Kurt Benirschke in Memoriam
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Messages from the Placentae Across Multiple Species a 50 Years
Placenta 84 (2019) 14–27 Contents lists available at ScienceDirect Placenta journal homepage: www.elsevier.com/locate/placenta Messages from the placentae across multiple species: A 50 years exploration T Hiroaki Soma Saitama Medical University, Japan ARTICLE INFO ABSTRACT Keywords: This review explores eight aspects of placentation in multiple mammalian. Gestational trophoblastic disease 1) Specialities of gestational trophoblastic disease. SUA(Single umbilical artery) 2) Clinical significance of single umbilical artery (SUA) syndrome. DIC(Disseminated intravascular coagulation) in 3) Pulmonary trophoblast embolism in pregnant chinchillas and DIC in pregnant giant panda. giant panda 4) Genetics status and placental behaviors during Japanese serow and related antelopes. Placentation in Japanese serow 5) Specific living style and placentation of the Sloth and Proboscis monkey. Hydatidiform mole in chimpanzee Placentation in different living elephant 6) Similarities of placental structures between human and great apes. Manatee and hyrax 7) Similarities of placental forms in elephants, manatees and rock hyrax with different living styles. Specific placental findings of Himalayan people 8) Specialities of placental pathology in Himalayan mountain people. Conclusions: It was taught that every mammalian species held on placental forms applied to different environ- mental life for their infants, even though their gestational lengths were different. 1. Introduction of effective chemotherapeutic agents. In 1959, I was fortunate tore- ceive an invitation from Prof. Kurt Benirschke at the Boston Lying-in Last October, Scientific American published a special issue about a Hospital. Before that, I had written to Prof. Arthur T. Hertig, Chairman baby's first organ, the placenta [1]. It is full of surprises and amazing of Pathology, Harvard Medical School, asking to study human tropho- science. -
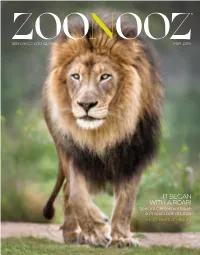
It Began with a Roar!
® ZOOSAN DIEGO ZOO GLOBAL N OOZ MAY 2016 IT BEGAN WITH A ROAR! Special Centennial Issue: A Proud Look at Lions + 100 Years of History WITH A MOTHER’S DAY BUFFET AT THE ZOO AND SAFARI PARK THIS YEAR SUNDAY, MAY 8, 2016 CONTINUOUS SEATING BEGINS AT 11 A.M. SEATINGS AT 10 A.M. AND 1 P.M. Enjoy the casual elegance of our Treetops Celebrate Mother’s Day at the San Diego Zoo Banquet Room as you make selections from our Safari Park with a delicious spring brunch. endless omelet bar, or choose from many generous Guests will be seated at their own reserved table, entrée choices and delectable desserts. set according to their guest count. $44.95 for adults; $18.95 for children ages 3 to 11, $44.95 for adults; $18.95 for children plus tax and gratuity. Nonmembers add Zoo admission. ages 3 to 11, plus tax and parking. For reservations, please call 619-557-3964 Nonmembers add Safari Park admission. between 10 a.m. and 4 p.m. daily. Secure your For reservations, call 619-718-3000, reservation with a credit card. or book online. May 2016 VOL. LXXXIX–NO. 03 Nooz Notes 2 Chairman’s Note; President’s Note; Save the Date; Centennial; What’s In Store; It’s Only a Number Graphically Speaking 8 Lions Revealed Discover the magnificent lion. BY AMY BLANDFORD AND WENDY PERKINS Cover Story 10 The Life of Lion What sets the “king of beasts” apart from other big cat species? A lion’s share of unique attributes, both physical and behavioral. -
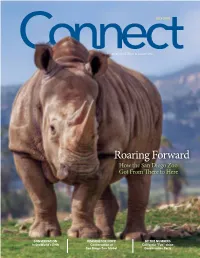
Roaring Forward How the San Diego Zoo Got from There to Here
