Could Hypoglycemia and Hypoalbuminemia Allow the Identifcation of Septic Patients at High Mortality Risk in Addition of Clinical Scores?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetically Determined Hypoalbuminemia As a Risk Factor for Hypertension: Instrumental Variable Analysis Jong Wook Choi1, Joon‑Sung Park2* & Chang Hwa Lee2*
www.nature.com/scientificreports OPEN Genetically determined hypoalbuminemia as a risk factor for hypertension: instrumental variable analysis Jong Wook Choi1, Joon‑Sung Park2* & Chang Hwa Lee2* Hypoalbuminemia is associated with vascular endothelial dysfunction and the development of chronic cardiovascular diseases. However, the relationship between serum albumin concentration and blood pressure changes remains controversial. Community‑based longitudinal cohort data collected from Korean Genome and Epidemiology Study were used in this study. Hypoalbuminemia was defned as a serum albumin concentration of ≤ 4.0 g/dL. A total of 4325 participants were categorized into control (n = 3157) and hypoalbuminemia (n = 1168) groups. Serum albumin had a non‑linear relationship with the risk of hypertension development. A genome‑wide association study revealed 71 susceptibility loci associated with hypoalbuminemia. Among susceptibility loci, genetic variations at rs2894536 in LOC107986598 and rs10972486 in ATP8B5P were related to elevated blood pressure. Serum albumin (HR = 0.654, 95% CI 0.521–0.820) and polymorphisms of rs2894536 (HR = 1.176, 95% CI 1.015–1.361) and rs10972486 (HR = 1.152, 95% CI 1.009–1.316) were signifcant predictors of hypertension development. Increased albumin concentration instrumented by 2 hypoalbuminemia‑associated SNPs (rs2894536 and rs10972486) was associated with decreased HRs for hypertension development (HR = 0.762, 95% CI 0.659–0.882 and HR = 0.759, 95% CI 0.656–0.878). Our study demonstrated that genetically determined hypoalbuminemia is a signifcant predictor of incipient hypertension. Albumin, one of the major serum proteins, has multiple important physiological functions involving stabilization of plasma colloid osmotic pressure, transportation of diverse substances, and signifcant antioxidant activity, and its concentration is fnely regulated by various systems in the physiologic state 1. -
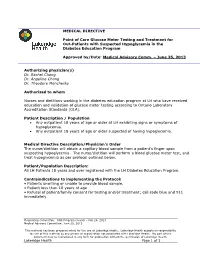
MEDICAL DIRECTIVE Point of Care Glucose Meter Testing And
MEDICAL DIRECTIVE Point of Care Glucose Meter Testing and Treatment for Out-Patients with Suspected Hypoglycemia in the Diabetes Education Program Approved by/Date: Medical Advisory Comm. – June 25, 2013 Authorizing physician(s) Dr. Rachel Chong Dr. Angeline Chong Dr. Theodore Monchesky Authorized to whom Nurses and dietitians working in the diabetes education program at LH who have received education and validation of glucose meter testing according to Ontario Laboratory Accreditation Standards (OLA). Patient Description / Population Any outpatient 18 years of age or older at LH exhibiting signs or symptoms of hypoglycemia. Any outpatient 18 years of age or older suspected of having hypoglycemia. Medical Directive Description/Physician’s Order The nurse/dietitian will obtain a capillary blood sample from a patient’s finger upon suspecting hypoglycemia. The nurse/dietitian will perform a blood glucose meter test, and treat hypoglycemia as per protocol outlined below. Patient/Population Description: All LH Patients 18 years and over registered with the LH Diabetes Education Program. Contraindications to implementing the Protocol: • Patients unwilling or unable to provide blood sample. • Patient less than 18 years of age • Refusal of patient/family consent for testing and/or treatment; call code blue and 911 immediately Originating Committee: RNS Program Council – Feb 26, 2013 Medical Advisory Committee: June 25, 2013 This material has been prepared solely for the use at Lakeridge Health. Lakeridge Health accepts no responsibility for use of this material by any person or organization not associated with Lakeridge Health. No part of this document may be reproduced in any form for publication without the permission of Lakeridge Health. -

