Zimbabwe Country Operational Plan 2018 Strategic Direction Summary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Midlands Province Mobile Voter Registration Centres
Midlands Province Mobile Voter Registration Centres Chirumhanzu District Team 1 Ward Centre Dates 18 Mwire primary school 10/06/13-11/06/13 18 Tokwe 4 clinic 12/06/13-13/06/13 18 Chingegomo primary school 14/06/13-15/06/13 16 Chishuku Seondary school 16/06/13-18/06/13 9 Upfumba Secondary school 19/06/13-21/06/13 3 Mutya primary school 22/06/13-24/06/13 2 Gonawapotera secondary school 25/06/13-27/06/13 20 Wildegroove primary school 28/06/13-29/06/13 15 Kushinga primary school 30/06/13-02/07/13 12 Huchu compound 03/07/13-04/-07/13 12 Central estates HQ 5/7/13 20 Mtao/Fair Field compound 6/7/13 12 Chiudza homestead 07/07/13-08/06/13 14 Njerere primary school 9/7/13 Team 2 Ward Centre Dates 22 Hillview Secondary school 10/07/13-12/07/13 17 Lalapanzi Secondary school 13/07/13-15/07/13 16 Makuti homestead 16/06/13-17/06/13 1 Mapiravana Secondary school 18/06/13-19/06/13 9 Siyahukwe Secondary school 20/06/13-23/06/13 4 Chizvinire primary school 24/06/13-25/06/13 21 Mukomberana Seconadry school 26/06/13-29/06/13 20 Union primary school 30/06/13-01/07/13 15 Nyikavanhu primary school 02/07/13-03/07/13 19 Musens primary school 04/07/13-06/07/13 16 Utah primary school 07/7/13-09/07/13 Team 3 Ward Centre Dates 11 Faerdan primary school 10/07/13-11/07/13 11 Chamakanda Secondary school 12/07/13-14/07/13 11 Chamakanda primary school 15/07/13-16/07/13 5 Chizhou Secondary school 17/06/13-16/06/13 3 Chilimanzi primary school 21/06/13-23/06/13 25 Maponda primary school 24/06/13-25/06/13 6 Holy Cross seconadry school 26/06/13-28/06/13 20 New England Secondary -
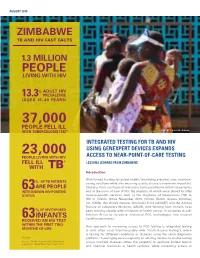
Integrated Testing for TB and HIV Zimbabwe
AUGUST 2019 ZIMBABWE TB AND HIV FAST FACTS 1.3 MILLION PEOPLE LIVING WITH HIV % ADULT HIV 13.3 PREVALENCE (AGES 15–49 YEARS) 37,000 PEOPLE FELL ILL WITH TUBERCULOSIS (TB)* © UNICEF/Costa/Zimbabwe INTEGRATED TESTING FOR TB AND HIV 23,000 USING GENEXPERT DEVICES EXPANDS PEOPLE LIVING WITH HIV ACCESS TO NEAR-POINT-OF-CARE TESTING FELL ILL * LESSONS LEARNED FROM ZIMBABWE WITH TB Introduction With limited funding for global health, identifying practical, cost- and time- OF TB PATIENTS % saving solutions while also ensuring quality of care is evermore important. 63ARE PEOPLE Globally, there are fleets of molecular testing platforms within laboratories WITH KNOWN HIV-POSITIVE and at the point of care (POC), the majority of which were placed to offer STATUS disease-specific services such as the diagnosis of tuberculosis (TB) or HIV in infants. Since November 2015, Clinton Health Access Initiative, Inc. (CHAI), the United Nations Children’s Fund (UNICEF) and the African Society of Laboratory Medicine (ASLM), with funding from Unitaid, have % OF HIV-EXPOSED been working closely with ministries of health across 10 countries in sub- Saharan Africa to introduce innovative POC technologies into national INFANTS 1 63 health programmes. RECEIVED AN HIV TEST WITHIN THE FIRST TWO One approach to increasing access to POC testing is integrated testing MONTHS OF LIFE (a term often used interchangeably with “multi-disease testing”), which is testing for different conditions or diseases using the same diagnostic *Annually platform.2 Leveraging excess capacity on existing devices to enable testing Sources: UNAIDS estimates 2019; World Health across multiple diseases offers the potential to optimize limited human Organization, ‘Global Tuberculosis Report 2018’ and financial resources at health facilities, while increasing access to rapid testing services. -