JULY 2016 A publication of the Association of Zoos & Aquariums Roaring Forward How the San Diego Zoo Got From There to Here CONSERVATION REASON FOR HOPE BY THE NUMBERS In SeaWorld’s DNA Conservation at California “Fun”-shine San Diego Zoo Global Conservation Facts July 2016 Features 20 26 34 ROARING FORWARD CONSERVATION REASONS FOR HOPE How the San Diego Zoo In Seaworld’s DNA Conservation at San Got from There to Here SeaWorld’s commitment to Diego Zoo Global 100 years of trials and conservation was a guiding As a conservation triumphs, innovation and principle of its founders organization, San Diego Zoo vision, extraordinary people more than 50 years ago. This Global is committed to saving and amazing animals, came commitment is stronger today species worldwide by uniting together to build San Diego than ever before. Through its expertise in animal care Zoo Global. The roar has its conservation efforts and and conservation science with been an important part of important research conducted its dedication to inspiring a the Zoo’s history ever since with the animals in its care, passion for nature. Each of those early days, a symbol of and by inspiring millions of its conservation projects is a “roaring forward” to conserve guests every year, SeaWorld collaborative effort, and the endangered species in will continue to deliver on its strength and effectiveness of habitats worldwide. promise to help conserve the conservation programs comes world we all share. BY KAREN WORLEY from these partnerships and BY DAVID KOONTZ their supporters. -

The San Diego Zoo After 100 Years
The San Diego Zoo After 100 Years Sarah Matteson Defying the Odds The nucleus that evolved into the San Diego Zoo lay in the display of animals at the Panama-California Exposition held in 1915- 1916. So popular did the Exposition become, it carried on for a second year, added the word international, and included an array of animals for viewing along “the Isthmus”— the fair’s fun zone. Thirty-two cages placed © along what is today Park Boulevard, opposite the exposition’s Painted Desert attraction, housed the original assortment of animals—kangaroos, bears, buffalos, lions, leopards, hyenas, wolves, baboons, monkeys, parrots, and cockatoos, to name a few.1 Some of these animals were on loan from Wonderland Amusement Park, but other animal collections dotted the park.2 By the time the Exposition closed on December 31, 1916, Wonderland had closed and the animals were in need of a new home and caretaker. The spark that set into motion the San Diego Zoo as a separate entity has become an almost mythical origin story. In short, it is said that the San Diego Zoo “began with a roar”—a local doctor and his brother were driving past the animal cages when they heard a lion roar. The man, Dr. Harry Wegeforth, thought to Sarah Matteson, a graduate of the University of California Los Angeles with BAs in History and Political Science, is the Education Coordinator at the San Diego History Center where she develops programming for varied audiences. She helped develop interactive elements and provided interpretation for the History Center’s exhibit for the San Diego Zoo centennial “The Lore Behind the Roar.” 105 The Journal of San Diego History himself that San Diego ought to keep these animals for a zoo. -

Scientific Papers of Kurt Benirschke
Scientific Papers of Kurt Benirschke Books 1. Benirschke K, Driscoll SG (1967) The pathology of the placenta. In: Henke-Lubarsch (ed) Handb path Anat, Vol VII/5. Springer, Berlin Heidelberg New York, p 500 2. Benirschke K (1967) Comparative aspects of reproductive failure. Conference held in Hanover, NH, July 1966, Springer, Berlin Heidelberg New York 3. Hsu TC, Benirschke K (1967) Mammalian chromosome atlas, VolI. Springer, Berlin Heidelberg New York 4. Hsu TC, Benirschke K (1968) Mammalian chromosome atlas, Vol II. Springer, Berlin Heidelberg New York 5. Hsu TC, Benirschke K (1969) Mammalian chromosome atlas, VolIIl. Springer, Berlin Heidelberg New York 6. Benirschke K (1969) Comparative aspects of mammalian cytogenetics. Conference held in Hanover, NH, July 1968. Springer, Berlin Heidelberg New York 7. Hsu TC, Benirschke K (1970) Mammalian chromosome atlas, VolIV. Springer, Berlin Heidelberg New York 8. Hsu TC, Benirschke K (1971) Mammalian chromosome atlas, VolVo Springer, Berlin Heidelberg New York 9. Hsu TC, Benirschke K (1971) Mammalian chromosome atlas, Vol VI. Springer, Berlin Heidelberg New York 10. Benirschke K (coeditor) (1972) Chromosome atlas: Fish, amphibians, birds, reptiles, Vol I. Springer, Berlin Heidelberg New York 11. Reid DE, Ryan KJ, Benirschke K (1972) Principles and management of human repro duction. Saunders, Philadelphia 12. Hsu TC, Benirschke K (1973) Mammalian chromosome atlas, Vol VII. Springer, Ber lin Heidelberg New York 13. Benirschke K (1974) The pathology of the human placenta. Medcom, New York 14. Benirschke K (coeditor) (1974) Chromosome atlas: Fish, amphibians, birds, reptiles, Vol II. Springer, Berlin Heidelberg New York 15. Hsu TC, Benirschke K (1974) Mammalian chromosome atlas, Vol VIII. -