Diabetes Control in Thyroid Disease
In Brief Thyroid disease is commonly found in most types of diabetes. This article defines the prevalence of thyroid disease in diabetes and elucidates through case studies the assessment, diagnosis, and clinical management of thyroid disease in diabetes. Diabetes Control in Thyroid Disease Thyroid disease is a pathological state abnormality. Several studies, including that can adversely affect diabetes con- the Colorado study, have documented trol and has the potential to negative- a higher prevalence of thyroid disease Jennal L. Johnson, MS, RNC, FNP, ly affect patient outcomes. Thyroid in women, with prevalence rates rang- BC-ADM, CDE disease is found commonly in most ing from 4 to 21%, whereas the rate in forms of diabetes and is associated men ranges from 2.8 to 16%.1 with advanced age, particularly in Thyroid disease increases with age. In type 2 diabetes and underlying the Colorado study, the 18-year-olds autoimmune disease in type 1 dia- had a prevalence rate of 3.5% com- betes. This article defines the preva- pared with a rate of 18.5% for those lence of thyroid disease in diabetes, ≥ 65 years of age. discusses normal physiology and The prevalence of thyroid disease in screening recommendations for thy- diabetes has been estimated at 10.8%,2 roid disease, and elucidates through with the majority of cases occurring as case studies the assessment, diagnosis, hypothyroidism (~ 30%) and subclini- and clinical management of thyroid cal hypothyroidism (~ 50%).2 Hyper- disease and its impact on diabetes. thyroidism accounts for 12%, and postpartum thyroiditis accounts for Thyroid Disease Prevalence 11%.2 Of the female patients with The prevalence of thyroid disease in type 1 diabetes, 30% have thyroid dis- the general population is estimated to ease, with a rate of postpartum thy- be 6.6%, with hypothyroidism the roid disease three times that of the most common malady.1 Participants normal population. -

Glycated Hemoglobin and Glycated Albumin in Patients with Diabetes
Kitajima et al. Renal Replacement Therapy (2020) 6:10 https://doi.org/10.1186/s41100-020-0260-5 RESEARCH Open Access Glycated hemoglobin and glycated albumin in patients with diabetes undergoing hemodiafiltration Yukie Kitajima1*, Shunichiro Urabe2, Takashi Hosono2, Satoshi Yoshikawa3, Yuzuru Sato3 and Toru Hyodo2 Abstract Background: Online hemodiafiltration (OHDF), which results in high albumin leakage, is now widely used in Japan for dialysis, since the national insurance system began reimbursing its costs in 2012. Glycated albumin (GA) levels are affected by albumin leakage into effluent dialysate fluid. Therefore, GA levels in patients requiring diabetes- related dialysis undergoing OHDF require monitoring. However, there have been no previous reports on glycemic control indicators of patients with diabetes undergoing OHDF. We aimed to develop a glycemic control index for patients requiring diabetes-related dialysis undergoing OHDF. Methods: This study comprised 133 diabetic patients undergoing OHDF. We examined the correlation between GA and glycated hemoglobin (HbA1c) levels. We analyzed effluent dialysate fluid samples from 41 patients classified into 3 groups, namely, group A, non-protein-leaking OHDF (n = 20); group B, protein-leaking OHDF (n = 14); and group C, highly efficient protein-leaking OHDF (n = 7). We examined the association between GA and HbA1c levels in each group and among patients. Results: A significant positive correlation was observed between GA and HbA1c levels (r = 0.562, p < 0.0001). There was no significant correlation between pre-dialysis blood glucose levels and HbA1c or GA levels as observed on regular blood tests performed under non-fasting conditions. Patients were classified into 2 groups based on their mean albumin levels (3.4 g/dL cutoff). -