Mopane Woodlands and the Mopane Worm: Enhancing Rural Livelihoods and Resource Sustainability
Mopane Woodlands and the Mopane Worm: Enhancing rural livelihoods and resource sustainability Final Technical Report Edited by Jaboury Ghazoul1, Division of Biology, Imperial College London Authors and contributors Mopane Tree Management: Dirk Wessels2, Member Mushongohande3, Martin Potgeiter7 Domestication Strategies: Alan Gardiner4, Jaboury Ghazoul Kgetsie ya Tsie Case Study: John Pearce5 Livelihoods and Marketing: Jayne Stack6, Peter Frost7, Witness Kozanayi3, Tendai Gondo3, Nyarai Kurebgaseka8, Andrew Dorward9, Nigel Poole5 New Technologies: Frank Taylor10, Alan Gardiner Choice experiments: Robert Hope11, Witness Kozanayi, Tendai Gondo Mopane worm diseases: Robert Knell12 Start and End Date 1 May 2001 – 31 January 2006 DFID Project Reference Number R 7822 Research Programme Forestry Research Programme (FRP) Research Production System Forest Agriculture Interface 1 Also ETH Zürich, Department of Environmental Sciences, ETH Zentrum CHN, Universitätstrasse 16, Zürich 8092, Switzerland 2 Department of Botany, university fo the North, South Africa 3 Forest Commission, Harare, Zimbabwe 4 Veld Products Research and Development, Gabarone, and Division of Biology, Imperial College London 5 Kgetsie ya Tsie, Tswapong Hills, Botswana 6 Imperial College London and University of Zimbabwe, Project Co-ordinator 7 Institute of Environmental Studies 8 Southern Alliance for Indigenous Resources 9 Imperial College London, Centre for Environmental Policy. 10 Veld Products Research and Development 11 University of Newcastle 12 Queen Mary College, University of London 1 Contents Executive Summary 3 Background 3 Project Purpose 6 Research Activities Section 1. Mopane tree ecology and management 7 Section 2.1 Mopane worm productivity and domestication 18 Section 2.2 Mini-livestock: Rural Mopane Worm Farming at the Household Level 34 Section 3. A case study of the Kgetsie ya Tsie community enterprise model for managing and trading mopane worms 59 Section 4. -

Malaria Outbreak Investigation in a Rural Area South of Zimbabwe: a Case–Control Study Paddington T
Mundagowa and Chimberengwa Malar J (2020) 19:197 https://doi.org/10.1186/s12936-020-03270-0 Malaria Journal RESEARCH Open Access Malaria outbreak investigation in a rural area south of Zimbabwe: a case–control study Paddington T. Mundagowa1* and Pugie T. Chimberengwa2 Abstract Background: Ninety percent of the global annual malaria mortality cases emanate from the African region. About 80–90% of malaria transmissions in sub-Saharan Africa occur indoors during the night. In Zimbabwe, 79% of the population are at risk of contracting the disease. Although the country has made signifcant progress towards malaria elimination, isolated seasonal outbreaks persistently resurface. In 2017, Beitbridge District was experiencing a second malaria outbreak within 12 months prompting the need for investigating the outbreak. Methods: An unmatched 1:1 case–control study was conducted to establish the risk factors associated with con- tracting malaria in Ward 6 of Beitbridge District from week 36 to week 44 of 2017. The sample size constituted of 75 randomly selected cases and 75 purposively selected controls. Data were collected using an interviewer-administered questionnaire and Epi Info version 7.2.1.0 was used to conduct descriptive, bivariate and multivariate analyses of the factors associated with contracting malaria. Results: Fifty-two percent of the cases were females and the mean age of cases was 29 13 years. Cases were diag- nosed using rapid diagnostic tests. Sleeping in a house with open eaves (OR: 2.97; 95% CI± 1.44–6.16; p < 0.01), spend- ing the evenings outdoors (OR: 2.24; 95% CI 1.04–4.85; p 0.037) and sleeping in a poorly constructed house (OR: 4.33; 95% CI 1.97–9.51; p < 0.01) were signifcantly associated= with contracting malaria while closing eaves was protec- tive (OR: 0.45; 95% CI 0.20–1.02; p 0.055). -

