Ischemic Colitis: Surging Waves of Update
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Twisted Bowels: Intestinal Obstruction Blake Briggs, MD Mechanical
Twisted Bowels: Intestinal obstruction Blake Briggs, MD Objectives: define bowel obstructions and their types, pathophysiology, causes, presenting signs/symptoms, diagnosis, and treatment options, as well as the complications associated with them. Bowel Obstruction: the prevention of the normal digestive process as well as intestinal motility. 2 overarching categories: Mechanical obstruction: More common. physical blockage of the GI tract. Can be complete or incomplete. Complete obstruction typically is more severe and more likely requires surgical intervention. Functional obstruction: diffuse loss of intestinal motility and digestion throughout the intestine (e.g. failure of peristalsis). 2 possible locations: Small bowel: more common Large bowel All bowel obstructions have the potential risk of progressing to complete obstruction Mechanical obstruction Pathophysiology Mechanical blockage of flow à dilation of bowel proximal to obstruction à distal bowel is flattened/compressed à Bacteria and swallowed air add to the proximal dilation à loss of intestinal absorptive capacity and progressive loss of fluid across intestinal wall à dehydration and increasing electrolyte abnormalities à emesis with excessive loss of Na, K, H, and Cl à further dilation leads to compression of blood supply à intestinal segment ischemia and resultant necrosis. Signs/Symptoms: The goal of the physical exam in this case is to rule out signs of peritonitis (e.g. ruptured bowel). Colicky abdominal pain Bloating and distention: distention is worse in distal bowel obstruction. Hyperresonance on percussion. Nausea and vomiting: N/V is worse in proximal obstruction. Excessive emesis leads to hyponatremic, hypochloremic metabolic alkalosis with hypokalemia. Dehydration from emesis and fluid shifts results in dry mucus membranes and oliguria Obstipation: severe constipation or complete lack of bowel movements. -

Jejunoileal Diverticulitis: Big Trouble in Small Bowel
Jejunoileal Diverticulitis: Big Trouble in Small Bowel MICHAEL CARUSO DO, HAO LO MD EMERGENCY RADIOLOGY, UMASS MEMORIAL MEDICAL CENTER, WORCESTER, MA LEARNING OBJECTIVES: After excluding Meckel’s diverticulum, less than 30% of reported diverticula occurred in the CASE 1 1. Be aware of the relatively rare diagnoses of jejunoileal jejunum and ileum. HISTORY: 52 year old female with left upper quadrant pain. diverticulosis (non-Meckelian) and diverticulitis. Duodenal diverticula are approximately five times more common than jejunoileal diverticula. FINDINGS: 2.2 cm diverticulum extending from the distal ileum with adjacent induration of the mesenteric fat, consistent with an ileal diverticulitis. 2. Learn the epidemiology, pathophysiology, imaging findings and differential diagnosis of jejunoileal diverticulitis. Diverticulaare sac-like protrusions of the bowel wall, which may be composed of mucosa and submucosa only (pseudodiverticula) or of all CT Findings (2) layers of the bowel wall (true . Usually presents as a focal area of bowel wall thickening most prominent on the mesenteric side of AXIAL AXIAL CORONAL diverticula) the bowel with adjacent inflammation and/or abscess formation . Diverticulitis is the result of When abscess is present, CT findings may include relatively smooth margins, areas of low CASE 2 obstruction of the neck of the attenuation within the mass, rim enhancement after IV contrast administration, gas within the HISTORY: 62 year old female with epigastric and left upper quadrant pain. diverticulum, with subsequent mass, displacement of the surrounding structures, and edema of thickening of the surrounding fat inflammation, perforation and or fascial planes FINDINGS: 4.7 cm diameter out pouching seen arising from the proximal small bowel and associated with adjacent inflammatory stranding. -