Refractory Hypoglycemia in T-Cell Lymphoma
Open Access Austin Oncology Case Reports Case Report Refractory Hypoglycemia in T-Cell Lymphoma Buyukaydina B1*, Tunca M1, Alayb M2, Kazanciogluc R3 and Reha E3 Abstract 1Bezmialem Vakif University, Department of Internal Hypoglycemia is commonly seen in diabetes mellitus patients; whereas it Medicine, Turkey is rarely seen in a healthy person. In this case, we reported a male patient 2Yuzuncu Yil University, Department of Endocrinology, with a treatment-resistant hypoglycemia. A 53 years old male patient admitted Turkey to our clinic with debility, nausea and vomiting. Physical examination revealed 3Bezmialem Vakif University, Department of Nephology, lymphadenopathies in the left axilla and inguinal regions; and presence of right Turkey upper quadrant tenderness. Biochemical results revealed severe hypoglycemia, *Corresponding author: Banu Buyukaydin, azotemia and elevation of liver enzymes. Histological result of the excisional Bezmialem Vakif University, Department of Internal lymph node biopsy was compatible with peripheral T cell lymphoma. In ward, Medicine, Turkey the patient has repeated recurrent hypoglycemia, which did not resolve with all treatment given. His general condition deteriorated and he died due to sepsis. Received: June 01, 2016; Accepted: July 10, 2016; This case highlighted the need to rule out hematologic malignancies; precisely Published: July 13, 2016 T-cell lymphoma in a patient who presented with resistant hypoglycemia in the presence of lymphadenopathy. Keywords: Hypoglycemia, Lymphoma, IGF-II Introduction approximately fifty percent of proliferation index. CD3 was positive. This finding was compatible to histological diagnosis of peripheral Hypoglycemia is defined as the occurrence of a variety of T-cell lymphoma with partial involvement of lymph ganglia. symptoms in association with plasma glucose concentration of 50mg/dl or less. -

CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E
Peer Reviewed PRACTICAL ONCOLOGY CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E. Burgess, DVM, Diplomate ACVIM (Oncology) Tufts University An insulinoma is a malignant pancreatic tumor that DIAGNOSIS inappropriately secretes excessive insulin, resulting in Aside from a histologic confirmation of insulinoma, profound hypoglycemia.1 no currently available diagnostic test provides a de- Pancreatic tumors are classified as: finitive diagnosis of insulinoma. Existing techniques • Exocrine, which includes adenocarcinomas of may help increase suspicion for an insulin-secreting ductular or acinar origin tumor but, with most diagnostic testing, it is im- • Endocrine, which arise from the islets of perative to interpret all results in the context of the Langerhans. coexisting clinical signs. Insulinomas are functional neuroendocrine tumors that originate in the beta cells of the islets Differential Diagnosis of Langerhans.1 A complete work-up, including careful patient history, physical examination, bloodwork, and PRESENTATION diagnostic imaging tests, should be performed to Signalment rule out other causes of hypoglycemia, such as Any breed of dog can be affected, but large sepsis, hepatic failure, adrenal cortical insufficiency, breeds tend to be overrepresented.1 While, in toxin ingestion, and other forms of neoplasia. humans, insulinomas affect females far more frequently than males, there is no apparent sex Laboratory Tests predilection in dogs.1-3 Dogs also commonly Blood Glucose present with a malignant variant, while humans A simple fasting blood glucose level of less than often have a benign adenoma (80%).1 Insulino- 40 mg/dL can suggest hyperinsulinemia, although ma is rare in cats.4 careful monitoring of a fasted dog with suspected insulinoma is strongly recommended due to high Clinical Signs risk for seizure activity. -