Bulawayo City Mpilo Central Hospital
Province District Name of Site Bulawayo Bulawayo City E. F. Watson Clinic Bulawayo Bulawayo City Mpilo Central Hospital Bulawayo Bulawayo City Nkulumane Clinic Bulawayo Bulawayo City United Bulawayo Hospital Manicaland Buhera Birchenough Bridge Hospital Manicaland Buhera Murambinda Mission Hospital Manicaland Chipinge Chipinge District Hospital Manicaland Makoni Rusape District Hospital Manicaland Mutare Mutare Provincial Hospital Manicaland Mutasa Bonda Mission Hospital Manicaland Mutasa Hauna District Hospital Harare Chitungwiza Chitungwiza Central Hospital Harare Chitungwiza CITIMED Clinic Masvingo Chiredzi Chikombedzi Mission Hospital Masvingo Chiredzi Chiredzi District Hospital Masvingo Chivi Chivi District Hospital Masvingo Gutu Chimombe Rural Hospital Masvingo Gutu Chinyika Rural Hospital Masvingo Gutu Chitando Rural Health Centre Masvingo Gutu Gutu Mission Hospital Masvingo Gutu Gutu Rural Hospital Masvingo Gutu Mukaro Mission Hospital Masvingo Masvingo Masvingo Provincial Hospital Masvingo Masvingo Morgenster Mission Hospital Masvingo Mwenezi Matibi Mission Hospital Masvingo Mwenezi Neshuro District Hospital Masvingo Zaka Musiso Mission Hospital Masvingo Zaka Ndanga District Hospital Matabeleland South Beitbridge Beitbridge District Hospital Matabeleland South Gwanda Gwanda Provincial Hospital Matabeleland South Insiza Filabusi District Hospital Matabeleland South Mangwe Plumtree District Hospital Matabeleland South Mangwe St Annes Mission Hospital (Brunapeg) Matabeleland South Matobo Maphisa District Hospital Matabeleland South Umzingwane Esigodini District Hospital Midlands Gokwe South Gokwe South District Hospital Midlands Gweru Gweru Provincial Hospital Midlands Kwekwe Kwekwe General Hospital Midlands Kwekwe Silobela District Hospital Midlands Mberengwa Mberengwa District Hospital . -

PLAAS RR46 Smeadzim 1.Pdf
Chrispen Sukume, Blasio Mavedzenge, Felix Murimbarima and Ian Scoones Faculty of Economic and Management Sciences Research Report 46 Space, Markets and Employment in Agricultural Development: Zimbabwe Country Report Chrispen Sukume, Blasio Mavedzenge, Felix Murimbarima and Ian Scoones Published by the Institute for Poverty, Land and Agrarian Studies, Faculty of Economic and Management Sciences, University of the Western Cape, Private Bag X17, Bellville 7535, Cape Town, South Africa Tel: +27 21 959 3733 Fax: +27 21 959 3732 Email: [email protected] Institute for Poverty, Land and Agrarian Studies Research Report no. 46 June 2015 All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means without prior permission from the publisher or the authors. Copy Editor: Vaun Cornell Series Editor: Rebecca Pointer Photographs: Pamela Ngwenya Typeset in Frutiger Thanks to the UK’s Department for International Development (DfID) and the Economic and Social Research Council’s (ESRC) Growth Research Programme Contents List of tables ................................................................................................................ ii List of figures .............................................................................................................. iii Acronyms and abbreviations ...................................................................................... v 1 Introduction ........................................................................................................ -