Little-Known Asian Animals with a Promising Economic Future
This PDF is available from The National Academies Press at http://www.nap.edu/catalog.php?record_id=19514 Little-Known Asian Animals With a Promising Economic Future: (1983) Pages Advisory Committee on Technology Innovation; Board 150 on Science and Technology for International Size Development; Office of International Affairs; National 5 x 9 Research Council ISBN 0309327156 Find Similar Titles More Information Visit the National Academies Press online and register for... Instant access to free PDF downloads of titles from the NATIONAL ACADEMY OF SCIENCES NATIONAL ACADEMY OF ENGINEERING INSTITUTE OF MEDICINE NATIONAL RESEARCH COUNCIL 10% off print titles Custom notification of new releases in your field of interest Special offers and discounts FROM THE ARCHIVES Distribution, posting, or copying of this PDF is strictly prohibited without written permission of the National Academies Press. Unless otherwise indicated, all materials in this PDF are copyrighted by the National Academy of Sciences. To request permission to reprint or otherwise distribute portions of this publication contact our Customer Service Department at 800-624-6242. Copyright © National Academy of Sciences. All rights reserved. Little-Known Asian Animals With a Promising Economic Future: http://www.nap.edu/catalog.php?record_id=19514 � liQMj �ationa[ Acadt"!_� Press The National Academy Press was created by the National Academy of Sciences to publish the reports issued by the Academy and by the National Academy of Engineering, the Institute of Medicine, and the National Research Council, all operating under the charter granted to the National Academy of Sciences by the Congress of the United States. The cover silhouettes first appeared in 19S3 in Hoofed Mammals of the World by Ugo Mochi and T. -

Reminiscences of Kurt Benirschke on His Career
International Journal of Gynecological Pathology 21:289–300, Lippincott Williams & Wilkins, Baltimore © 2002 International Society of Gynecological Pathologists Special Article Placentas, Peccaries, and Pathologists: Reminiscences of Kurt Benirschke on his Career An Interview with Rebecca N. Baergen Dr. Baergen: Where did you grow up and what was Force. We were sent to the northeastern front, East Prus- your childhood like? sia, and then to what is now Alsace Lorraine and even- Dr. Benirschke: I was born on May 26, 1924 in tually to the Battle of the Bulge. That’s where I con- Glueckstadt, north of Hamburg, where the Holstein cows tracted acute hepatitis. I was sent to the hospital and was come from. I grew up there, in this very small town of supposed to go back to the front but I contracted diph- about 5000 people. It was a farming community—one theria. There was no more anti-serum in Germany so I doctor in town, one dentist—and my father was em- was given sulfonamides, which didn’t jive with my liver ployed as an organic chemist in a large paper factory. He too well, and so I was again in the hospital. When the war originally came from what is now the Czech republic and was over, the hospital closed and I just went home. I was had finished his chemical degree in East Prussia, which discharged later on by the British Army, which occupied is now part of Russia. I had a wonderful childhood with that area. I was able to go back to medical school in my two sisters and comfortable surroundings. -

Elephant Notes and News Joann M