Clinical and Histopathological Features of Renal Maldevelopment in Boxer Dogs: a Retrospective Case Series (1999–2018) †
animals Article Clinical and Histopathological Features of Renal Maldevelopment in Boxer Dogs: A Retrospective Case Series (1999–2018) † Maria Alfonsa Cavalera 1, Floriana Gernone 1, Annamaria Uva 1, Paola D’Ippolito 2, Xavier Roura 3 and Andrea Zatelli 1,* 1 Department of Veterinary Medicine, University of Bari, 70010 Valenzano, Italy; [email protected] (M.A.C.); fl[email protected] (F.G.); [email protected] (A.U.) 2 Veterinary diagnostic Lab ACV Triggiano, 70019 Triggiano, Italy; [email protected] 3 Hospital Clínic Veterinari, Universitat Autònoma de Barcelona, 08193 Bellaterra, Spain; [email protected] * Correspondence: [email protected]; Tel.: +39-080-4679804 † This study was partially presented as oral communication at the 11th ECVIM-CA/ESVIM Congress, Dublin (Ireland) as “Congenital nephrotic syndrome with renal glomerular immaturity in 7 Boxer dogs”. Zatelli, A., Domenech, O., Bussadori, C., Lubas, G., Del Piero, F. Simple Summary: This study describes clinical findings in Boxer dogs with renal maldevelopment and proposes a possible mode of inheritance. Medical records of 9 female Boxer dogs, older than 5 months and with a clinical diagnosis of proteinuric chronic kidney disease prior to one year of age, showed the presence of polyuria and polydipsia, decreased appetite, weight loss, lethargy and weakness in all affected dogs. Common laboratory findings were proteinuria and diluted urine, non- regenerative anemia, azotemia, hyperphosphatemia, hypoalbuminemia and hypercholesterolemia. Citation: Cavalera, M.A.; Gernone, Histopathology of the kidneys identified the presence of immature glomeruli in all dogs. In 7 out F.; Uva, A.; D’Ippolito, P.; Roura, X.; of 9 related dogs, the pedigree analysis showed that a simple autosomal recessive trait may be a Zatelli, A. -

Hypoglycemia, Hepatic Dysfunction, Muscle Weakness, Cardiomyopathy
Pediatr. Res. 17: 319-326 (1983) Hypoglycemia, Hepatic Dysfunction, Muscle Weakness, Cardiomyopathy, Free Carnitine Deficiency and Long-Chain Acylcarnitine Excess Responsive to Medium Chain Triglyceride Diet ALLEN M. GLASGOW,'~~'ANDREW G. ENGEL, DENNIS M. BIER, LOWELL W. PERRY, MARY DICKIE, JANE TODARO, BARBARA I. BROWN, AND MERTON F. UTTER Departments of Endocrinology and Metabolism [A.M.G.], Gastroenterology [J. TI, Cardiology [L. W.P.] and Dietary [M.B.], Children's Hospital National Medical Center, Washington, D.C.; Department of Neurology, and the Neuromuscular Research Laboratory [A. G.E.], Mayo Clinic and Mayo Foundation, Rochester, Minnesota USA; Departments of Medicine and Pediatrics [D. M. B.] and Biochemistry [B. I. B.], Washington University, School of Medicine, St. Louis, Missouri, USA; and Department of Biochemistry [MI U.],Case Western Reserve, Cleveland, Ohio, USA Summary Hepatic long-chain acyl CoA carnitine transferase deficiency (4), multiple acyl CoA dehydrogenase deficiency (glutaric aciduria Fraternal twins who had fasting hypoglycemia, hypoketonemia, type 11) (18), and systemic carnitine deficiency (3,9, 12, 17, 24, 37, muscle weakness, and hepatic dysfunction are reported. The he- 43), all of which are associated with impaired fatty acid oxidation, patic dysfunction occurred only during periods of caloric depriva- have hypoglycemia as a major clinical manifestation. tion. The surviving patient developed a cardiomyopathy. In this The purpose of this paper is twofold: (1) to report fraternal sibling, muscle weakness and cardiomyopathy were markedly im- proved by a diet high in medium chain triglycerides. There was a twins with free carnitine deficiency and long-chain acylcarnitine marked deficiency of muscle total carnitine and a mild deficiency excess in whom hypoglycemia, hepatic dysfunction, muscle weak- of hepatic total carnitine. -

