this case, we reported a male patient 2Yuzuncu Yil University, Department of Endocrinology, with a treatment-resistant hypoglycemia. A 53 years old male patient admitted Turkey to our clinic with debility, nausea and vomiting. Physical examination revealed 3Bezmialem Vakif University, Department of Nephology, lymphadenopathies in the left axilla and inguinal regions; and presence of right Turkey upper quadrant tenderness. Biochemical results revealed severe hypoglycemia, *Corresponding author: Banu Buyukaydin, azotemia and elevation of liver enzymes. Histological result of the excisional Bezmialem Vakif University, Department of Internal lymph node biopsy was compatible with peripheral T cell lymphoma. In ward, Medicine, Turkey the patient has repeated recurrent hypoglycemia, which did not resolve with all treatment given. His general condition deteriorated and he died due to sepsis. Received: June 01, 2016; Accepted: July 10, 2016; This case highlighted the need to rule out hematologic malignancies; precisely Published: July 13, 2016 T-cell lymphoma in a patient who presented with resistant hypoglycemia in the presence of lymphadenopathy. Keywords: Hypoglycemia, Lymphoma, IGF-II Introduction approximately fifty percent of proliferation index. CD3 was positive. This finding was compatible to histological diagnosis of peripheral Hypoglycemia is defined as the occurrence of a variety of T-cell lymphoma with partial involvement of lymph ganglia. symptoms in association with plasma glucose concentration of 50mg/dl or less. -

CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E
Peer Reviewed PRACTICAL ONCOLOGY CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E. Burgess, DVM, Diplomate ACVIM (Oncology) Tufts University An insulinoma is a malignant pancreatic tumor that DIAGNOSIS inappropriately secretes excessive insulin, resulting in Aside from a histologic confirmation of insulinoma, profound hypoglycemia.1 no currently available diagnostic test provides a de- Pancreatic tumors are classified as: finitive diagnosis of insulinoma. Existing techniques • Exocrine, which includes adenocarcinomas of may help increase suspicion for an insulin-secreting ductular or acinar origin tumor but, with most diagnostic testing, it is im- • Endocrine, which arise from the islets of perative to interpret all results in the context of the Langerhans. coexisting clinical signs. Insulinomas are functional neuroendocrine tumors that originate in the beta cells of the islets Differential Diagnosis of Langerhans.1 A complete work-up, including careful patient history, physical examination, bloodwork, and PRESENTATION diagnostic imaging tests, should be performed to Signalment rule out other causes of hypoglycemia, such as Any breed of dog can be affected, but large sepsis, hepatic failure, adrenal cortical insufficiency, breeds tend to be overrepresented.1 While, in toxin ingestion, and other forms of neoplasia. humans, insulinomas affect females far more frequently than males, there is no apparent sex Laboratory Tests predilection in dogs.1-3 Dogs also commonly Blood Glucose present with a malignant variant, while humans A simple fasting blood glucose level of less than often have a benign adenoma (80%).1 Insulino- 40 mg/dL can suggest hyperinsulinemia, although ma is rare in cats.4 careful monitoring of a fasted dog with suspected insulinoma is strongly recommended due to high Clinical Signs risk for seizure activity. -

Rational Design of Resveratrol O-Methyltransferase for the Production of Pinostilbene
International Journal of Molecular Sciences Article Rational Design of Resveratrol O-methyltransferase for the Production of Pinostilbene Daniela P. Herrera 1 , Andrea M. Chánique 1,2 , Ascensión Martínez-Márquez 3, Roque Bru-Martínez 3 , Robert Kourist 2 , Loreto P. Parra 4,* and Andreas Schüller 4,5,* 1 Department of Chemical and Bioprocesses Engineering, School of Engineering, Pontificia Universidad Católica de Chile, Vicuña Mackenna 4860, Santiago 7820244, Chile; [email protected] (D.P.H.); [email protected] (A.M.C.) 2 Institute of Molecular Biotechnology, Graz University of Technology, Petersgasse 14, 8010 Graz, Austria; [email protected] 3 Department of Agrochemistry and Biochemistry, Faculty of Science and Multidisciplinary Institute for Environmental Studies “Ramon Margalef”, University of Alicante, 03690 Alicante, Spain; [email protected] (A.M.-M.); [email protected] (R.B.-M.) 4 Institute for Biological and Medical Engineering, Schools of Engineering, Medicine and Biological Sciences, Pontificia Universidad Católica de Chile, Vicuña Mackenna 4860, Santiago 7820244, Chile 5 Department of Molecular Genetics and Microbiology, School of Biological Sciences, Pontificia Universidad Católica de Chile, Av. Libertador Bernardo O’Higgins 340, Santiago 8320000, Chile * Correspondence: [email protected] (L.P.P.); [email protected] (A.S.) Abstract: Pinostilbene is a monomethyl ether analog of the well-known nutraceutical resveratrol. Both compounds have health-promoting properties, but the latter undergoes rapid metabolization and has low bioavailability. O-methylation improves the stability and bioavailability of resveratrol. In plants, these reactions are performed by O-methyltransferases (OMTs). Few efficient OMTs that Citation: Herrera, D.P.; Chánique, monomethylate resveratrol to yield pinostilbene have been described so far. -

Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

Hypoglycemia, Hepatic Dysfunction, Muscle Weakness, Cardiomyopathy
Pediatr. Res. 17: 319-326 (1983) Hypoglycemia, Hepatic Dysfunction, Muscle Weakness, Cardiomyopathy, Free Carnitine Deficiency and Long-Chain Acylcarnitine Excess Responsive to Medium Chain Triglyceride Diet ALLEN M. GLASGOW,'~~'ANDREW G. ENGEL, DENNIS M. BIER, LOWELL W. PERRY, MARY DICKIE, JANE TODARO, BARBARA I. BROWN, AND MERTON F. UTTER Departments of Endocrinology and Metabolism [A.M.G.], Gastroenterology [J. TI, Cardiology [L. W.P.] and Dietary [M.B.], Children's Hospital National Medical Center, Washington, D.C.; Department of Neurology, and the Neuromuscular Research Laboratory [A. G.E.], Mayo Clinic and Mayo Foundation, Rochester, Minnesota USA; Departments of Medicine and Pediatrics [D. M. B.] and Biochemistry [B. I. B.], Washington University, School of Medicine, St. Louis, Missouri, USA; and Department of Biochemistry [MI U.],Case Western Reserve, Cleveland, Ohio, USA Summary Hepatic long-chain acyl CoA carnitine transferase deficiency (4), multiple acyl CoA dehydrogenase deficiency (glutaric aciduria Fraternal twins who had fasting hypoglycemia, hypoketonemia, type 11) (18), and systemic carnitine deficiency (3,9, 12, 17, 24, 37, muscle weakness, and hepatic dysfunction are reported. The he- 43), all of which are associated with impaired fatty acid oxidation, patic dysfunction occurred only during periods of caloric depriva- have hypoglycemia as a major clinical manifestation. tion. The surviving patient developed a cardiomyopathy. In this The purpose of this paper is twofold: (1) to report fraternal sibling, muscle weakness and cardiomyopathy were markedly im- proved by a diet high in medium chain triglycerides. There was a twins with free carnitine deficiency and long-chain acylcarnitine marked deficiency of muscle total carnitine and a mild deficiency excess in whom hypoglycemia, hepatic dysfunction, muscle weak- of hepatic total carnitine. -

WO 2013/064736 Al 10 May 2013 (10.05.2013) P O P CT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2013/064736 Al 10 May 2013 (10.05.2013) P O P CT (51) International Patent Classification: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, C12N 9/10 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (21) International Application Number: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, PCT/FI2012/05 1048 ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (22) International Filing Date: NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, 3 1 October 2012 (3 1.10.2012) RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (25) Filing Language: English ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 201 16074 1 November 201 1 (01. 11.201 1) FI GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (71) Applicant: VALIO LTD [FI/FI]; Meijeritie 6, FI-00370 TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Helsinki (FI). EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, (72) Inventors: RAJAKARI, Kirsi; c/o Valio Ltd, Meijeritie 6, TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, GW, FI-00370 Helsinki (FI). -