Elephant Volume 2 | Issue 4 Article 28 1-1-2000 Elephant Notes and News Joann M. Holden Eleanor C. Marsac Faye D. Rosser Jeheskel Shoshani Sandra L. Shoshani Follow this and additional works at: https://digitalcommons.wayne.edu/elephant Recommended Citation Holden, J. M., Marsac, E. C., Rosser, F. D., Shoshani, J., & Shoshani, S. L. (2000). Elephant Notes and News. Elephant, 2(4), 87-106. Doi: 10.22237/elephant/1521732272 This Elephant Notes and News is brought to you for free and open access by the Open Access Journals at DigitalCommons@WayneState. It has been accepted for inclusion in Elephant by an authorized editor of DigitalCommons@WayneState. January 2000 Holden et al. - Elephant Notes and News 87 much less during this period and spend a lot of time walking in Elephant. Volume 2, Number 4, pages 87-107 search of females. Musth bulls have a peculiar gait known as the Copyright © 2000 Elephant Research Foundation ‘musth walk’, characterized by them holding their heads up high and swinging them from side to side. With all this extra activity their body condition deteriorates and eventually they fall out of Elephant Notes and News musth, whereupon they go back to their sedate life with the other boys [Charles Foley], compiled by Joann M. Holden, Eleanor C. Marsac, Faye D. Rosser, Jeheskel Shoshani, and Sandra L. Shoshani Q. What is the typical home range of an elephant group? Does it vary with season, food abundance, competitive groups, human Full Contents on page iii disturbance, or group size? What’s the farthest distance a group might cover while migrating? Abbreviations: Below are abbreviations used in this and other sections A. -

Curriculum Vitae OLIVER A. RYDER, Ph.D
Curriculum Vitae OLIVER A. RYDER, Ph.D. * * * PERSONAL DATA Place of Birth: Alexandria, Virginia Business Address: San Diego Zoo Institute for Conservation Research 15600 San Pasqual Valley Road, Escondido, CA 92027-7000 Business Telephone: (760) 291.5452 Business Facsimile: (760) 796.5631 E-mail Address: [email protected] Web Pages: http://www.sandiegozoo.org/ www.biology.ucsd.edu/faculty/ryder.html EDUCATIONAL BACKGROUND 1968-75 University of California, San Diego: Ph.D. in Biology 1964-68 University of California, Riverside: B.A. in Biology with High Honors CURRENT PROFESSION Director of Genetics, Kleberg Chair; San Diego Zoo’s Institute for Conservation Research; San Diego, CA Adjunct Professor of Biology; Department of Biology, University of California, San Diego; La Jolla, CA Adjunct Professor of Biology; Department of Biology, San Diego State University Visiting Scholar; Center for Conservation Biology, University of California, Riverside; Riverside, CA PROFESSIONAL BACKGROUND 2009- Adjunct Professor of Biology; Department of Biology, San Diego State University 2007- Visiting Scholar; Center for Conservation Biology, University of California, Riverside; Riverside, CA 1995- Adjunct Professor of Biology; Department of Biology, University of California, San Diego; La Jolla, CA 1986- Director of Genetics, Kleberg Chair; San Diego Zoo’s Institute for Conservation Research; San Diego, CA 1988-95 Adjunct Associate Professor of Biology; Department of Biology, University of California, San Diego; La Jolla, CA 1979-87 Research Associate; Department -
![Kurt Benirschke (1924-) [1]](https://docslib.b-cdn.net/cover/0830/kurt-benirschke-1924-1-4190830.webp)
Kurt Benirschke (1924-) [1]
Published on The Embryo Project Encyclopedia (https://embryo.asu.edu) Kurt Benirschke (1924-) [1] By: Love, Karen Keywords: Frozen Zoo [2] Kurt Benirschke studied cells, placentas, and endangered species in Germany and the US during the twentieth century. Benirschke was professor at the University of California in San Diego, California, and a director of the research department at the San Diego Zoo in San Diego, California. He also helped form the research department of the San Diego Zoo and its sister organization [3], the Center for Reproduction of Endangered Species. Benirschke contributed to the field ofe mbryology [4] through his work on human and animal reproduction, including work on human placentas and birth defects [5], through work on the structure of chromosomes, and through work on the reproduction and conservation of endangered species. Kurt Benirschke was born 26 May 1924 in Glückstadt, Germany, to Marie Luebcke and Fritz Benirschke. In 1948, he