Increasing Ferritin Predicts Early Death in Adult Hemophagocytic Lymphohistiocytosis
Henry Ford Health System Henry Ford Health System Scholarly Commons Pathology Articles Pathology 2-17-2021 Increasing ferritin predicts early death in adult hemophagocytic lymphohistiocytosis Rand Abou Shaar Charles S. Eby Suzanne van Dorp Theo de Witte Zaher K. Otrock Follow this and additional works at: https://scholarlycommons.henryford.com/pathology_articles Received: 13 November 2020 | Accepted: 29 January 2021 DOI: 10.1111/ijlh.13489 ORIGINAL ARTICLE Increasing ferritin predicts early death in adult hemophagocytic lymphohistiocytosis Rand Abou Shaar1 | Charles S. Eby2 | Suzanne van Dorp3 | Theo de Witte3 | Zaher K. Otrock1 1Department of Pathology and Laboratory Medicine, Henry Ford Hospital, Detroit, MI, Abstract USA Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare syndrome of 2 Department of Pathology and Immunology, pathologic immune activation. Most studies on adult HLH have evaluated prognostic Washington University School of Medicine, St. Louis, MO, USA factors for overall survival; factors predicting early mortality have not been suffi- 3Radboud University Medical Center, ciently investigated. Nijmegen, Netherlands Methods: This was a collaborative study between Henry Ford Hospital and Barnes- Correspondence Jewish Hospital. We identified all adult HLH patients with at least 2 ferritin levels Zaher K. Otrock, Transfusion Medicine Division, Department of Pathology and within 30 days from admission. Laboratory Medicine, Henry Ford Hospital, Results: One- hundred twenty- four patients were identified. There were -

National Coverage Determination Procedure Code: 82977 Gamma Glutamyl Transferase CMS Policy Number: 190.32 Back to NCD List
National Coverage Determination Procedure Code: 82977 Gamma Glutamyl Transferase CMS Policy Number: 190.32 Back to NCD List Description: Gamma glutamyl transferase (GGT) is an intracellular enzyme that appears in blood following leakage from cells. Renal tubules, liver, and pancreas contain high amounts, although the measurement of GGT in serum is almost always used for assessment of Hepatobiliary function. Unlike other enzymes which are found in heart, skeletal muscle, and intestinal mucosa as well as liver, the appearance of an elevated level of GGT in serum is almost always the result of liver disease or injury. It is specifically useful to differentiate elevated alkaline phosphatase levels when the source of the alkaline phosphatase increase (bone, liver, or placenta) is unclear. The combination of high alkaline phosphatase and a normal GGT does not, however, rule out liver disease completely. As well as being a very specific marker of Hepatobiliary function, GGT is also a very sensitive marker for hepatocellular damage. Abnormal concentrations typically appear before elevations of other liver enzymes or biliuria are evident. Obstruction of the biliary tract, viral infection (e.g., hepatitis, mononucleosis), metastatic cancer, exposure to hepatotoxins (e.g., organic solvents, drugs, alcohol), and use of drugs that induce microsomal enzymes in the liver (e.g., cimetidine, barbiturates, phenytoin, and carbamazepine) all can cause a moderate to marked increase in GGT serum concentration. In addition, some drugs can cause or exacerbate liver dysfunction (e.g., atorvastatin, troglitazone, and others as noted in FDA Contraindications and Warnings.) GGT is useful for diagnosis of liver disease or injury, exclusion of hepatobiliary involvement related to other diseases, and patient management during the resolution of existing disease or following injury. -