Biosynthetic Investigation of Phomopsins Reveals a Widespread Pathway for Ribosomal Natural Products in Ascomycetes
Biosynthetic investigation of phomopsins reveals a widespread pathway for ribosomal natural products in Ascomycetes Wei Dinga, Wan-Qiu Liua, Youli Jiaa, Yongzhen Lia, Wilfred A. van der Donkb,c,1, and Qi Zhanga,b,1 aDepartment of Chemistry, Fudan University, Shanghai 200433, China; bDepartment of Chemistry, University of Illinois at Urbana–Champaign, Urbana, IL 61801; and cHoward Hughes Medical Institute, University of Illinois at Urbana–Champaign, Urbana, IL 61801 Edited by Jerrold Meinwald, Cornell University, Ithaca, NY, and approved February 23, 2016 (received for review November 24, 2015) Production of ribosomally synthesized and posttranslationally mod- dehydroaspartic acid, 3,4-dehydroproline, and 3,4-dehydrovaline ified peptides (RiPPs) has rarely been reported in fungi, even (Fig. 1A). though organisms of this kingdom have a long history as a prolific Early isotopic labeling studies showed that Ile, Pro, and Phe were source of natural products. Here we report an investigation of the all incorporated into the phomopsin scaffold (24). Because a Phe phomopsins, antimitotic mycotoxins. We show that phomopsin is a hydroxylase that can convert Phe to Tyr has not been found in fungal RiPP and demonstrate the widespread presence of a path- Ascomycetes, the labeling study seems incongruent with a ribosomal way for the biosynthesis of a family of fungal cyclic RiPPs, which we route to phomopsins, in which Tyr, not Phe, would need to be in- term dikaritins. We characterize PhomM as an S-adenosylmethionine– corporated into the phomopsin structure via a tRNA-dependent dependent α-N-methyltransferase that converts phomopsin A to pathway. Here we report our investigation of the biosynthetic path- an N,N-dimethylated congener (phomopsin E), and show that the way of phomopsins, which explains the paradoxical observations in methyltransferases involved in dikaritin biosynthesis have evolved the early labeling studies and unequivocally demonstrates that pho- differently and likely have broad substrate specificities. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Relating Metatranscriptomic Profiles to the Micropollutant
1 Relating Metatranscriptomic Profiles to the 2 Micropollutant Biotransformation Potential of 3 Complex Microbial Communities 4 5 Supporting Information 6 7 Stefan Achermann,1,2 Cresten B. Mansfeldt,1 Marcel Müller,1,3 David R. Johnson,1 Kathrin 8 Fenner*,1,2,4 9 1Eawag, Swiss Federal Institute of Aquatic Science and Technology, 8600 Dübendorf, 10 Switzerland. 2Institute of Biogeochemistry and Pollutant Dynamics, ETH Zürich, 8092 11 Zürich, Switzerland. 3Institute of Atmospheric and Climate Science, ETH Zürich, 8092 12 Zürich, Switzerland. 4Department of Chemistry, University of Zürich, 8057 Zürich, 13 Switzerland. 14 *Corresponding author (email: [email protected] ) 15 S.A and C.B.M contributed equally to this work. 16 17 18 19 20 21 This supporting information (SI) is organized in 4 sections (S1-S4) with a total of 10 pages and 22 comprises 7 figures (Figure S1-S7) and 4 tables (Table S1-S4). 23 24 25 S1 26 S1 Data normalization 27 28 29 30 Figure S1. Relative fractions of gene transcripts originating from eukaryotes and bacteria. 31 32 33 Table S1. Relative standard deviation (RSD) for commonly used reference genes across all 34 samples (n=12). EC number mean fraction bacteria (%) RSD (%) RSD bacteria (%) RSD eukaryotes (%) 2.7.7.6 (RNAP) 80 16 6 nda 5.99.1.2 (DNA topoisomerase) 90 11 9 nda 5.99.1.3 (DNA gyrase) 92 16 10 nda 1.2.1.12 (GAPDH) 37 39 6 32 35 and indicates not determined. 36 37 38 39 S2 40 S2 Nitrile hydration 41 42 43 44 Figure S2: Pearson correlation coefficients r for rate constants of bromoxynil and acetamiprid with 45 gene transcripts of ECs describing nucleophilic reactions of water with nitriles. -

Can Hyperuricemia Predict Glycogen Storage Disease (Mcardle's Disease) in Rheumatology Practice? (Myogenic Hyperuricemia)
Clinical Rheumatology (2019) 38:2941–2948 https://doi.org/10.1007/s10067-019-04572-8 CASE BASED REVIEW Can hyperuricemia predict glycogen storage disease (McArdle’s disease) in rheumatology practice? (Myogenic hyperuricemia) Döndü Üsküdar Cansu1 & Bahattin Erdoğan2 & Cengiz Korkmaz1 Received: 25 March 2019 /Revised: 17 April 2019 /Accepted: 18 April 2019 /Published online: 1 May 2019 # International League of Associations for Rheumatology (ILAR) 2019 Abstract Gout disease is an inflammatory arthritis that arises due to the accumulation of monosodium urate crystals (MSU) around the joints and in tissues. Clinical manifestation of metabolic diseases leading to secondary hyperuricemia most predominantly occurs in the form of gouty arthritis. Hyperuricemia and gout may develop during the course of glycogen storage diseases (GSD), particularly in GSD type I, which involves the liver. On the other hand, during the course of GSD type V (GSDV, McArdle’s disease), which merely affects the muscle tissue due to the deficiency of the enzyme myophosphorylase, hyperuricemia and/or gout is rarely an expected symptom. These patients may mistakenly be diagnosed as having idiopathic hyperuricemia and associated gout, leading to the underlying secondary causes be overlooked and thus, diagnostic delays may occur. In this case report, we present a premenopausal female patient who experienced flare-ups of chronic arthritis while on disease-modifying antirheumatic drugs and intraarticular steroids due to a diagnosis of undifferentiated arthritis. The patient was initially suspected of having gouty arthritis because elevated concentrations of uric acid were incidentally detected, but then, a diagnosis of asymptomatic GSDV was made owing to elevated concentrations of muscle enzymes during colchicine use.