Coping with the Problems of Diagnosis of Acute Colitis
Diagnostic and Interventional Imaging (2013) 94, 793—804 . CONTINUING EDUCATION PROGRAM: FOCUS . Coping with the problems of diagnosis of acute colitis a,∗,c b a E. Delabrousse , F. Ferreira , N. Badet , a b M. Martin , M. Zins a Urinogenital and Digestive Imaging Department, hôpital Jean-Minjoz, CHRU de Besanc¸on, 3, boulevard Fleming, 25030 Besanc¸on, France b Radiology Department, hôpital Saint-Joseph, 184, rue Raymond-Losserand, 75014 Paris, France c EA 4662, Nanomedicine Laboratory, Imagery and Therapeutics, University of Franche-Comté, Besanc¸on, France KEYWORDS Abstract Acute colitis is an acute condition of the colon. For the radiologist, it is mainly Colitis; diagnosed during differential diagnosis of acute abdominal conditions. There are many causes Ischaemia; of colitis and the degree of its severity varies. A CT scan is the best imaging examination for IBD; diagnosing it and also for analysing and characterising colitis. The topography, type of lesion Pseudomembranous; and associated factors can often suggest a precise diagnosis but it is nevertheless essential to Neutropenia integrate these findings into the clinical context and take laboratory values into account. The use of endoscopy is still the rule where a doubt remains, or to obtain necessary histological evidence. © 2013 Éditions françaises de radiologie. Published by Elsevier Masson SAS. All rights reserved. Acute colitis is an acute condition of the colon and most often presents in the form of an acute abdominal picture with very variable clinical symptoms and laboratory test results. The most frequent symptoms encountered in colitis are abdominal pain, fever and diarrhoea [1]. Hyperleucocytosis and elevated CRP in laboratory tests are common. -
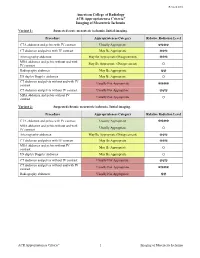
ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia Variant 1: Suspected acute mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ MRA abdomen and pelvis without and with May Be Appropriate (Disagreement) IV contrast O Radiography abdomen May Be Appropriate ☢☢ US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ MRA abdomen and pelvis without IV Usually Not Appropriate contrast O Variant 2: Suspected chronic mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ MRA abdomen and pelvis without and with Usually Appropriate IV contrast O Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ MRA abdomen and pelvis without IV May Be Appropriate contrast O US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ Radiography abdomen Usually Not Appropriate ☢☢ ACR Appropriateness Criteria® 1 Imaging of Mesenteric Ischemia IMAGING OF MESENTERIC ISCHEMIA Expert Panels on Vascular Imaging and Gastrointestinal Imaging: Michael Ginsburg, MDa; Piotr Obara, MDb; Drew L. Lambert, MDc; Michael Hanley, MDd; Michael L. Steigner, MDe; Marc A. Camacho, MD, MSf; Ankur Chandra, MDg; Kevin J. Chang, MDh; Kenneth L. -

Small Bowel Infarction by Aspergillus
short report Haematologica 1997; 82:182-183 SMALL BOWEL INFARCTION BY ASPERGILLUS LUCIO CATALANO, MARCO PICARDI, DARIO ANZIVINO,* LUIGI INSABATO,° ROSARIO NOTARO, BRUNO ROTOLI Cattedre di Ematologia, *Microbiologia e °Anatomia Patologica, Università Federico II, Naples, Italy ABSTRACT Primary gut involvement by Aspergillus is a rare for small bowel perforation. The patient died a and often fatal complication of intensive anti- week later in spite of amphotericin-B treatment leukemic therapy. We describe the case of an adult and neutrophil recovery. Anti-Aspergillus prophy- patient affected by acute leukemia who developed laxis and early introduction of amphotericin-B in a small bowel fungal thromboembolism without the treatment of febrile neutropenia is probably radiographic evidence of lung involvement during advisable in all cases of AML. the post-induction aplastic phase. The diagnosis ©1997, Ferrata Storti Foundation was made histologically at laparotomy performed Key words: Aspergillosis, small bowel, mycotic thromboembolism linical reports of gut involvement by revealed diffuse mycotic infiltration of the intestinal Aspergillus with arterial infarctions are rare.1-3 wall with fungal emboli obturating the lumen of CWe report on an adult male affected by a the superior mesenteric artery branches (Figures 1 favorable subtype of acute myeloid leukemia (AML and 2). Colonies of A. fumigatus grew from bowel M4-Eo) who succumbed to fatal intestinal asper- fragment cultures. Melena persisted despite neu- gillosis (IA) after effective induction treatment. trophil recovery (which was accelerated by adminis- tration of G-CSF at 300 µg/d for 7 days) and treat- Case report ment with 50 mg/d liposomal amphotericin, cho- AML, FAB M4-Eo with cytogenetic evidence of sen because the patient was in severe renal failure inv 16, was diagnosed in a 58-year-old male in (plasma creatinine 5 mg/dL). -