Hypoalbuminemia at Admission Predicts the Development of Acute Kidney Injury in Hospitalized Patients: a Retrospective Cohort Study
RESEARCH ARTICLE Hypoalbuminemia at admission predicts the development of acute kidney injury in hospitalized patients: A retrospective cohort study Mi-yeon Yu1, Sung Woo Lee2, Seon Ha Baek3, Ki Young Na4, Dong-Wan Chae4, Ho Jun Chin4, Sejoong Kim4* 1 Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea, 2 Department of a1111111111 Internal Medicine, Eulji General Hospital, Seoul, Korea, 3 Department of Internal Medicine, Hallym University Dongtan Sacred Heart Hospital, Gyeonggi-do, Korea, 4 Department of Internal Medicine, Seoul National a1111111111 University Bundang Hospital, Seongnam, Korea a1111111111 a1111111111 * [email protected] a1111111111 Abstract OPEN ACCESS Citation: Yu M-y, Lee SW, Baek SH, Na KY, Chae D-W, Chin HJ, et al. (2017) Hypoalbuminemia at Background admission predicts the development of acute Development of acute kidney injury (AKI) is common and is associated with poor outcomes. kidney injury in hospitalized patients: A We aimed to determine whether hypoalbuminemia (HA) at admission could be a risk factor retrospective cohort study. PLoS ONE 12(7): e0180750. https://doi.org/10.1371/journal. for the development of AKI and mortality in hospitalized patients. pone.0180750 Editor: Emmanuel A. Burdmann, University of Sao Paulo Medical School, BRAZIL Methods Received: March 14, 2017 We enrolled patients who were admitted to Seoul National University Bundang Hospital Accepted: June 20, 2017 from January 2013 to December 2013. HA at admission was defined as a serum albumin Published: July 19, 2017 level < 3.4 mg/dL measured within two days after admission. AKI was defined as an increase in the serum creatinine level by 0.3 mg/dL or 1.5 times of the baseline value Copyright: © 2017 Yu et al. -

Can Hyperuricemia Predict Glycogen Storage Disease (Mcardle's Disease) in Rheumatology Practice? (Myogenic Hyperuricemia)
Clinical Rheumatology (2019) 38:2941–2948 https://doi.org/10.1007/s10067-019-04572-8 CASE BASED REVIEW Can hyperuricemia predict glycogen storage disease (McArdle’s disease) in rheumatology practice? (Myogenic hyperuricemia) Döndü Üsküdar Cansu1 & Bahattin Erdoğan2 & Cengiz Korkmaz1 Received: 25 March 2019 /Revised: 17 April 2019 /Accepted: 18 April 2019 /Published online: 1 May 2019 # International League of Associations for Rheumatology (ILAR) 2019 Abstract Gout disease is an inflammatory arthritis that arises due to the accumulation of monosodium urate crystals (MSU) around the joints and in tissues. Clinical manifestation of metabolic diseases leading to secondary hyperuricemia most predominantly occurs in the form of gouty arthritis. Hyperuricemia and gout may develop during the course of glycogen storage diseases (GSD), particularly in GSD type I, which involves the liver. On the other hand, during the course of GSD type V (GSDV, McArdle’s disease), which merely affects the muscle tissue due to the deficiency of the enzyme myophosphorylase, hyperuricemia and/or gout is rarely an expected symptom. These patients may mistakenly be diagnosed as having idiopathic hyperuricemia and associated gout, leading to the underlying secondary causes be overlooked and thus, diagnostic delays may occur. In this case report, we present a premenopausal female patient who experienced flare-ups of chronic arthritis while on disease-modifying antirheumatic drugs and intraarticular steroids due to a diagnosis of undifferentiated arthritis. The patient was initially suspected of having gouty arthritis because elevated concentrations of uric acid were incidentally detected, but then, a diagnosis of asymptomatic GSDV was made owing to elevated concentrations of muscle enzymes during colchicine use.