Promotion of Climate-Resilient Lifestyles Among Rural Families in Gutu
Promotion of climate-resilient lifestyles among rural families in Gutu (Masvingo Province), Mutasa (Manicaland Province) and Shamva (Mashonaland Central Province) Districts | Zimbabwe Sahara and Sahel Observatory 26 November 2019 Promotion of climate-resilient lifestyles among rural families in Gutu Project/Programme title: (Masvingo Province), Mutasa (Manicaland Province) and Shamva (Mashonaland Central Province) Districts Country(ies): Zimbabwe National Designated Climate Change Management Department, Ministry of Authority(ies) (NDA): Environment, Water and Climate Development Aid from People to People in Zimbabwe (DAPP Executing Entities: Zimbabwe) Accredited Entity(ies) (AE): Sahara and Sahel Observatory Date of first submission/ 7/19/2019 V.1 version number: Date of current submission/ 11/26/2019 V.2 version number A. Project / Programme Information (max. 1 page) ☒ Project ☒ Public sector A.2. Public or A.1. Project or programme A.3 RFP Not applicable private sector ☐ Programme ☐ Private sector Mitigation: Reduced emissions from: ☐ Energy access and power generation: 0% ☐ Low emission transport: 0% ☐ Buildings, cities and industries and appliances: 0% A.4. Indicate the result ☒ Forestry and land use: 25% areas for the project/programme Adaptation: Increased resilience of: ☒ Most vulnerable people and communities: 25% ☒ Health and well-being, and food and water security: 25% ☐ Infrastructure and built environment: 0% ☒ Ecosystem and ecosystem services: 25% A.5.1. Estimated mitigation impact 399,223 tCO2eq (tCO2eq over project lifespan) A.5.2. Estimated adaptation impact 12,000 direct beneficiaries (number of direct beneficiaries) A.5. Impact potential A.5.3. Estimated adaptation impact 40,000 indirect beneficiaries (number of indirect beneficiaries) A.5.4. Estimated adaptation impact 0.28% of the country’s total population (% of total population) A.6. -
Zimbabwe Annual Budget Review for 2016 and the 2017 Outlook
ZIMBABWE ANNUAL BUDGET REVIEW FOR 2016 AND THE 2017 OUTLOOK Presented to the Parliament of Zimbabwe on Thursday, July 20, 2017 by The Hon. P. A. Chinamasa, M.P. Minister of Finance and Economic Development 1 1 2 FOREWORD In presenting the 2017 National Budget on 8 December 2016, I indicated the need to strengthen the outline of the Budget Statement presentation as an instrument of Budget accountability and fiscal transparency, in the process improving policy engagement and accessibility for a wider range of public and targeted audiences. Accordingly, I presented a streamlined Budget Statement, and advised that extensive economic review material, which historically was presented as part of the National Budget Statement, would now be provided through a new publication called the Annual Budget Review. I am, therefore, pleased to unveil and Table the first Annual Budget Review, beginning with Fiscal Year 2016. This reports on revenue and expenditure outturn for the full fiscal year, 2016. Furthermore, the Annual Budget Review also allows opportunity for reporting on other recent macro-economic developments and the outlook for 2017. As I indicated to Parliament in December 2016, the issuance of the Annual Budget Review, therefore, makes the issuance of the Mid-Term Fiscal Policy Review no longer necessary, save for exceptional circumstances requiring Supplementary Budget proposals. 3 Treasury will, however, continue to provide Quarterly Treasury Bulletins, capturing quarterly macro-economic and fiscal developments, in addition to the Consolidated Monthly Financial Statements published monthly in line with the Public Finance Management Act. This should avail the public with necessary information on relevant economic developments, that way enhancing and supporting their decision making processes, activities and engagement with Government on overall economic policy issues. -

1 Research Application Summary Evaluating the Level of Adoption Of
Research Application Summary Evaluating the level of adoption of improved agrosilvopastoral technologies, factors affecting adoption and establishing the species and systems adopted among small holder farmers of Buhera and Mutasa Districts of Manicaland Province, Zimbabwe Chihota B.P., Mupanda K., Mrema M., Tagwira F. & Ajayi O.C. Background Two thirds of the rural populations in most countries of Sub-Saharan Africa subsist on less than US$1 a day. The farmers’ economies have weak linkages to the markets and they have little or no access to external inputs. The increasing cost of inputs and high transport costs make external inputs unaffordable for the smallholder farmer (Spencer, 2002). Inorganic fertilizer use has declined to 8kg/ha (NEPAD, 2006). Smallholder farmers cannot afford stock feeds for supplementing limited and poor quality pasture during the dry and cold season. Land degradation and siltation are an environmental concern that also reduces yields (Rattsø, 1996). Crop and livestock yields are low and declining. Countries like Zimbabwe, Malawi, Zambia, Mozambique and Botswana are affected and as a result, food insecure (Bohringer, 2002). Some agroforestry technologies have been shown to improve the soil and animal fodder availability (Dzowela, 1994; Govere, 2003). Agroforestry can improve crop and livestock production by providing relatively less costly, more affordable and locally available inputs for fodder and soil amendments to the smallholder farmer. Government departments and non-governmental organizations (NGOs) like World Agroforestry Centre (WAC) are scaling up agroforestry through training and distributing germplasm to the smallholder farmers in the region. Not much has been done on assessment of adoption and factors that affect adoption of agroforestry in different geographical areas and agricultural sectors in Zimbabwe. -