Colonic Ischemia 9/21/14, 9:02 PM
Colonic ischemia 9/21/14, 9:02 PM Official reprint from UpToDate® www.uptodate.com ©2014 UpToDate® Colonic ischemia Authors Section Editors Deputy Editor Peter Grubel, MD John F Eidt, MD Kathryn A Collins, MD, PhD, FACS J Thomas Lamont, MD Joseph L Mills, Sr, MD Martin Weiser, MD All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Aug 2014. | This topic last updated: Aug 25, 2014. INTRODUCTION — Intestinal ischemia is caused by a reduction in blood flow, which can be related to acute arterial occlusion (embolic, thrombotic), venous thrombosis, or hypoperfusion of the mesenteric vasculature causing nonocclusive ischemia. Colonic ischemia is the most frequent form of intestinal ischemia, most often affecting the elderly [1]. Approximately 15 percent of patients with colonic ischemia develop gangrene, the consequences of which can be life-threatening, making rapid diagnosis and treatment imperative. The remainder develops nongangrenous ischemia, which is usually transient and resolves without sequelae [2]. However, some of these patients will have a more prolonged course or develop long-term complications, such as stricture or chronic ischemic colitis. The diagnosis and treatment of patients can be challenging since colonic ischemia often occurs in patients who are debilitated and have multiple medical problems. The clinical features, diagnosis, and treatment of ischemia affecting the colon and rectum will be reviewed here. Acute and chronic intestinal ischemia of the small intestine are discussed separately. (See "Acute mesenteric ischemia" and "Chronic mesenteric ischemia".) BLOOD SUPPLY OF THE COLON — The circulation to the large intestine and rectum is derived from the superior mesenteric artery (SMA), inferior mesenteric artery (IMA), and internal iliac arteries (figure 1). -

An Ileal Duplication Cyst Manifested As an Ileocolic Intussusception in An
Turk J Gastroenterol 2014; 25 (Suppl.-1): 196-8 An ileal duplication cyst manifested as an ileocolic intussusception in an adult xxxxxxxxxxxxxxx Hyun-Soo Kim1, Ji-Youn Sung2, Won Seo Park3, Youn Wha Kim2 1Aerospace Medical Research Center, Republic of Korea Air Force, Chungcheongbuk-do, Republic of Korea 2Department of Pathology, Kyung Hee University Faculty of Medicine, Seoul, Republic of Korea 3Department of Surgery, Kyung Hee University Faculty of Medicine, Seoul, Republic of Korea ABSTRACT An enteric duplication cyst presenting as enterocolic intussusception is an exceptional clinical entity. We herein report a rare case of an ileal duplication cyst that manifested as an ileocolic intussusception. A 19-year-old woman was hospitalized due to right upper quadrant pain. Colonoscopy revealed a polypoid mass protruding into the co- lonic lumen. Ultrasonography demonstrated intussusception with a teardrop-shaped cystic mass at the tip. Com- puted tomography also showed ileocolic intussusception with a 2.5 cm-sized round cystic mass at the tip of intus- susceptum. Microscopically, the cystic wall consisted of a well-defined smooth muscle coat and heterotopic gastric mucosa, consistent with an enteric duplication cyst. This case highlights an ileal duplication cyst as an uncommon cause of adult ileocolic intussusception. To the best of our knowledge, this is the first case of enteric duplication cyst identified as a pathological lead point for enterocolic intussusception in an adult. Enteric duplication cysts should be included in the differential diagnosis of cystic-leading lesions for adult intussusceptions. Keywords: Enteric duplication cyst, enterocolic intussusception, adult Case Report Case INTRODUCTION of an ileal duplication cyst manifested as an ileocolic in- Intussusception occurs when a portion of the diges- tussusception in a young adult woman. -