received his medical degree from the University of Hamburg [6] in Hamburg, Germany. He studied English in London, England, before moving to the United States in 1949 in search of work as a physician. Prior to accepting an internship in 1950 at the Holy Name Hospital in Teaneck, New Jersey, he delivered German newspapers with his cousin to receive an income. Benirschke met Marion Elizabeth Waldhausen, a nurse, in Teaneck. They married and had three children, Rolf Joachim, Stephen Kurt, and Ingrid Marie. Though Benirschke encouraged Rolf to pursue medical studies, Rolf played professional football. Stephen became an orthopedic surgeon, while Ingrid Marie became a marketer. In 1955, Benirschke became a pathology resident at Harvard Medical School [7] in Boston, Massachusetts. -

It Began with a Roar 100 Years of History at the San Diego Zoo
It Began with a Roar 100 Years of History at the San Diego Zoo Teacher Resources & Activities GRADES 3 TO 6 Taku | Polar Bear First polar bear born at the Zoo, 1942 1 © ZSSD 2017 © ZSSD Table of Contents Welcome from Zookeeper Rick Schwartz 2 Biographies of Four Zoo Leaders 4 Profiles of Historic Animals 6 Activities What Would You Do? (Grade 3) 9 Healthy Homes (Grade 3) 13 A History of Great Leaders (Grade 4) 17 Shining Animal Stars (Grade 4) 18 Surviving in Slim Times (Grade 5) 20 You Belong at the Zoo! (Grade 6) 22 Read All About It (Grades 3-6) 26 Resources 27 Glossary 27 Connection to Common Core Standards 28 The activities in this booklet follow the 5E Instructional Model developed through the Biological Sciences Curriculum Study (BSCS). The phases of the BSCS 5E-teaching sequence are Engage, Explore, Explain, Elaborate, and Evaluate. Generally, activity steps 1 through about these 5 align with these phases, and activities match to a grade level. However, activities can be adapted to any grade to complement activities in-classroom curriculum. Like this activity guide? Go to sandiegozoo.org/tearchersurvey for a quick, online feedback form. We appreciate your comments. First polar bear born at the Zoo, 1942 1 © ZSSD 2017 © ZSSD Welcome From Zookeeper Rick Schwartz Happy Birthday, San Diego Zoo! The San Diego Zoo celebrated its 100th birthday in 2016, and, boy, what a year we had! I was lucky enough to be at many events, helping to greet Zoo visitors and tell them all about the Zoo’s fascinating history. -

2008-2009000 080 8-208 2 000 090 9 October 2009
SAN DIEGO NATURAL HISTORY MUSEUM 2008-2009000 080 8-208 2 000 090 9 October 2009 Dear Museum Friends: This year’s Annual Report ushers in another milestone for the San Diego Natural History Museum—the start of our 135th anniversary. We enter this landmark year on the heels of presenting what I believe are some of the most educational exhibitions we have ever offered. Water: A California Story and Water: H20 = Life could not have been more timely as we enter into mandatory water rationing. We closed the fi scal year with Gunther von Hagens’ BODY WORLDS & The Brain— Our Three Pound Gem. This groundbreaking exhibition had 300,000 visitors and reached an unprecedented number of students with its outreach and programming. As importantly, as we move into the anniversary year, we refl ect on the theme from our successful capital campaign, Full Circle, which referred to the Museum’s return to its original mission and vision as a repository and research organization focused on our amazing region. Our fi rst comprehensive strategic planning process, initiated in 1991, led us back to the motivation for our founding: a fascination by early San Diegans with the extraordinary biodiversity of the southern California and Baja California region. It is worthwhile to refl ect on the past year’s accomplishments and on how our mission has consistently guided our efforts in research, education, and exhibitions. The Biodiversity Research Center of the Californias’ contribution to the Annual Report focuses on an exciting centennial project in the San Jacinto mountains. This expedition unites each of our research disciplines as we revisit pioneering work done 100 years ago, collect new data and compare changes.