Tendayi Mutimukuru-Maravanyika Phd Thesis
Can We Learn Our Way to Sustainable Management? Adaptive Collaborative Management in Mafungautsi State Forest, Zimbabwe. Tendayi Mutimukuru-Maravanyika Thesis committee Thesis supervisors Prof. dr. P. Richards Professor of Technology and Agrarian Development Wageningen University Prof. dr. K.E. Giller Professor of Plant Production Systems Wageningen University Thesis co-supervisor Dr. ir. C. J. M. Almekinders Assistant Professor, Technology and Agrarian Development Group Wageningen University Other members Prof. dr. ir. C. Leeuwis, Wageningen University Prof. dr. L.E. Visser, Wageningen University Dr. ir. K. F. Wiersum, Wageningen University Dr. B.B. Mukamuri, University of Zimbabwe This research was conducted under the auspices of the CERES Research School for Resource Studies for Development. Can We Learn Our Way to Sustainable Management? Adaptive Collaborative Management in Mafungautsi State Forest, Zimbabwe. Tendayi Mutimukuru-Maravanyika Thesis submitted in fulfilment of the requirements for the degree of doctor at Wageningen University by the authority of the Rector Magnificus Prof. dr. M. J. Kropff in the presence of the Thesis Committee appointed by the Academic Board to be defended in public on Friday 23 April 2010 at 11 a.m. in the Aula. Tendayi Mutimukuru-Maravanyika Can We Learn Our Way to Sustainable Management? Adaptive Collaborative Management in Mafungautsi State Forest, Zimbabwe. 231 pages Thesis Wageningen University, Wageningen, NL (2010) ISBN 978-90-8585-651-1 Dedication To my parents, my husband Simeon , my son Tafadzwa -

Zimbabwe-HIV-Estimates Report 2018
ZIMBABWE NATIONAL AND SUB-NATIONAL HIV ESTIMATES REPORT 2017 AIDS & TB PROGRAMME MINISTRY OF HEALTH AND CHILD CARE July 2018 Foreword The Ministry of Health and Child Care (MOHCC) in collaboration with National AIDS Council (NAC) and support from partners, produced the Zimbabwe 2017 National, Provincial and District HIV and AIDS Estimates. The UNAIDS, Avenir Health and NAC continued to provide technical assistance and training in order to build national capacity to produce sub-national estimates in order to track the epidemic. The 2017 Estimates report gives estimates for the impact of the programme. It provide an update of the HIV and AIDS estimates and projections, which include HIV prevalence and incidence, programme coverages, AIDS-related deaths and orphans, pregnant women in need of PMTCT services in the country based on the Spectrum Model version 5.63. The 2017 Estimates report will assist the country to monitor progress towards the fast track targets by outlining programme coverage and possible gaps. This report will assist programme managers in accounting for efforts in the national response and policy makers in planning and resource mobilization. Brigadier General (Dr.) G. Gwinji Permanent Secretary for Health and Child Care Page | i Acknowledgements The Ministry of Health and Child Care (MOHCC) would want to acknowledge effort from all individuals and organizations that contributed to the production of these estimates and projections. We are particularly grateful to the National AIDS Council (NAC) for funding the national and sub-national capacity building and report writing workshop. We are also grateful to the National HIV and AIDS Estimates Working Group for working tirelessly to produce this report. -

Grant Assistance for Grassroots Human Projects in Zimbabwe
Grant Assistance for Grassroots Human Projects in Zimbabwe Amount Amount No Year Project Title Implementing Organisation District (US) (yen) 1 1989 Mbungu Primary School Development Project Mbungu Primary School Gokwe 16,807 2,067,261 2 1989 Sewing and Knitting Project Rutowa Young Women's Club Gutu 5,434 668,382 3 1990 Children's Agricultural Project Save the Children USA Nyangombe 8,659 1,177,624 Mbungo Uniform Clothing Tailoring Workshop 4 1990 Mbungo Women's Club Masvingo 14,767 2,008,312 Project Construction of Gardening Facilities in 5 1991 Cold Comfort Farm Trust Harare 42,103 5,431,287 Support of Small-Scale Farmers 6 1991 Pre-School Project Kwayedza Cooperative Gweru 33,226 4,286,154 Committee for the Rural Technical 7 1992 Rural Technical Training Project Murehwa 38,266 4,936,314 Training Project 8 1992 Mukotosi Schools Project Mukotosi Project Committee Chivi 20,912 2,697,648 9 1992 Bvute Dam Project Bvute Dam Project Committee Chivi 3,558 458,982 10 1992 Uranda Clinic Project Uranda Clinic Project Committee Chivi 1,309 168,861 11 1992 Utete Dam Project Utete Dam Project Committee Chivi 8,051 1,038,579 Drilling of Ten Boreholes for Water and 12 1993 Irrigation in the Inyathi and Tsholotsho Help Age Zimbabwe Tsholotsho 41,574 5,072,028 PromotionDistricts of ofSocialForestry Matabeleland andManagement Zimbabwe National Conservation 13 1993 Buhera 46,682 5,695,204 ofWoodlands inCommunalAreas ofZimbabwe Trust Expansion of St. Mary's Gavhunga Primary St. Mary's Gavhunga Primary 14 1994 Kadoma 29,916 3,171,096 School School Tsitshatshawa