Diagnosis of Acute Abdominal Pain in Older Patients COREY LYON, LCDR, MC, USN, U.S
Diagnosis of Acute Abdominal Pain in Older Patients COREY LYON, LCDR, MC, USN, U.S. Naval Hospital Sigonella, Sigonella, Italy DWAYNE C. CLARK, M.D., Fond du Lac Regional Clinic, Fond du Lac, Wisconsin Acute abdominal pain is a common presenting complaint in older patients. Presentation may differ from that of the younger patient and is often complicated by coexistent disease, delays in presentation, and physical and social barri- ers. The physical examination can be misleadingly benign, even with catastrophic conditions such as abdominal aortic aneurysm rupture and mesenteric ischemia. Changes that occur in the biliary system because of aging make older patients vulnerable to acute cholecystitis, the most common indication for surgery in this population. In older patients with appendicitis, the initial diagnosis is correct only one half of the time, and there are increased rates of perforation and mortality when compared with younger patients. Medication use, gallstones, and alcohol use increase the risk of pancreatitis, and advanced age is an indicator of poor prognosis for this disease. Diverticulitis is a common cause of abdominal pain in the older patient; in appropriately selected patients, it may be treated on an outpatient basis with oral antibiotics. Small and large bowel obstructions, usually caused by adhesive disease or malignancy, are more common in the aged and often require surgery. Morbidity and mortality among older patients presenting with acute abdominal pain are high, and these patients often require hospitalization with prompt surgical consultation. (Am Fam Physician 2006;74:1537-44. Copyright © 2006 American Academy of Family Physicians.) cute abdominal pain (generally sultation.2,11 In retrospective studies, more defined as pain of less than one than one half of older patients presenting week’s duration) is a common to the emergency department with acute presenting complaint among abdominal pain required hospital admission, Aolder patients. -

Delayed Diagnosis of Chronic Mesenteric Ischaemia Woon CYL, Tay KH, Tan SG
Case Report Singapore Med J 2007; 48(1) : e9 Delayed diagnosis of chronic mesenteric ischaemia Woon CYL, Tay KH, Tan SG ABSTRACT peptic ulcer disease and a 30-year smoking history. Chronic mesenteric ischaemia is a rare disease. He first presented with colicky pain in the right Patients typically present with a protracted hypochondrium and epigastrium. He was diagnosed course of vague abdominal symptoms and with acute cholecystitis and underwent open profound weight loss, leading to a delay in cholecystectomy. Recovery was uneventful. Over the diagnosis. If untreated, it progresses to following two years, he was admitted ten times for colicky bowel infarction, which has a poor prognosis. left hypochondriac and epigastric pain, often worse Once diagnosed, however, it can be easily postprandially, poor appetite, diarrhoea, and weight loss remedied via endovascular stenting or open of 13 kg. Abnormalities on blood investigations included surgery. Symptom reversal is prompt and mildly-elevated alkaline phosphatase, gamma glutamyl patients rapidly achieve premorbid habitus. transferase, serum amylase and urine amylase. Repeated We report a 58-year-old man in whom oesophagogastroduodenoscopies (OGDs), colonoscopies, the diagnosis was missed for two years, during barium studies, abdominal computed tomography (CT) which numerous investigations were performed. and magnetic resonance cholangiopancreatography The diagnosis was eventually revealed on scans were normal. He finally underwent a coeliac plexus angiography, and he was cured by mesenteric block for pain relief. bypass surgery. For patients with the triad of Two months later, he returned with similar abdominal chronic, unrelenting weight loss, sitophobia symptoms. Owing to his severely cachectic appearance (food fear) and postprandial abdominal pain, and the persistence of symptoms, the diagnosis of this condition must be considered, and actively CMI was entertained. -

Ischemic Colitis Complicating Major Vascular Surgery Scott R
Surg Clin N Am 87 (2007) 1099–1114 Ischemic Colitis Complicating Major Vascular Surgery Scott R. Steele, MD, FACS Department of Surgery, Madigan Army Medical Center, Fort Lewis, WA 98431, USA Ischemic colitis is a well-described complication of major vascular surgery, mostly following open abdominal aortic aneurysm (AAA) repair and endovascular aneurysm repair (EVAR), but also with aortoiliac surgery, aortic dissection, and thoracic aneurysm repair [1,2]. Although Boley and colleagues [3] described ischemia of the colon in 1963 as a revers- ible process secondary to vascular occlusion, the term was not coined until 1966, when Marston and colleagues [4] described its three stages of evolu- tion (transient ischemia, late ischemic stricture, and gangrene), along with the natural history of the disease. Furthermore, the development of colonic ischemia as a result of major vascular and aortic surgery has only been well described since the 1970s [5–9]. The original reports were scattered and mostly consisted of autopsy studies, depicting not only the high mortality associated with this condition but also, in retrospect, the relative lack of in- sight as to explanations for its onset and progression. Unfortunately, recent outcomes have not shown much improvement. Luckily, the overall inci- dence remains low, estimated at between 0.6% and 3.1%, with higher rates attributed to ruptured aneurysms, open repair, and emergent surgery [10]. Following the development of ischemic colitis, mortality has been reported to be as high as 67%, highlighting the need for rapidly identifying the com- mencement of symptoms and, perhaps more importantly, those patients at risk, in attempt to prevent its onset [10,11]. -

Ischemic Colitis in Five Points: an Update 2013 REVUE
revue systématique de la littérature Ischemic colitis in five points: an update 2013 Rania Hefaiedh*, Mériam Sabbah*, Rym Ennaifer*, Hayfa Romdhane*, Amine Attaoui**, Najet Bel Hadj*, Lassad Gharbi**, Mohamed Taher Khalfallah** *Department of Gastroenterology and Hepatology –Mongi Slim University Hospital – La Marsa Tunis, Tunisia **Department of Surgery - Mongi Slim University Hospital – La Marsa Tunis, Tunisia R. Hefaiedh, M. Sabbah, R. Ennaifer, H. Romdhane, A. Attaoui, N. R. Hefaiedh, M. Sabbah, R. Ennaifer, H. Romdhane, A. Attaoui, N. Bel Hadj, L. Gharbi, M. T. Khalfallah Bel Hadj, L. Gharbi, M. T. Khalfallah La colite ischémique en cinq points: mise à jour 2013 Ischemic colitis in five points: An update 2013 LA TUNISIE MEDICALE - 2014 ; Vol 92 (n°05) : 299-303 LA TUNISIE MEDICALE - 2014 ; Vol 92 (n°05) : 299-303 résumé summary Prérequis : La colite ischémique est la forme la plus commune de Background: Ischemic colitis is the most common form of l'ischémie intestinale. La présence de diarrhée et de rectorragies intestinal ischemia. The presence of diarrhea and mild lower doivent orienter le diagnostic. Bien que la biologie et l’imagerie gastrointestinal bleeding should guide the diagnosis. Although many puissent orienter le diagnostic, la coloscopie avec des biopsies laboratory tests and radiographic images may suggest the diagnosis, demeure le gold standard pour poser le diagnostic d'ischémie colique. colonic endoscopic with histological analysis of biopsies is the gold But : Le but de notre étude était de résumer en cinq points standard for identification of colonic ischemia. l’épidémiologie, les caractéristiques cliniques, l'approche diagnostic aim : The aim of this study was to resume in 5 points: the et la prise en charge de la colite ischémique. -

Serum Lactate Is a Poor Marker of Bowel Ischemia Following Angioembolization for Lower Gastrointestinal Bleeding
4 Correspondence Page 1 of 4 Serum lactate is a poor marker of bowel ischemia following angioembolization for lower gastrointestinal bleeding Lynn Soo Hoon Yeo1^, Jiayan Wee2, Kumaresh Venkatesan3 1Department of Anaesthesia, Khoo Teck Puat Hospital/Woodlands Health Campus, Singapore; 2Department of Anaesthesiology, Intensive Care and Pain Medicine, Tan Tock Seng Hospital, Singapore; 3Department of Anaesthesia, Khoo Teck Puat Hospital, Singapore Correspondence to: Lynn Soo Hoon Yeo. Department of Anaesthesia, Khoo Teck Puat Hospital/Woodlands Health Campus, 90 Yishun Central, Singapore 768828, Singapore. Email: [email protected]. Received: 17 April 2020; Accepted: 19 November 2020; Published: 30 December 2020. doi: 10.21037/dmr-20-51 View this article at: http://dx.doi.org/10.21037/dmr-20-51 In patients with suspected active bleeding from the (ED) with abdominal pain and per-rectal bleeding. His lower gastrointestinal tract, urgent angiography and abdomen was soft, tender over left lower quadrant with angioembolization of bleeding vessels is an accepted no generalized peritonism. Computed tomography (CT) management strategy (1). Technological advances in mesenteric angiogram performed showed active contrast interventional radiology have allowed endovascular extravasation in one of the hepatic flexure diverticula, treatment of lower gastrointestinal tract bleeding to be safer keeping with an acute bleed of the right colic artery. and more precise (2). Angioembolization of right colic artery was performed. A known complication after angioembolization of Serum lactate levels were trended routinely after the bleeding vessels is the development of ischemic bowel. The angioembolization procedure. Serum lactate levels remained incidence of ischemic bowel after angioembolization has low at 0.8 to 1.7 mmol/L, however, the patient developed been reported as 13% to 24% in different case series (3,4).